Back to Journals » International Journal of Women's Health » Volume 15
A Vagino-Laparoscopic Strategy for Hysterectomy of Large Uteri to Ease Surgical Challenges
Authors Purohit R , Sharma JG, Meher D
Received 29 December 2022
Accepted for publication 2 March 2023
Published 14 March 2023 Volume 2023:15 Pages 369—379
DOI https://doi.org/10.2147/IJWH.S400587
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Everett Magann
Supplementary video 2 of "Vagino-laparoscopic hysterectomy" [ID 400587].
Views: 235
Ramkrishna Purohit, Jay Gopal Sharma, Devajani Meher
Purohit General Hospital, Bargarh, Odisha, India
Correspondence: Ramkrishna Purohit, Purohit General Hospital, Bargarh, Odisha, 768028, India, Email [email protected]
Purpose: To develop a vagino-laparoscopic strategy for hysterectomy (VLH) to treat uteri with large fibroids at ≥ 16 weeks of gestation to ease surgical challenges.
Patients and Methods: This was an observational study conducted in our private general hospital on 64 consecutive cases involving uteri with large and benign fibroids at ≥ 16 weeks of gestation. We excluded cases with an associated ventro-fixed uterus and large cervical fibroids.
Interventions: The VLH strategy involves vaginal separation of the uterosacral with the uterine arteries followed by laparoscopic separation of the remaining upper pedicles. The uterus was then removed vaginally.
Results: The largest uteri receiving treatment was at 26 weeks of gestation and the mean uterus weight was 869.60 ± 275.10 g (range: 500– 1900 g). The VLH strategy was successful in 63 (98.43%) cases irrespective of the configuration of the uterus. One case (1.56%) required mini-laparotomy conversion due to the need for adhesiolysis; this case exhibited extensive adhesion of the rectum to the posterior wall of the uterus due to a history of previous myomectomy of the posterior wall. There were no conversions due to failed laparoscopic exposure of the adnexal or uterine vascular pedicles, or due to uncontrolled intraoperative bleeding. There were no cases of urinary tract injury or other major complications. The vaginal detachment of uterosacral ligaments before the laparoscopic phase of the VLH strategy increased upwards mobility and dislodged the cervico-isthmic level of large uteri from the narrow lower aspect of the pelvis to the upper wider part of the pelvis; this eased the surgical challenges associated with such cases and avoided complications during laparoscopy.
Conclusion: We developed a vagino-laparoscopic strategy for hysterectomy that can ease the technical challenges associated with the majority of large uteri.
Keywords: surgical challenges during laparoscopic hysterectomy, large fibroid uterus, laparoscopic hysterectomy, thick uterovesical scar, displaced adnexal and uterine vessels
Introduction
Several routes can be used for hysterectomy; however, the vaginal route is the least invasive option. Where possible, the vaginal route should be preferred over strategies that involve laparoscopy or laparoscopic assistance; this is because the vaginal route requires less surgical time and reduces hospital costs.1–3 Uteri with large fibroids are difficult to treat by vaginal hysterectomy as such cases are technically challenging. Existing literature support the fact that vaginal hysterectomy can be performed by various techniques in many cases that involve a uterus with large fibroids up to 16 weeks of gestation, although there is no set upper limit.4 In most large uteri, it is possible to separate the lower pedicles up to the uterine artery via the vaginal approach. However, the expanded upper part of a uterus with a large fibroid (≥16 weeks of gestation) commonly resists descent and often requires debulking; this is challenging and occasionally results in a failed vaginal hysterectomy. The use of total laparoscopic hysterectomy (TLH) and laparoscopic assisted vaginal hysterectomy (LAVH) for uteri with large fibroids are associated with significant surgical and technical challenges, even in skilled hands. Thus, in cases where we anticipated difficult vaginal and laparoscopic hysterectomy of a large uterus, we planned vaginal separation of the lower pedicles up to the uterine artery followed by laparoscopic separation of the upper pedicles. Our overall aim was to ease surgical and technical challenges during the laparoscopic phase and make it simpler to remove a large uterus via the vaginal route by performing a minimally invasive strategy. Therefore, in this study, we describe the development of a vagino-laparoscopic strategy for hysterectomy to treat cases involving uteri with large fibroids at ≥ 16 weeks of gestation and report the clinical outcomes of our patients.
Materials and Methods
We conducted an observational study in our private clinic between September 2020 and August 2022 on all candidates for hysterectomy due to a non-prolapsed uterus with large and benign fibroids at ≥16 weeks of gestation. Cases with a ventro-fixed uterus and large cervical fibroids were excluded. The included candidates were all subjected to the vagino-laparoscopic hysterectomy (VLH) procedure described below.
This study was approved by the Purohit General Hospital Institutional Ethics Committee prior to the inclusion of the first case. It complies with the declaration of Helsinki.
All participants provided signed and informed consent in this research study as well as consent for surgery. We investigated the success and failure of each case, along with intraoperative challenges and complications. Data were analysed by descriptive statistics.
The Vagino-Laparoscopic Strategy
The surgical procedure commenced vaginally and was completed laparoscopically. The uterus was then removed vaginally.
The Vaginal Phase
The procedure was started using the purohit technique for vaginal hysterectomy.5 An open bipolar sealer/shearer (17 cm in length) was used instead of ordinary bipolar forceps for coagulation and for the division of anatomies to separate the lower part of the uterus from the bodily attachments.
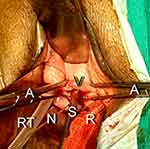
The vaginal wall, supravaginal ligament, and cardinal ligaments were sequentially separated from the cervix. These manoeuvres, helped to expose the posterior cul-de-sac. Then, we opened the posterior cul-de-sac. Thereafter, the uterosacral ligament was hooked from the posterior aspect by right-angle forceps and then separated from the cervix. These manoeuvres helped to expose the bulge of the uterine artery. Then, the uterine artery was hooked by right-angle forceps, coagulated, and then divided by a sealer/shearer between the prongs of right-angle forceps (Figure 1, Supplementary Video 1). This was repeated on the opposite side to separate the uterine artery bilaterally. Then, the uterovesical space was dissected as far as possible. Then, preparation was done for the laparoscopic phase to separate the remaining upper pedicles. The venous openings of the wall on the cervical side were adequately coagulated to prevent backflow bleeding. The distal end of a Ryle’s tube (with pores) was then inserted into the right side of the pelvis through the posterior cul-de-sac opening to create a pneumoperitoneum for laparoscopy. Holding the posterior vaginal vault incision by Alli’s forceps, two roller gauze packs were placed in the posterior cul-de-sac, one on each side of the midline above the vault; we did this to reduce gas leakage and to compress venous oozing. A nylon thread (number 1) was inserted and tied to the cervical lip and held far below the introitus by artery forceps. Then, a straight metal laparoscopic suction cannula (5 mm) was inserted into the uterine cavity. This was used for upwards and side-to-side uterine manipulation during laparoscopy. Then, the margins of the vaginal stump were horizontally clamped by two Alli’s forceps below the cervix, one on each side of the suction cannula (Figure 2). Then, the surgeon began the laparoscopic phase.
Laparoscopic Phase
CO2 gas was passed through the Ryle’s tube to create a pneumoperitoneum. A primary intraumbilical or supraumbilical port was then inserted depending on the level of uterine fundus. Then, the gas channel was switched on to the side channel of the primary port. A 5 mm lateral port was inserted just below the level of the umbilicus on the left side and another on the right side. A third 5mm suprapubic port was then inserted in the midline above the pubic hairline level. Intra-abdominal pressure was maintained at 10–12 mm of Hg.
Next, the metal suction cannula was pushed gently upwards and then from side to side by the vaginal assistant to elevate the uterus similar to a tent. These manoeuvres dislodged the distended lower part of the large uterus from the narrow lower pelvis and placed it onto the wider upper part of the pelvis. In addition, we increased the degree of anteromedial motion of the cornue by applying a laparoscopic myoma screw around the straight uterine manipulator. This manoeuvre helped to expose the posteriorly displaced cornual pedicles (Figure 3, Supplementary Videos 1 and 2); this occurred far from the lateral wall in cases with a large fundal or cornual fibroid. In addition, these manoeuvres loosened the broad ligament and helped to create a distance of 4–5 cm between the lateral wall of the uterus and the lateral pelvic wall, even in cases with a broad ligament fibroid. The combination of bilateral upper vascular pedicle separation and bilateral vaginal division of the uterine artery made the uterus avascular and allowed bloodless dissection of the lower broad ligament.
Then, the anterior and posterior folds of the stretched broad ligament below the round ligament were gradually separated with a bipolar shearer in a downwards direction while hugging the lateral uterine wall (not close to the pelvic wall). The anterior leaf incision joined the vaginally dissected uterovesical space from the lateral aspect. The posterior leaf incision joined the vaginally dissected incision between the uterosacral ligament and the cervix. At this stage, the vaginally separated cervix and uterine artery stump could be clearly visible anteriorly through the uterovesical space (Figure 4, Supplementary Videos 1 and 2) and posteriorly through the posterior cul-de-sac. Next, a laparoscopic suction cannula was inserted through the suprapubic port and moved into the uterovesical space from the lateral aspect. The remaining uterovesical fold, bladder pillars, and lower part of the broad ligament (including the veins) were stretched by the suction cannula away from the cervix to define the dissection plane (Figure 5, Supplementary Video 1) and then separated from the lateral aspect by the bipolar sealer-shearer hugging the uterus to complete the hysterectomy. This manoeuvre kept the bipolar incision far from the lateral pelvic wall. Next, we performed bilateral opportunistic salpingectomy. The indicated adnexectomy was then performed and the excised adnexa was positioned above the vault for vaginal removal. Then, the surgeon moved to the vaginal side. The thread tied to the cervix was then gradually pulled down vaginally to expose the cervix. The Ryle’s tube, uterine manipulator, and roller gauze were then removed. Next, the uterus was vaginally removed by applying conventional vaginal morcellation techniques. No laparoscopic morcellator was used. Then, we performed laparoscopic lavage and closed the vault vaginally in two layers.
Additional Techniques That Can Be Applied During the Laparoscopic Phase in Certain Situations
- The broad ligament (lower margin) elevation technique to expose a vaginally undivided uterine artery.
Pulsatile bleeding from the uterine sidewall during the separation of cornual pedicles indicates the presence of a vaginally undivided and intact uterine artery. In such cases, we separated the uterovesical fold and then moved the suprapubic port suction cannula in the posterior direction through the incision between the lateral wall of the cervix and the uterosacral stump to touch the pelvic wall. Then, the lower margin of the broad ligament was elevated laterally forwards by the cannula (Figure 6). This elevation manoeuvre brought the posteriorly displaced contents of the broad ligament into the surgeon’s view. Then, the displaced uterine artery from the heavy distended uterus was skeletonised, coagulated 2–3 times along the exposed pedicle and divided close to the uterine wall. This manoeuvre produces a long uterine artery stump far from the lateral pelvic wall while avoiding ureteric injury.
Then, using a monopolar hook or bipolar shear, we made a deep incision from the right side above the level of the uterine artery or the distended part of the uterus obliquely around the anterior wall to the opposite side below the round ligament. Then, the uterus was rotated by the myoma screw to expose the intact posterior surface of the uterus. The incision was continued spirally upwards around the posterior wall to reduce the girth and the uterus was elongated for easy passage through the pelvic cavity. We did not use a laparoscopic morcellator.
All cases were followed up postoperatively for 6 weeks.
Results
Table 1 shows the characteristics of the patients. In total, 64 cases were diagnosed with a large fibroid uterus and underwent VLH during the study period. The maximum size of the uterus was at 26 weeks-of-gestation. Cases were included irrespective of nulliparity, a large single intramural fibroid (≥ 10 cm), an associated large cornual fibroid or large broad ligament fibroid (≥ 7.5 cm), previous pelvic surgery, and previous CS.
 |
Table 1 Preoperative Characteristics of the Patients |
Table 2 shows intraoperative challenges and solutions. The uterosacral ligaments were separated vaginally in a bilateral manner in all cases. This helped to increase the upwards mobility of the cervix isthmic level from the narrow lower pelvis to the upper wider pelvis during the laparoscopic phase. This also eased the ergonomics of laparoscopy. No difficulties were experienced with regards to laparoscopic exposure and separation of the upper pedicles.
 |
Table 2 Intraoperative Challenges and Solutions |
The bilateral uterine vessels were secured successfully by the vaginal route in 47 cases (73.43%) before moving to the laparoscopic phase. There was no concern with regards to intraoperative bleeding. In the remaining 17 cases (26.56%), vaginal ligation of the uterine artery (unilateral or bilateral) was unsuccessful and there was concern over intraoperative bleeding during the laparoscopic phase. In these cases, we used the additional broad ligament elevation technique to successfully divide the uterine arteries laparoscopically.
Very thick uterovesical fold appearing like the serosa of the uterine wall following a previous CS was observed in 7/64 (10.93%) or 7/21 (33.33%) previous CS cases. In these cases, we used the additional uterovesical scar elevation technique to help separate the uterovesical fold laparoscopically from the uterus. In other cases of previous CS, we experienced no difficulty in separating the uterovesical scar or fold from the uterus.
Heavy uteri were evident in 8 cases (12.5%) and required laparoscopic slimming of the uterus before we attempted extraction vaginally. In other cases, vaginal morcellation was performed by conventional methods to facilitate removal of the uterus.
In all cases, there was no loss of the pneumoperitoneum through the vaginal vault.
Table 3 shows the causes of displaced uterine arteries and failed vaginal division. The causes of failed vaginal division of the uterine artery were due to the uterine vessels being displaced either anteriorly, posteriorly, or cranially by the expanded lower part of the uterine corpus. These cases had either a “T”- or an inverted “L”- shaped angulation of the expanded lower uterine corpus (as the horizontal arm) over the slender cervix (as the vertical leg) at the isthmic level. These risky cases had either large and broad ligament splitting fibroids (≥ 7.5 cm), large cornual fibroids (≥ 7.5 cm) stretching cornual pedicles, very thick and wide uterovesical scars with a thick and scarred peritoneal fold following a previous CS, or a dorsofixed uterus following previous posterior uterine wall myomectomy and mostly associated with a uterus at ≥ 20 weeks-of-gestation. All of these pathologies resisted uterine descent and kept the uterine artery pedicle at a high level beyond the reach of the vaginal surgeon. Displaced uterine vessels were evident, irrespective of whether the uteri weighed < or > 1000 g.
 |
Table 3 Causes of Displaced Uterine Arteries and Failed Vaginal Division |
Table 4 shows the outcomes of VLH which was successfully performed in 63 cases (98.43%). One case (1.56%) required mini-laparotomy conversion so that we were able to perform adhesiolysis due to wide adhesion of the posterior wall of the uterus to the rectum; this particular patient had a history of previous myomectomy of the posterior wall. Analysis showed that uterine weight exceeded 1000 g in 14 cases (21.87%).
 |
Table 4 The Outcomes of VLH |
None of the cases experienced bladder or ureteric injury. Intraoperative bleeding during the VLH procedure was 300–500mL in 12 cases (18.75%) and 501–900mL in 4 cases (6.25%); bleeding was mostly related to cases involving failed vaginal ligation of one or both uterine arteries. There was no conversion due to uncontrolled intraoperative bleeding and no other major intraoperative and postoperative complications.
Discussion
Here, we describe a new strategy (VLH) to ease the technical challenges associated with laparoscopic hysterectomy for cases with large uteri. This new technique involves two phases: a vaginal phase (up to the uterine artery) and then a laparoscopic phase. This strategy overcomes the technical difficulty of exposing the displaced adnexal vascular pedicles when using laparoscopy. In addition, the broad ligament elevation technique overcomes the technical challenges associated with exposing the displaced uterine vessels without the need to consider the outer configurations of the large uterus. The additional uterovesical elevation technique overcomes the technical difficulties associated with exposing the uterovesical dissection plane in cases with thick uterovesical scarting following previous CS.
Displacement of the adnexal and uterine vascular pedicles by an asymmetrically configured large uterus has been identified by conventional methods of laparoscopic hysterectomy as a potential risk factor for technical difficulties, conversions, and intraoperative surgical complications.6 Our VLH technique is minimally invasive and can achieve satisfactory outcomes irrespective of the external uterine configuration (Table 3). VLH can also overcome difficulties associated with the conventional laparoscopic technique when exposing and securing the displaced adnexal and uterine vessels. In contrast to a previous study,6 none of the cases described herein required conversion to laparotomy due to the failure to expose the vascular pedicles or due to uncontrolled intraoperative bleeding, even though we included cases where the uteri were in ≥ 24 weeks-of-gestation, weighed ≥ 1000 g, or contained large fibroids that were ≥ 10 cm in size.7
The increased upwards mobility of the large uterine mass following the vaginal separation of uterosacral ligaments in these risky cases (Table 3) with a large broad ligament, large cornual fibroids or thick scarring from previous CS, helped us to reduce the technical difficulty, simplified the range of instrument motion, and increased laparoscopic accessibility to the displaced vascular pedicles.
In 47 cases (73.43%), the vaginal artery was successfully ligated bilaterally (Table 2) and the surgeon experienced no difficulties during the laparoscopic phase to complete VLH. Separation of the upper pedicles devascularized the uterus; subsequent separation of the broad ligament completed the hysterectomy; no additional manoeuvres were required.
In 17 cases (26.56%), ligation of the vaginal artery was unsuccessful (on one or both sides) (Table 2; in these cases, the surgeon predicted an increased intraoperative blood loss during the laparoscopic phase. These issues were due to the displacement of uterine vessels caused by different pathologies (Table 3). Collectively, the vaginal phase, the laparoscopic phase, and the additional broad ligament elevation technique during the laparoscopic phase, simplified the surgical challenges associated with securing and divide the uterine arteries in large “T” and inverted “L” shaped uteri (Table 3).
In seven cases (10.93%) we observed a very thick uterovesical scar with a uterovesical fold that appeared to be similar to the uterine serosa; in these cases, there was a concern for bladder injury. In our VLH technique, the technical challenges associated with finding the dissection plane between the bladder and uterus when performing conventional laparoscopic hysterectomy (TLH/LAVH) was simplified by including an additional vaginal phase prior to the laparoscopic phase.
Similar to the finding by M Roushdy in vaginally assisted laparoscopic hysterectomy,8 none of the cases undergoing VLH experienced bladder or ureteric injury, despite some cases having a history of CS, a large uterus weighing ≥ 1000 g, or large and broad ligament fibroids (Table 4). When using the VLH strategy, there was no requirement for laparoscopic retroperitoneal uterine artery ligation or ureteric dissection. By performing the vaginal phase up to the uterine artery, the laparoscopic phase above the uterine artery, and applying the additional broad ligament elevation technique and the additional uterovesical scar elevation technique in indicated cases, we successfully able to avoid urinary tract injury in the VLH strategy.
The cervix was accessible vaginally in all cases; therefore, we were able to commence surgery via the vaginal route. Cases with a cervix that could not be accessed vaginally, such as those with a ventrofixed uterus and those with large cervical fibroids, were excluded from VLH. Two cases (3.12%) had a large uterus and were at 16 weeks-of-gestation (Table 1); these cases were indicated for VLH due to broad ligament fibroids and multiple CS previously. In other cases, the indications for VLH included a large upper uterine mass, large broad ligament fibroids, and large cornual fibroids.
Using VLH, the lateral attachments of the uterus below the level of the isthmus were separated vaginally by applying a bipolar sealer/shearer. The lateral attachments above the isthmus were then separated laparoscopically by a bipolar sealer/shearer. The vaginal bipolar shearer is a short version of the long laparoscopic bipolar shear. This bipolar sealer/shearer avoided the technical challenges associated with traditional suture ligation of the uterine artery during the vaginal phase of VLH. This approach combines the advantages of the least invasive vaginal surgery with those of minimally invasive laparoscopic surgery.
There were some limitations that need to be considered. For example, surgeons would need to become competent at vaginal hysterectomy with the bipolar shears. However, this technique is simple for vaginal surgeon, even with average laparoscopic ability. Of course, It requires further multicentric evaluation.
Conclusion
Here, we describe the development of a new vagino-laparoscopic strategy for hysterectomy that simplifies the technical challenges associated with cases with large uteri.
Precis
Development of a vagino-laparoscopic strategy for hysterectomy can be performed to ease the technical challenges associated with the majority of large uteri.
Acknowledgments
The authors would like to thank Vijay Babar for the statistical assistance.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
No external funding was received for this study.
Disclosure
None of the authors have any conflicts of interest to declare for this work.
References
1. Aarts JW, Nieboer TE, Johnson N, et al. Surgical approach to hysterectomy for benign gynaecological disease. Cochrane Database Syst Rev. 2015;2015:8.
2. Sandberg EM, Twijnstra ARH, Driessen SRC, et al. Total laparoscopic hysterectomy versus vaginal hysterectomy: a systematic review and meta-analysis. J Minim Invasive Gynecol. 2017;24(2):206–217.
3. Kho W. Abr~ao MS. In search for the best minimally invasive hysterectomy approach for the large uterus: a review. Clin Obstet Gynecol. 2017;60:286–295.
4. Fashokun TB, Honda VL. Vaginal hysterectomy. In: Handa VL, Le Linda V, editors. Telinde’s Operative Gynaecology.
5. Purohit RK. Purohit technique of vaginal hysterectomy: a new approach. BJOG. 2003;110(12):1115–1119.
6. Uccella S, Kho RM, Garzon S, et al.; BJOG. The large uterus classification system: a prospective observational study. BJOG. 2021;128:1526–1533.
7. Cianci S, Gueli Alletti S, Rumolo V, et al. Total laparoscopic hysterectomy for enlarged uteri: factors associated with the rate of conversion to open surgery. J Obstet Gynaecol. 2019;39:805–810.
8. Roushdy M. Vaginally assisted laparoscopic hysterectomy: a technique suited for large uteri. Gynaecol Endosc. 1997;6:95–97.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.