Back to Journals » Clinical Epidemiology » Volume 11
Access to palliative care for cancer patients between diagnosis and death: a national cohort study
Authors Janah A , Gauthier LR, Morin L , Bousquet PJ, Le Bihan C , Tuppin P , Peretti-Watel P, Bendiane MK
Received 25 February 2019
Accepted for publication 2 April 2019
Published 5 June 2019 Volume 2019:11 Pages 443—455
DOI https://doi.org/10.2147/CLEP.S198499
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Henrik Sørensen
Video abstract presented by Asmaa Janah
Views: 859
Asmaa Janah,1 Lynn R Gauthier,2 Lucas Morin,3 Philippe Jean Bousquet,1,4 Christine Le Bihan,4 Philippe Tuppin,5 Patrick Peretti-Watel,6 Marc-Karim Bendiane1
1Aix Marseille Univ, INSERM, IRD, Economics and Social Sciences Applied to Health & Analysis of Medical Information (SESSTIM), Marseille, France; 2Department of Family and Emergency Medicine, Faculty of Medicine, Université Laval - Centre Hospitalier Universitaire de Québec-Université Laval Research Centre, Oncology Division and Équipe de recherche Michel-Sarrazin en oncologie psychosociale et soins palliatifs, Université Laval Cancer Research Centre, Québec, Canada; 3Aging Research Center, Karolinska Institutet, Stockholm, Sweden; 4Survey, Monitoring and Assessment Department, Public Health and Healthcare Division, Institut National du Cancer (French National Cancer Institute - INCa), Boulogne Billancourt, France; 5Département des études sur les pathologies et les patients (DEPP), Caisse Nationale d’Assurance Maladie, Paris, France; 6Aix Marseille Univ, IRD, AP-HM, SSA, VITROME, IHU-Méditerranée Infection, and ORS PACA, Southeastern Health Regional Observatory, Marseille, France
Background and purpose: Introducing palliative care earlier in the disease trajectory has been found to provide better management of physical and psychological suffering. In France, the proportion of cancer patients who receive palliative care is unclear. This study aimed primarily to measure the prevalence of access to inpatient palliative care and associated patient-level factors, and to identify the time between access to palliative care and death.
Patients and methods: A nationwide retrospective cohort study using data from the French national health system database (SNDS). All those diagnosed with cancer in 2013 who died between 2013 and 2015 were included. Access to inpatient palliative care was the main outcome.
Results: Of the 313,059 patients diagnosed with cancer in 2013 in France, 72,315 (23%) died between 2013 and 2015. Overall, 57% had access to inpatient palliative care. The following groups were the most likely to have access to palliative care: women (adjusted odds ratio, aOR: 1.15; 95% CI: 1.11–1.20), people aged 18–49 (aOR: 1.38; 95% CI: 1.26–1.51), individuals with metastatic cancer (aOR: 2.04; 95% CI: 1.96–2.13), and patients with cancer of the nervous system (aOR: 1.80; 95% CI: 1.62–2.01). The median time between palliative care and death was 29 (interquartile range: 13–67) days.
Conclusion: More than half of cancer patients who died within 2 years after diagnosis had access to inpatient palliative care. Access to palliative care occurs late in the disease trajectory, often during the final month of life. Further research and guidelines are warranted to optimize access to early, standardized palliative care.
Keywords: French national health system database, palliative care, cancer, death, factors, timing
Introduction
According to the WHO, palliative care (PC) is a patient-centered approach which improves the quality of life of patients and their families facing problems associated with a life-threatening illness through the prevention and relief of suffering by means of early identification and efficient assessment and treatment of pain and other physical, psychosocial, and spiritual problems.1 Closely linked to the concept of supportive care, the latest model of PC focuses on patients’ quality of life and comfort.2–4 It takes their preferences into account, and encourages their involvement in decision-making processes.5,6
However, in France, as in most Southern European countries, the adoption of PC has been slower than in the United Kingdom or in Northern America.7 Clinical and structural resistance and barriers have hampered the implementation and development of this model of care for patients with serious illnesses, as evidenced by the distrust of either clinicians and patients regarding referral or access to PC.4,7,8 For the past 15 years, a succession of French government programs have been implemented to deal with the management of pain and support for patients with life-threatening illnesses, including cancer.9,10
International literature has shown that PC access may differ according to patients’ characteristics and that men, older people, patients with a low socioeconomic status, and those with hematological cancers are less likely to have access to PC.11–17 Besides, there is evidence that access to early integrated PC can improve patients quality of life and survival18–20 while reducing caregivers’ and health professionals’ psychological suffering.21,22 While not all patients need PC, all should have access to adequate symptom and psychological management when required. Patients with physical and/or psychosocial suffering must be referred to PC immediately irrespective of age or cancer stage.3,4,23 However, the literature shows that most of the time, access to PC occurs late in the disease trajectory,18,24–27 resulting in inadequate care. One of the major reasons for late access to PC is the common misconception that it cannot be provided in conjunction with curative treatments. Some practitioners are reluctant to refer patients to PC as they see referral as a reflection of their “failure” to successfully treat the patient. Linked to this is their fear that the patient’s circle of family and friends will also blame them for this “failure”.4,28–30
While several recent studies have estimated the proportion of patients receiving inpatient PC in France,31–33 to date, no study has investigated the impact of patient characteristics, such as age, gender, and cancer stage on access to this type of care. Accordingly, using a national database with full population coverage, we aimed to: 1) estimate the prevalence and characteristics of cancer patients admitted at least once to inpatient PC before death in the period 2013–2015; 2) calculate the time between PC access and death.
Material and methods
Study design
For this nationwide retrospective cohort study, we used data from the French National Cancer Cohort, which includes all people living in France with health insurance coverage (ie, nearly 100% of the French population) who are diagnosed with or treated for cancer. A detailed description of the methods can be found elsewhere.34 Briefly, this cohort is extracted from the French national health system database,35 and collects the following data since 2010: 1) all individual health care utilization reimbursement data (ie, hospitalization, outpatient care, medication expenditures) collected in a unique consumption database of the various national health insurance schemes (Données de Consommation Inter-Régimes database, DCIR); 2) private and public hospital database records, collected in the medical information system program (Programme de Médicalisation des Systèmes d’Information, PMSI) by the national agency for information on hospital care. The cohort is updated once a year by the French Health Insurance Scheme. New cases to be included are identified, and information on health care utilization during the year and the vital status of individuals already included is updated.
Data sources
The PMSI database, which is based on diagnosis-related groups (DRG), describes hospital stays and costs in acute care units (short stays – MCO), rehabilitation care units (SSR), hospital-at-home services (HAD), and psychiatric units. It contains demographic (age, sex, town/city, postcode, vital status at the end of hospital stay) and medical information including diagnoses and medical procedures using the same classification as in DCIR. They also contain data on consumption of expensive drugs and health care devices not included in the DRG pricing.
Study population (eligibility and exclusion criteria)
For the present analysis, the study population included all cancer patients diagnosed in 2013 who died between 2013 and 2015. The following inclusion criteria were adopted: 1) being entered as a new case in the cohort in 2013, 2) insured under the National General Insurance Scheme (ie, nearly 90% of the French population) as of the end of 2013, 3) not having a tumor with uncertain or unknown behavior (ie, whether malignant or benign), 4) receiving surgery, chemotherapy, hormone therapy, radiotherapy, PC, or other hospitalization for cancer in conventional medical units (short stays – MCO) in 2013. We excluded from the analysis individuals for whom the date of the first inpatient or outpatient treatment was missing, as it was not possible to calculate the interval between cancer diagnosis and death.
Outcomes measurement
Inpatient PC access was defined as the main outcome and was identified using the ICD-10 “PC” coding as primary diagnosis, related diagnosis, or significantly associated diagnosis. More specifically, inpatient PC stays were defined using: 1) the ICD-10 PC code for acute care units (Z51.5); 2) the French code for support in hospital-at-home services (=04); and 3) the ICD-10 PC code for rehabilitation care units (Z51.5). Stays in PC beds in acute care units (typically two or four beds to a room in hospital departments providing care for seriously ill patients) and admissions in PC inpatient units (ie, exclusively dedicated to providing specialist PC) were also considered.36 The study’s two secondary outcomes were the proximity of 1) cancer diagnosis and death and 2) initial access to inpatient PC and death. Accordingly, we calculated the following time intervals: between initial inpatient PC access and death, between cancer diagnosis and death, and between diagnosis and initial inpatient PC access.
Individual characteristics
We extracted personal and social characteristic data including birth and death dates, gender, zip code. We also extracted medical characteristics such as being registered as having a costly or long-term disease (LTD). LTD patients are entitled to 100% reimbursement. Cancer is an LTD whose diagnosis is coded according to the International Statistical Classification of Diseases and Related Health Problems-10th Revision (ICD-10). Moreover, data on outpatient health care utilization and costs were extracted, including date and nature of medical consultation and paramedical intervention, medication prescription and dates of delivery, lists of specific products and medical devices reimbursed, medical procedures, laboratory tests (without the results), medical transport, occupational accidents and illnesses, and finally disability.
Furthermore, cancer stages for included patients were identified using ICD-10 codes, since SNDS database does not provide clinical variables, such as the TNM (Tumour, Nodes, and Metastasis) cancer classification.34 Besides, comorbidities were identified on the basis of SNDS data. This was done using algorithms to distribute beneficiaries into 56 non-exclusive disease groups of chronic diseases, health events, and chronic treatments, assembled into 13 main categories.37,38 Additionally, to consider patients’ socioeconomic status, we used the French ecological deprivation index as a proxy (Fdep99).39
Statistical analysis
Two groups were identified from the extracted data: 1) individuals who had accessed inpatient PC at least once before death, and 2) individuals who had not. First, we compared the distribution of sociodemographic and medical characteristics between these two groups. Second, independent factors associated with PC access were identified by carrying out three multivariable logistic regressions while adjusting for inclusion characteristics. A first model was fitted for the overall population who had died between 2013 and 2015 only for cancer sites common to both men and women (11 sites). Two additional models were built separately for men and women, with cancer sites specific to each gender in each model. Finally, to explore the timing of PC in the disease trajectory, we computed three different time intervals between: 1) diagnosis and death, 2) diagnosis and PC access, and 3) PC access and death. The interval between PC and death was stratified by gender, age, site, and stage of cancer.
All the sections of this article were drawn up following recommendations in the REporting studies Conducted using Observational Routinely collected health Data (RECORD) statement.40 The French cancer cohort protocol was approved by a national committee (Comité Consultatif sur le Traitement de l’Information en Matière de Recherche dans le Domaine de la Santé, study registered under n°22/2011), and authorized by the French Data Protection Agency (Commission nationale de l’informatique et des libertés—Cnil, study registered under n°911297). Confidentiality in the cohort is guaranteed for all participants with regard to any personal information, as all data are pseudonymized.
Results
Proportion of PC access
Of the 313,059 patients diagnosed with cancer in 2013, 72,315 (23%) died between 2013 and 2015 (Figure 1). Among the latter, 40,941 (57%) had accessed inpatient PC at least once before death: 87% in short stays, 15% in homecare units, and 17% in rehabilitation care units. Median time between diagnosis and death for the entire died population was 208 days.
 | Figure 1 Selection of study population flowchart. |
Characteristics of patients who had accessed PC at least once
The median age of patients who had accessed PC at least once before death was 71. Half of them were aged 50–74 years in 2013 and 43% were women. As presented in Table 1, most patients who had access to PC before death had cancer localized in the gastrointestinal system (32%) (n=12, 996) or the respiratory system (23%) (n=9,419). Furthermore, 50% had a metastatic cancer (n=20,551). When considering each cancer site as a subpopulation, Figure 2 shows that after excluding breast, female and male genitals, multiple and non-attributable cancer sites, among deceased cancer patients, women accessed PC most frequently. More specifically, access to PC was more frequent in women than in men for several cancer sites: respiratory, gastrointestinal, and upper aerodigestive tract. Between 2013 and 2015, 52% of subjects who accessed PC underwent inpatient chemotherapy, 41% surgery for cancer and 34% at least one session of radiotherapy. This health care consumption was relatively lower among those without PC access(Figure 3).
 |  |  | Table 1 Sociodemographic and medical characteristics of cancer patients included in the French Cancer Cohort who died between 2013 and 2015 (N=72,315) |
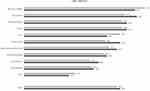 | Figure 2 Palliative care access for cancer patients included in the French Cancer Cohort who died between 2013 and 2015 by gender and according to each cancer site. |
 | Figure 3 Cancer-related health care consumption between 2013 and 2015 according to palliative care access. |
Factors associated with PC access
The results of the three multivariable logistic regressions are presented in Table 2. In the first multivariable model – carried out on the overall population yet limited to cancer sites common to both women and men – women, people aged 18–49, individuals with a metastatic cancer, patients a cancer of the nervous system, and those with a low deprivation index were all more likely to have accessed PC. In addition, patients residing in the two regions “Île-de-France” and “Auvergne-Rhône-Alpes” had the most frequent PC access. However, access was less likely for patients with two comorbidities or more. One of the important findings from the two gender-specific models is the impact of age on PC access: people over 75 were the least likely to have access to PC services, irrespective of gender.
 | Table 2 Factors independently associated with PC access. Multivariable logistic regressions |
Timing of PC access
Table 3 presents the number of days from cancer diagnosis to death, from diagnosis to PC access, and from initial PC access to death. Median time between 1) diagnosis and death, 2) diagnosis and initial PC access, and 3) initial PC access and death were 231, 144, and 29 days, respectively. Age- and gender-dependent differences regarding the time between PC access and death were observed. Men had a median of 28 days PC before death unlike women who had a longer median time (32 days). We found a linear relationship between age and timing of PC access. The median interval between PC access and death for cancer patients over 75 was 29 days, 30 days for patients aged between 50 and 74, 34 days for patients aged between 18 and 49, and 37.5 days for those under 18 years.
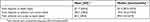 | Table 3 Time between initial palliative care access and death, cancer diagnosis and death, and diagnosis and palliative care access (N=40,941) |
Discussion
Main results
To the best of our knowledge, this is one of the few studies worldwide to explore the proportion of cancer patients with PC access before death in large population databases,15,41 to identify sociodemographic and clinical factors associated with this differentiated access and to examine the time between PC access and death. The findings revealed that more than half of the cancer patients included in the French cancer cohort who died between 2013 and 2015 had access to inpatient PC. However, access differed according to sociodemographic and medical characteristics. More specifically, women, younger patients, individuals with cancer of the nervous system, patients with a metastatic cancer, and those with fewer comorbidities, were the most likely populations to have access. Furthermore, we found substantial regional variations. With regard to the timing of PC, our results suggest that access to inpatient PC in France occurs late in the disease trajectory.
Proportion of PC access
Fifty-seven percent of our study population had accessed PC at least once before death, most of the times in acute care units. Our study is one of the few to explore PC prevalence in cancer patients in the French context. Poulalhon et al32 studied access to inpatient PC in people who died in France in 2013 based on their characteristics, for all pathologies and not only cancer. They reported that among the 347,253 individuals included in the study, 29% had access to PC (all diseases included) in the year before death and that this proportion reached 52% in cancer patients, a proportion that remains relatively lower than that reported in our study (57%). Two other studies exploring the use of end-of-life health care reported a PC access rate of 14.8% in the last month of life in patients with hematological malignancies31 and a rate reaching 78.4% during the last 3 months of life in patients with metastatic melanoma.33 In our study, PC access for those metastatic cancers reached 69%. Our result shows that the proportion of patients who had access to PC was relatively high compared with studies conducted in the United States and in the United Kingdom.11,12,42 Moreover, higher proportions than that reported in our study were found in three additional studies.15,16,43 In addition, in a study by Morin et al, the authors estimated – on the basis of the causes of death – that, between 41% and 69% of those who died required PC,44 this value being 62.2% in yet another study by Ravanello et al45. However, specific percentages for cancer patients are unclear.
Characteristics and factors associated with PC access
Previous studies have shown that PC access may differ according to patients’ characteristics and that men, older people, patients with a low socioeconomic status, and those with hematological cancers are the least likely to have access to PC.11–17 Our findings are consistent with those reported in these studies.
Age is a determining factor in PC access. Although older patients at the end of their lives may have greater needs than younger patients,44 studies have demonstrated that the latter are more likely to have access to PC.11,15,16,46 There are several possible explanations for this. First, it has been shown that older patients with cancer are the least informed about their diagnosis and prognosis, are less likely to discuss their preferences, especially in end-of-life situations, and may be more likely to accept the terminal nature of these situations, consequently expressing their desire for PC less often to their health care professional.47,48 Second, the higher incidence of comorbidities among older patients (eg, cardio-vascular diseases or neurodegenerative diseases), together with age-related deteriorations in functioning and related symptoms, may further complicate the management of both physical and psychological distress in this population. Accordingly, there is a greater likelihood of their accessing other hospital services (eg, cardiology) more frequently than PC services.49,50
With respect to gender, in line with several previous studies,12,16,46 women in the present study were more likely to have PC access than men. One study reported less PC access for men over 65 years of age.15 Our finding regarding the gender effect was expected given the higher estimated needs for PC in women than for men at the end of life,44 the active role that women play in decision-making processes when communicating with oncologists about their disease,51 and the fact that women prefer to access PC more than men.52
Our study revealed that patients with cancer of the nervous system were the most likely to access PC before death. This finding contrasts with that reported by Ziegler et al46 and may be explained by the highly symptomatic burden in patients with this type of cancer. Because these patients often have severe functional impairment as well as behavioral/cognitive dysfunction, and suffer from greater dependency and hopelessness, they are more likely to request PC.53 By contrast, patients with skin and hematological cancers in our study had significantly less PC access. For hematological cancers, for example, this finding is consistent with that reported by Hui et al11 and may be explained by the fact that these patients tend to access more frequently to hospital services other than PC services – including intensive units and emergency room visits – because of their needs (eg, transfusions).54,55
Cancer stage at diagnosis was also significantly associated with PC access, as patients with a node involvement or a metastatic cancer were most likely to have PC access. This was expected since these stages are associated with the worst prognosis and the highest rates of both physical and psychological morbidity.56,57
Timing of PC access
Several previous studies have reported that earlier access to PC in the disease trajectory is very effective as regards improving the management of various symptoms, including pain, minimizing aggressive cancer treatments, and especially enabling patients to make their own choices concerning end-of-life care.20,43,58 However, we reported a median of 29 days between PC access and death. This duration is considerably shorter than the optimal duration of 6 months reported in the literature20,58,59 but longer than that reported in at least one study.60 In addition, differences in the timing of PC were observed: older patients and men accessed PC later than younger patients and women. These results – especially that regarding the impact of age – are consistent with results reported in several studies.25,42,60,61
Strengths and limitations of the study
This is the largest cohort study conducted to assess inpatient PC access and its timing in cancer patients in France. The French cancer cohort is an exhaustive population-based cohort, including all citizens living in France irrespective of national insurance system or socioeconomic status. With more than 7 million individuals included between 2010 and 2015, the cohort is one of the largest cancer databases in the world. One strength of the present work is that it takes into account cancer only within a broader description of cancer sites, unlike a recent study on PC access in the French context.32 Moreover, unlike previous studies exploring predictors of PC access and/or its timing which included patients at an advanced cancer stage only,11,13,16,18–20,25,42,46 our study aimed to provide a comprehensive picture for policy and planning using a broader definition of PC which does not simply cover the final moments in life, but rather starts from the moment of cancer diagnosis and runs simultaneously with curative strategies, irrespective of patients’ age or cancer stage.3,4,62
The present study has limitations. Because the retrospective nature of the data collection and the lack of clinical variables in the SNDS, we were not able to explore the effect of access to PC services on the physical and psychological suffering of patients and families. Moreover, we focused on inpatient PC. Accordingly, with the exception of hospital-at-home services, we did not take into account outpatient PC occurring, for example, in accommodation facilities for dependent elderly people. One other reason for a probable underestimation of PC access is the possibility that some patients benefited from integrated PC (eg, symptom management) not coded as “PC”. Conversely, a likely overestimation of access to PC in our study could be related to probable inconsistencies in the coding of hospital stays in the PMSI database.
Another limitation is that the SNDS does not include data on the cause of death (at least at the time of the study). As comorbidities generally increase at the end of life, cancer may not be the only cause of death. To overcome this bias, we made a hypothesis about cancer mortality choosing the 2 years after diagnosis, as this is the period during which the majority of cancer-related deaths normally occur. Finally, it is important to bear in mind that our findings are based on a particular population (those who died within 2 years of diagnosis) and therefore cannot be generalized to those who survive longer.
Conclusions
The use of data from the French cancer cohort in this study allowed us to identify several patient characteristics as determinants of PC access. Further studies are recommended to better understand how these characteristics impact PC access, and especially to assess current needs of PC and its effects in cancer patients. This will help French policy-makers to ensure early, equitable, and individualized PC.
Acknowledgments
The authors of this study thank the Ligue contre le cancer charity for providing a doctoral fellowship to Asmaa Janah and the Caisse nationale d’assurance maladie des travailleurs salaries (Cnamts) for providing data. This study and the French cancer cohort are self-funded by the French National Cancer Institute. The funder of the study approved the study design, collected the data and participated in the analysis, and interpretation. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Author contributions
All authors contributed to data analysis, drafting or revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
1.
2. Cherny NI, Catane R, Kosmidis P. ESMO takes a stand on supportive and palliative care. Ann Oncol. 2003;14(9):1335–1337. doi:10.1093/annonc/mdg379
3. Ferrell BR, Temel JS, Temin S, et al. Integration of palliative care into standard oncology care: American Society of clinical oncology clinical practice guideline update. J Clin Oncol Off J Am Soc Clin Oncol. 2017;35(1):96–112. doi:10.1200/JCO.2016.70.1474
4. Hawley P. Barriers to access to palliative care. Palliat Care. 2017;10. doi:10.1177/1178224216688887.
5. Bélanger E, Rodríguez C, Groleau D, Légaré F, MacDonald ME, Marchand R. Patient participation in palliative care decisions: an ethnographic discourse analysis. Int J Qual Stud Health Well-Being. 2016;11. doi:10.3402/qhw.v11.32438.
6. Kaasa S, Loge JH, Aapro M, et al. Integration of oncology and palliative care: a lancet oncology commission. Lancet Oncol. 2018. doi:10.1016/S1470-2045(18)30415-7
7.
8. Sochor M, Sláma O, Loučka M. Early integration of palliative care into standard oncology care - benefits, limitations, barriers and types of palliative care. Klin Onkol Cas Ceske Slov Onkol Spolecnosti. 2015;28(3):171–176.
9.
10. Ministère des Solidarités et de la Santé. Le plan national “Soins Palliatifs 2015–2018”. Paris: Ministère des Solidarités et de la Santé; December 2016. Available from:
11. Hui D, Kim S-H, Kwon JH, et al. Access to palliative care among patients treated at a comprehensive cancer center. Oncologist. 2012;17(12):1574–1580. doi:10.1634/theoncologist.2012-0192
12. Fadul N, Elsayem A, Palmer JL, Zhang T, Braiteh F, Bruera E. Predictors of access to palliative care services among patients who died at a comprehensive cancer center. J Palliat Med. 2007;10(5):1146–1152. doi:10.1089/jpm.2006.0259
13. Tanco K, Hui D, Kim SH, et al. Predictors of palliative care (PC) referral for advanced cancer patients. J Clin Oncol. 2012;30(15_suppl):e19613–e19613. doi:10.1200/jco.2012.30.15_suppl.e19613
14. Maddison AR, Asada Y, Urquhart R. Inequity in access to cancer care: a review of the Canadian literature. Cancer Causes Control. 2011;22(3):359–366. doi:10.1007/s10552-010-9722-3
15. Burge FI, Lawson BJ, Johnston GM, Grunfeld E. A population-based study of age inequalities in access to palliative care among cancer patients. Med Care. 2008;46(12):1203–1211. doi:10.1097/MLR.0b013e31817d931d
16. Valentino TCDO, Paiva BSR, Oliveira MAD, Hui D, Paiva CE. Factors associated with palliative care referral among patients with advanced cancers: a retrospective analysis of a large Brazilian cohort. Support Care Cancer. 2018;1–9. doi:10.1007/s00520-017-4031-y
17. Colibaseanu DT, Osagiede O, Spaulding AC, et al. The determinants of palliative care use in patients with colorectal cancer: a national study. Am J Hosp Palliat Med. 2018:1049909118765092. doi:10.1177/1049909118765092.
18. Bakitas MA, Tosteson TD, Li Z, et al. Early versus delayed initiation of concurrent palliative oncology care: patient outcomes in the ENABLE III randomized controlled trial. J Clin Oncol Off J Am Soc Clin Oncol. 2015;33(13):1438–1445. doi:10.1200/JCO.2014.58.6362
19. Temel JS, Greer JA, Muzikansky A, et al. Early palliative care for patients with metastatic non-small-cell lung cancer. N Engl J Med. 2010;363(8):733–742. doi:10.1056/NEJMoa1000678
20. Zimmermann C, Swami N, Krzyzanowska M, et al. Early palliative care for patients with advanced cancer: a cluster-randomised controlled trial. Lancet Lond Engl. 2014;383(9930):1721–1730. doi:10.1016/S0140-6736(13)62416-2
21. Wright AA, Zhang B, Ray A, et al. Associations between end-of-life discussions, patient mental health, medical care near death, and caregiver bereavement adjustment. JAMA. 2008;300(14):1665–1673. doi:10.1001/jama.300.14.1665
22. Dionne-Odom JN, Azuero A, Lyons KD, et al. Benefits of early versus delayed palliative care to informal family caregivers of patients with advanced cancer: outcomes from the ENABLE III randomized controlled trial. J Clin Oncol Off J Am Soc Clin Oncol. 2015;33(13):1446–1452. doi:10.1200/JCO.2014.58.7824
23. Higginson IJ, Addington-Hall JM. Palliative care needs to be provided on basis of need rather than diagnosis. BMJ. 1999;318(7176):123. doi:10.1136/bmj.318.7176.123
24. Hui D, Elsayem A, De la Cruz M, et al. Availability and integration of palliative care at US cancer centers. JAMA. 2010;303(11):1054–1061. doi:10.1001/jama.2010.258
25. Cheng -W-W, Willey J, Palmer JL, Zhang T, Bruera E. Interval between palliative care referral and death among patients treated at a comprehensive cancer center. J Palliat Med. 2005;8(5):1025–1032. doi:10.1089/jpm.2005.8.1025
26. Bruera E, Hui D. Integrating supportive and palliative care in the trajectory of cancer: establishing goals and models of care. J Clin Oncol Off J Am Soc Clin Oncol. 2010;28(25):4013–4017. doi:10.1200/JCO.2010.29.5618
27. Yoong J, Park ER, Greer JA, et al. Early palliative care in advanced lung cancer: a qualitative study. JAMA Intern Med. 2013;173(4):283–290. doi:10.1001/jamainternmed.2013.1874
28. Freireich EJ, Kurzrock R. The role of investigational therapy in management of patients with advanced metastatic malignancy. J Clin Oncol. 2009;27(2):304–306. doi:10.1200/JCO.2008.19.6543
29. De Lima L, Pastrana T. Opportunities for palliative care in public health. Annu Rev Public Health. 2016;37:357–374. doi:10.1146/annurev-publhealth-032315-021448
30. Rodriguez KL, Barnato AE, Arnold RM. Perceptions and utilization of palliative care services in acute care hospitals. J Palliat Med. 2007;10(1):99–110. doi:10.1089/jpm.2006.0155
31. Beaussant Y, Daguindau E, Chauchet A, et al. Hospital end-of-life care in haematological malignancies. BMJ Support Palliat Care. 2018;8(3):314–324. doi:10.1136/bmjspcare-2017-001446
32. Poulalhon C, Rotelli-Bihet L, Moine S, Fagot-Campagna A, Aubry R, Tuppin P. Use of hospital palliative care according to the place of death and disease one year before death in 2013: a French national observational study. BMC Palliat Care. 2018;17(1):75. doi:10.1186/s12904-018-0327-z
33. Gallais Sérézal I, Beaussant Y, Rochigneux P, et al. End-of-life care for hospitalized patients with metastatic melanoma in France: a nationwide, register-based study. Br J Dermatol. 2016;175(3):583–592. doi:10.1111/bjd.14631
34. Bousquet PJ, Lefeuvre D, Tuppin P, et al. Cancer care and public health policy evaluations in France: usefulness of the national cancer cohort. PLoS One. 2018;13(10):e0206448. doi:10.1371/journal.pone.0206448
35. Tuppin P, Rudant J, Constantinou P, et al. Value of a national administrative database to guide public decisions: from the système national d’information interrégimes de l’Assurance Maladie (SNIIRAM) to the système national des données de santé (SNDS) in France. Rev Epidemiol Sante Publique. 2017;65(Suppl 4):S149–S167. doi:10.1016/j.respe.2017.05.004
36. Morin L, Aubry R. The development of palliative care services in France (1987–2013). Med Palliat. 2015;14(3):134–141.
37.
38. Tuppin P, Rivière S, Rigault A, et al. Prevalence and economic burden of cardiovascular diseases in France in 2013 according to the national health insurance scheme database. Arch Cardiovasc Dis. 2016;109(6–7):399–411. doi:10.1016/j.acvd.2016.01.011
39. Rey G, Jougla E, Fouillet A, Hémon D. Ecological association between a deprivation index and mortality in France over the period 1997–2001: variations with spatial scale, degree of urbanicity, age, gender and cause of death. BMC Public Health. 2009;9:33. doi:10.1186/1471-2458-9-33
40. Benchimol EI, Smeeth L, Guttmann A, et al. The reporting of studies conducted using observational routinely-collected health data (RECORD) statement. PLoS Med. 2015;12(10):e1001885. doi:10.1371/journal.pmed.1001885
41. Rosenwax L, McNamara B, Blackmore A, Holman C. Estimating the size of a potential palliative care population. Palliat Med. 2005;19(7):556–562. doi:10.1191/0269216305pm1067oa
42. Bennett MI, Ziegler L, Allsop M, Daniel S, Hurlow A. What determines duration of palliative care before death for patients with advanced disease? A retrospective cohort study of community and hospital palliative care provision in a large UK city. BMJ Open. 2016;6(12):e012576. doi:10.1136/bmjopen-2016-012576
43. Merchant SJ, Brogly SB, Goldie C, et al. Palliative care is associated with reduced aggressive end-of-life care in patients with gastrointestinal cancer. Ann Surg Oncol. 2018;25(6):1478–1487. doi:10.1245/s10434-018-6430-9
44. Morin L, Aubry R, Frova L, et al. Estimating the need for palliative care at the population level: A cross-national study in 12 countries. Palliat Med. 2017;31(6):526–536. doi:10.1177/0269216316671280
45. Ravanello A., Rotelli-Bihet L. Atlas des soins palliatifs et de la fin de vie en France : Première édition - 2018. Paris : Centre national des soins palliatifs et de la fin de vie, 2018, 70.
46. Ziegler LE, Craigs CL, West RM, et al. Is palliative care support associated with better quality end-of-life care indicators for patients with advanced cancer? A retrospective cohort study. BMJ Open. 2018;8:1. doi:10.1136/bmjopen-2017-018284
47. Ahmed N, Bestall JC, Ahmedzai SH, Payne SA, Clark D, Noble B. Systematic review of the problems and issues of accessing specialist palliative care by patients, carers and health and social care professionals. Palliat Med. 2004;18(6):525–542. doi:10.1191/0269216304pm921oa
48. Lloyd A, Kendall M, Carduff E, Cavers D, Kimbell B, Murray SA. Why do older people get less palliative care than younger people? Eur J Palliative Care. 2016;23(3). Available from:
49. Désesquelles A, Gamboni A, Demuru E, the MultiCause network. We only die once… but from how many causes? Popul Soc. 2016;(534). Available from:
50.
51. Fletcher K, Prigerson HG, Paulk E, et al. Gender differences in the evolution of illness understanding among patients with advanced cancer. J Support Oncol. 2013;11(3):126–132.
52. Saeed F, Hoerger M, Norton SA, Guancial E, Epstein RM, Duberstein PR. Preference for palliative care in cancer patients: are men and women alike? J Pain Symptom Manage. 2018;56(1):1–6.e1. doi:10.1016/j.jpainsymman.2018.03.014
53. Taillibert S, Laigle-Donadey F, Sanson M. Palliative care in patients with primary brain tumors. Curr Opin Oncol. 2004;16(6):587–592.
54. McGrath P, Holewa H. Special considerations for haematology patients in relation to end-of-life care: australian findings. Eur J Cancer Care (Engl). 2007;16(2):164–171. doi:10.1111/j.1365-2354.2006.00745.x
55. Ho TH, Barbera L, Saskin R, Lu H, Neville BA, Earle CC. Trends in the aggressiveness of end-of-life cancer care in the universal health care system of Ontario, Canada. J Clin Oncol Off J Am Soc Clin Oncol. 2011;29(12):1587–1591. doi:10.1200/JCO.2010.31.9897
56. Nipp RD, El-Jawahri A, Moran SM, et al. The relationship between physical and psychological symptoms and health care utilization in hospitalized patients with advanced cancer. Cancer. 2017;123(23):4720–4727. doi:10.1002/cncr.30912
57. Moran SMC, El-Jawahri A, Pirl WF, et al. Symptom burden in hospitalized patients with advanced cancer. J Clin Oncol. 2015;33(29_suppl):100. doi:10.1200/jco.2015.33.29_suppl.100
58. Bakitas M, Lyons KD, Hegel MT, et al. The project ENABLE II randomized controlled trial to improve palliative care for rural patients with advanced cancer: baseline findings, methodological challenges, and solutions. Palliat Support Care. 2009;7(1):75–86. doi:10.1017/S1478951509000108
59. Hui D, Kim SH, Roquemore J, Dev R, Chisholm G, Bruera E. Impact of timing and setting of palliative care referral on quality of end-of-life care in cancer patients. Cancer. 2014;120(11):1743–1749.
60. Alshammary SA, Alsuhail A, Duraisamy BP, Alabdullateef SH, Ratnapalan S. Interval between first palliative care consultation and death among patients in a comprehensive cancer center in Saudi Arabia. J Health Spec. 2015;3(2):61. doi:10.4103/1658-600X.156107
61. Kwon JH, Hui D, Chisholm G, et al. Clinical characteristics of cancer patients referred early to supportive and palliative care. J Palliat Med. 2013;16(2):148–155. doi:10.1089/jpm.2012.0344
62. Guo Q, Jacelon CS, Marquard JL. An evolutionary concept analysis of palliative care. J Palliat Care Med. 2012;2(6):1–6. doi:10.4172/2165-7386.1000127
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
