Back to Journals » International Journal of Women's Health » Volume 10
Adequacy of calcium intake during pregnancy in a tertiary care center
Authors Chotboon C , Soontrapa S, Buppasiri P, Muktabhant B , Kongwattanakul K, Thinkhamrop J
Received 12 March 2018
Accepted for publication 31 May 2018
Published 13 September 2018 Volume 2018:10 Pages 523—527
DOI https://doi.org/10.2147/IJWH.S167980
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Elie Al-Chaer
Chokchai Chotboon,1 Sukree Soontrapa,1 Pranom Buppasiri,1 Benja Muktabhant,2 Kiattisak Kongwattanakul,1 Jadsada Thinkhamrop1
1Department of Obstetrics and Gynecology, Faculty of Medicine, Khon Kaen University, Khon Kaen, Thailand; 2Faculty of Public Health, Research Group on Prevention and Control of Diabetes in the Northeast, Khon Kaen University, Khon Kaen, Thailand
Background: Calcium is an essential element for the body, which is taken through the dietary sources. Calcium supplements may be needed to achieve the dietary reference intake (DRI). Dietary calcium and supplemental calcium intake for calcium balance might be necessary. However, increasing evidence shows that calcium supplementation may enhance soft tissue calcification and cause cardiovascular diseases. Calcium requirement during pregnancy is markedly increased. If calcium supplementation depends on the dietary style of a region, then the adequacy of dietary calcium intake may guide the calcium supplementation.
Materials and methods: A cross-sectional descriptive study was conducted among pregnant women who attended prenatal care at Srinagarind Hospital, Khon Kaen University. We used semiquantitative food frequency questionnaire (SFFQ) to evaluate the amount of daily calcium intake, and 3 days food record to assess the SFFQ reliability. We used the INMUCAL-N V.3.0, based on the Thai food composition table for nutritional calculation.
Results: Among 255 recruited pregnant women, the mean daily dietary calcium intake was 1,256.9 mg/day (SD: 625.1) and up to 1,413.4 mg/day (SD: 601.3) in daily milk consumed group. Based on Thai DRI for pregnant women, with 800 mg/day as adequate intake of calcium, 74.9% had adequate calcium intake, and majority of them had milk daily.
Conclusion: The majority of pregnant women in a province of Northeast Thailand had adequate calcium intake, particularly those who had milk with their meal every day.
Keywords: calcium intake, pregnant women
Introduction
Calcium is an important mineral in many physiological processes. The most important function of calcium being bone composition and maintenance of normal cell processing, especially nerve and muscle cells. Calcium accumulation starts at fetal period and is higher during adolescent period.1 Calcium transportation is active from mother to fetus under placental regulation.2 Prevention of Hypertensive disorders and preeclampsia are the advantages of calcium supplementation during pregnancy, especially in low calcium-consumed population.3 Recommendation of daily calcium intake for women is 1,000–1,300 mg, depended on age.4 Thai dietary reference intake (DRI), in terms of adequate intake (AI) of calcium for pregnant women, is 800 mg/day and the international recommended dietary allowance of calcium is 1,000 mg/day.4,5
Adequate and appropriate calcium intake is very important. The excessive or inappropriate calcium intake might cause undesirable side effects, including lower iron absorption, constipation, flatulence, urinary stone, myocardial infarction, etc.6–8 However, an adequate calcium intake during pregnancy might prevent preterm birth, fetal growth restriction, increasing maternal bone mass, and reduce fracture risks.9–11
Dietary calcium consumption varies with geographic regions. Calcium intake is higher than the recommended daily requirement of each country in Europe and America. On the other hand, calcium intake is lower than the recommended daily requirement in Japan, New Zealand, India, Egypt, and Qatar.12–15
There are many studies on the dietary calcium intake among women in Thailand. Based on the data from South Thailand, calcium intake of pregnant women was lower than Thai recommended daily intake.16,17 While in the Northeast, calcium consumption among women was also found to be lower than the Thai DRI, there are no clear evidence specifically on pregnant women of the region.18 Therefore, it is required to study the dietary calcium intake among pregnant women in our setting to guide the calcium suggestion prescribed during pregnancy.
Materials and methods
Study of participants and design
A cross-sectional descriptive study was conducted among pregnant women who attended prenatal care at Srinagarind Hospital, Khon Kaen University, Khon Kaen Province, a tertiary care center in Northeast Thailand. The inclusion criteria were singleton pregnant women ≥20 years of age, ≥20 weeks of gestational age, and without any previous medical condition or pregnancy complications which limited certain kind of dietary intake. The sample size calculation was based on the result of Pongchaiyakul et al’s study.18 This research was approved by the Khon Kaen University Ethics Committee on Human Research (HE591446). After obtaining a written informed consent, all participants were interviewed for their daily dietary intake during the past 7 days to assess the amount of daily calcium intake.
Estimation of calcium intake
We used 73-item semiquantitative food frequency questionnaires (SFFQ) for calcium consumption assessment in studied women by asking them to recall types, amount, and frequency of food intake during the last 7 days. The first 30 participants, selected from one of every three subjects at the beginning of the recruitment, were asked to record everyday meal for 3 days in the food-record form, to validate the SFFQ.
There are two parts to the data collection: the first part was their general and pregnancy status, and the second part was semiquantitative food frequency questionnaire which consisted types of food and drink such as milk and its products, and common local foods.19 The trained assistant interviewed the women and recorded the forms. The 3-day food record is self-record maintained for all kinds and amount of food consumed for 3 days (two weekdays and one day of the weekend). We used the INMUCAL-N V.3.0, based on a Thai food composition database for calcium intake analysis. The frequency of consuming milk was classified as daily, often (4–6 days/week), sometimes (2–3 days/week), and occasionally (<2 days/week).
Statistical analysis
Stata V.10.0 was applied to analyze their general and pregnancy status. The amount of calcium intake was analyzed in terms of mean, SD, median, interquartile range, percentage, and 95% CI.
Results
Between January and September 2017, a total of 255 pregnant women were recruited to the study. Their mean age was 29.2±5.4 years, mean body mass index (BMI) was normal (21.8±4.0 kg/m2) and most of them were in their third trimester (gestational age’s mean 32.0±5.3 weeks). Almost half of them were primi-gravidity (46.3%) and worked as a government officer (45.9%) as demonstrated in Table 1.
  | Table 1 General and pregnancy characteristics of the studied women |
Comparing the energy and calcium consumption with 3 days food record validated the SFFQ. Among the first 30 pregnant women who recorded 3 days food every day, only 14 women (46.7%) had completed the form. The differences of energy and calcium consumption were 1.3% (95% CI: −1.0, 3.6), and 15.6% (95% CI: 9.0, 21.3), respectively.
The majority of pregnant women had cow’s milk daily (74.9%) and had soy milk at least once a week (74.5%). Only 6.3% of them had the food that reduced calcium absorption intake, such as tea, coffee, chocolate, and cocoa every day (Table 2).
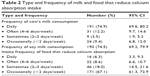  | Table 2 Type and frequency of milk and food that reduce calcium absorption intake |
The mean daily dietary calcium intake was 1,256.9 mg/day (SD: 625.1) and up to 1,413.4 (SD: 601.3) in daily milk consumed group. The mean calcium intake of the pregnant women who had milk intake less than 2 times/week was lower than Thai AI (800 mg/day).5 The mean calcium intake from food excluding all types of milk, revealed 404.8 mg/day (SD: 168.5). The mean of the volume of cow’s milk and soy milk intake were 255.8 (SD: 174.7) and 142.8 (SD: 153.1) mL/day, respectively.
Based on Thai AI of calcium (800 mg/day), 74.9% of pregnant women had adequate calcium intake. Whereas, based on international AI of calcium, 1,000 mg/day, only 61.6% of them consumed adequately. Majority of pregnant women with adequate calcium intake had milk in their meal daily. Meanwhile, according to Thai and international recommendation, by excluding milk in the daily diet, only 3.9% (95% CI: 2.0, 5.9) and 1.2% (95% CI: –0.8, 3.1), respectively, had an adequate calcium intake (Table 3).
  | Table 3 Amount of calcium intake and percentage of participants with adequate calcium intake, according to Thai AI |
We also demonstrated that among the sources of daily dietary calcium, the five main sources of calcium were from milk and its products, fishes, vegetables, and soy products when using mean. While, the median and the interquartile range were also displayed since the data did not distribute normally (Table 4).
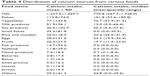  | Table 4 Distribution of calcium sources from various foods |
Discussion
The calcium requirement mainly depends on age.4,5 Women at reproductive age require adequate calcium intake, most importantly during pregnancy. In this study, 74.9% of pregnant women had cow’s milk, the main source of calcium in the daily diet, 74.5% of them had soy milk at least once a week as another source of calcium. Only 6.3% of them had food that reduced calcium absorption intake, such as tea, coffee, chocolate, and cocoa. The mean calcium consumption was 1,256.9 mg/day (SD: 625.1) and up to 1,413.4 mg/day (SD: 601.3) in daily milk consumed group. When excluding calcium sources from any type of milk, the mean daily calcium intake was only 404.8 mg/day (SD: 168.5). According to Thai AI, 800 mg/day of calcium is defined as adequate calcium intake for pregnant women of 19–50 years of age; hence the daily calcium intake in the study group would not be adequate if there was no milk in their daily meals.
Among the studied women, 74.9% had adequate calcium intake. This was similar to the study in America and Canada, United Kingdom, and Europe, with their mean daily calcium intake as 1,176, 933, and 1,141 mg/day, respectively.12 However, these results were different from studies in Japan, Australia, New Zealand, India, Egypt, Qatar, Saudi Arabia, Indonesia, and the South of Thailand in which the daily calcium intake was lower than their country’s AI.12–18 The main source of calcium was from milk (61.3% of daily dietary calcium source), possibly due to the awareness among pregnant women that calcium was important, which lead them to have milk daily during pregnancy, similar to the study in Brazil.20 To encourage adding milk in the daily diet during pregnancy would facilitate acceptability, adherence, and feasibility of calcium intake adequacy.21,22
There are many tools for nutritional assessment such as food frequency questionnaire and food record. The pros of food frequency questionnaire is its convenience and shows the overall food consuming pattern, but the cons are recall bias and likely shows a higher nutritional intake than food record. The food record, which may be recorded for 3, 7, or 14 days, is more accurate for the amount of food intake assessment, but less compliant and quite inconvenient for participants, particularly for longer period food record.23,24 This study found that only 46.7% of 3 days food records were completed for SFFQ validation.
Though we used SFFQ, and tried best to validate with 3 days food record, we found no clinically significant difference of energy and calcium consumption between SFFQ and 3 days food record (1.3% and 15.6% differences in records), as there was no change in results of adequacy of calcium intake.
Calcium prescription or encouragement to add milk in the daily diet during pregnancy should be considered if milk is not included in their daily meal. Also women should be advised to take iron supplements at different time, particularly in regions where iron deficiency is common. Further research trials should be encouraged to compare the calcium prescription or adding milk in the daily diet in terms of cost, convenience, satisfaction, and its adverse effects for pregnant women.
Conclusion
The majority of pregnant women in a province of Northeast Thailand had adequate calcium intake, particularly those who had milk in their meal every day.
Acknowledgments
We would like to thank the Department of Obstetrics and Gynecology, Faculty of Medicine, and Department of Nutrition, Faculty of Public Health, Khon Kaen University for their kind technical support for this work. Additionally, we are grateful for the financial support of the research fund of the Faculty of Medicine, Khon Kaen University, Khon Kaen, Thailand.
Disclosure
The authors report no conflicts of interest in this work.
References
Bringhurst FR, Demay MB, Krane SM, Kronenberg HM, editors. Bone and mineral metabolism in health and disease. In: Harrison’s Principles of Internal Medicine. 19th ed. New York: McGraw-Hill Education; 2015:2456–2458. | ||
Roberts V, Myatt L. uptodate® [homepage on the Internet]. Placental development and physiology; [cited August 19, 2016]. Available from: https://www.uptodate.com/contents/placental-development-and-physiology?search=placental-developmentandphysiology&source=search_result&selectedTitle=1~150&usage_type=default&display_rank=1 | ||
Hofmeyr GJ, Lawrie TA, Atallah ÁN, Duley L, Torloni MR. Calcium supplementation during pregnancy for preventing hypertensive disorders and related problems [review]. Cochrane Database Syst Rev. 2014;24(6):CD001059. | ||
Cunningham FG, Leveno KJ, Bloom SL, Spong CY, Dashe JS, Hoffman BL. Section 4: preconceptional and prenatal care. In: Williams Obstetrics. 24th ed. New York: McGraw-Hill Education; 2014:s179. | ||
Teinboon P. Vitamins–minerals supplementation & CRN pyramid. Thai J Parenter Enteral Nutr. 2006;17(2):72–85. | ||
Hallberg L, Rossander-Hultén L, Brune M, Gleerup A. Calcium and iron absorption: mechanism of action and nutritional importance. Eur J Clin Nutr. 1992;46(5):317–327. | ||
Reid IR, Bristow SM, Bolland MJ. Calcium supplements: benefits and risks. J Intern Med. 2015;278(4):354–368. | ||
Micromedexsolutions.com [homepage on Internet]. Calcium carbonate; [cited August 13, 2016]. Micromedex® Medication, Disease and Toxicology Management. Available from: http://www.micromedexsolutions.com/micromedex2/librarian/CS/3EC77F/ND_PR/evidencexpert/ND_P/evidencexpert/DUPLICATIONSHIELDSYNC/CD071A/ND_PG/evidencexpert/ND_B/evidencexpert/ND_AppProduct/evidencexpert/ND_T/evidencexpert/PFActionId/evidencexpert.DoIntegratedSearch?SearchTerm=Calcium%20carbonate&UserSearchTerm=Calcium%20carbonate&SearchFilter=filterNone&navitem=searchALL# | ||
Buppasiri P, Lumbiganon P, Thinkhamrop J, Ngamjarus C, Laopaiboon M, Medley N. Calcium supplementation (other than for preventing or treating hypertension) for improving pregnancy and infant outcomes [review]. Cochrane Database Syst Rev. 2015;25(2):CD007079. | ||
Tai V, Leung W, Grey A, Reid IR, Bolland MJ. Calcium intake and bone mineral density: systematic review and meta-analysis. BMJ. 2015;351:h4183. | ||
Bolland MJ, Leung W, Tai V, et al. Calcium intake and risk of fracture: systematic review. BMJ. 2015;351:h4580. | ||
Blumfield ML, Hure AJ, Macdonald-Wicks L, Smith R, Collins CE. A systematic review and meta-analysis of micronutrient intakes during pregnancy in developed countries. Nutr Rev. 2013;71(2):118–132. | ||
Gupta A, Kant S, Pandav CS, Gupta SK, Rai SK, Misra P. Dietary calcium intake, serum calcium level, and their association with preeclampsia in rural North India. Indian J Community Med. 2016;41(3):223–227. | ||
Darwish AM, Mohamad SN, Gamal Al-Din HR, Elsayed YA, Ahmad SI. Prevalence and predictors of deficient dietary calcium intake during the third trimester of pregnancy: the experience of a developing country. J Obstet Gynaecol Res. 2009;35(1):106–112. | ||
Hartriyanti Y, Suyoto PS, Muhammad HF, Palupi IR. Nutrient intake of pregnant women in Indonesia: a review. Mal J Nutr. 2012;18(1):113–124. | ||
Piammongkol S, Marks GC, Williams G, Chongsuvivatwong V. Food and nutrient consumption patterns in third trimester Thai-Muslim pregnant women in rural southern Thailand. Asia Pac J Clin Nutr. 2004;13(3):236–241. | ||
Sukchan P, Liabsuetrakul T, Chongsuvivatwong V, Songwathana P, Sornsrivichai V, Kuning M. Inadequacy of nutrients intake among pregnant women in the deep South of Thailand. BMC Public Health. 2010;10:572. | ||
Pongchaiyakul C, Charoenkiatkul S, Kosulwat V, Rojroongwasinkul N, Rajatanavin R. Dietary calcium intake among rural Thais in northeastern Thailand. J Med Assoc Thai. 2008;91(2):153–158. | ||
Sinawut S. Nutritive Values of Thai Foods. 1st ed. Nonthaburi: The War Veterans Organization of Thailand; 2001. | ||
Sato AP, Fujimori E, Szarfarc SC, Borges AL, Tsunechiro MA. Food consumption and iron intake of pregnant and reproductive aged women. Rev Lat Am Enfermagem. 2010;18(2):247–254. | ||
Omotayo MO, Dickin KL, O’Brien KO, Neufeld LM, Regil LMD, Stoltzfus RJ. Calcium supplementation to prevent preeclampsia: translating guidelines into practice in low-income countries. Adv Nutr. 2016;7(2):275–278. | ||
Omotayo MO, Dickin KL, Chapleau GM, et al. Cluster-randomized non-inferiority trial to compare supplement consumption and adherence to different dosing regimens for antenatal calcium and iron-folic acid supplementation to prevent preeclampsia and anaemia: rationale and design of the Micronutrient Initiative study. J Public Health Res. 2015;4(3):582. | ||
Wulandari H, Susetyowati, Prasanto H. Comparison between brief food frequency questionnaire and food record to assess the energy and protein intake of hemodialysis patients at Dr. Sardjito Hospital in Indonesia. Saudi J Kidney Dis Transpl. 2018;29(1):145–152. | ||
Takechi R, Alfonso H, Harrison A, et al. Assessing self-reported green tea and coffee consumption by food frequency questionnaire and food record and their association with polyphenol biomarkers in Japanese women. Asia Pac J Clin Nutr. 2018;27(2):460–465. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
