Back to Journals » International Journal of General Medicine » Volume 12
A Unique Case Of Tenofovir-Induced DRESS Syndrome Associated With Raynaud’s Of The Tongue
Authors Aqtash O, Ajmeri AN , Thornhill BA, Anderson E, Carroll R, Elhamdani A , Tackett E
Received 18 May 2019
Accepted for publication 17 September 2019
Published 23 October 2019 Volume 2019:12 Pages 381—385
DOI https://doi.org/10.2147/IJGM.S215511
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser

Obadah Aqtash,1 Aman Naim Ajmeri,1 Brent A Thornhill,1 Elise Anderson,2 Ryan Carroll,1 Adee Elhamdani,1 Eva Tackett1
1Internal Medicine, Joan C. Edwards School of Medicine, Marshall University, Huntington, WV 25701, USA; 2Charleston Area Medical Center, Charelston, WV 25701, USA
Correspondence: Aman Naim Ajmeri
Internal Medicine, Joan C. Edwards School of Medicine, Marshall University, Huntington, WV 25701, USA,
Email [email protected]
Abstract: Drug reaction with eosinophilia and systemic symptoms (DRESS) is a potentially fatal severe adverse reaction to medications. Numerous drugs have been implicated, with carbamazepine and allopurinol being the most common. Tenofovir-induced DRESS is extremely rare. We report a case of a 65-year-old male patient with a diffuse exfoliative maculopapular rash across his entire body of five weeks of duration. The patient also had icteric sclera, abnormal liver enzymes and Raynaud’s of the tongue, nose and the left fifth finger. After discontinuation of tenofovir, the case resolved over a span of ten days. A high index of suspicion is crucial along with the prompt withdrawal of the offending medication for a good outcome.
Keywords: DRESS, drug reaction with eosinophilia and systemic symptoms, tenofovir, tenofovir-induced DRESS, Raynaud’s phenomena, Raynaud’s of the tongue
Introduction
Drug reaction with eosinophilia and systemic symptoms (DRESS) is a potentially fatal severe adverse reaction associated with multiple medications. It is characterized by a prolonged latency period and includes skin eruption and internal organ involvement. Onset of symptoms occurs 2–6 weeks after initiating use of the offending agent. It has a diverse range of clinical manifestations but typically presents with fever, rash, lymphadenopathy and single or multi-organ involvement.1 The liver is most frequently affected but all organs are potentially susceptible. A mortality rate of approximately 10% has been reported.2 The incidence is uncertain but it has an estimated population risk that ranges between 1 in 1000 and 1 in 10,000 drug exposures.3 Fifty or more drugs have been implicated, but tenofovir-induced DRESS is extremely rare has only been previously reported once.4,5 Herein, we report a case of a patient who developed tenofovir-induced DRESS that manifested as liver failure, skin eruption, and Raynaud’s of the tongue.
Case Presentation
A 65-year-old male patient was transferred from a local hospital with the complaint of a generalized skin rash, tongue swelling and lip peeling without mucous membrane involvement. The rash started approximately five weeks ago, appearing as red welts on the abdomen that then spread in a generalized manner throughout the body. At that time, the rash was described as a generalized maculopapular rash that was erythematous and non-blanching and treatment with steroids resulted in clinical improvement. Two weeks prior to this hospital visit, the rash had returned with peeling of the skin. During this hospital visit, there were new features in the form of itching and sloughing of skin.
The patient was hemodynamically stable with a blood pressure of 135/96, heart rate of 95, and temperature of 36.5°C. On physical exam, the patient had icteric sclera and a diffuse exfoliative maculopapular rash involving the head, face, abdomen, arms and legs (See Figure 1A–E). On laboratory evaluation, complete blood count and basic metabolic panel were found to be normal with the exceptions of white blood cell count of 11.3 k/cmm and sodium level of 133 mEq/L. Liver function testing was significant for alkaline phosphatase level of 1505 units/L, AST 376 units/L, ALT 595 units/L, total bilirubin of 15.4 mg/dL, and direct bilirubin of 12.8 mg/dL. Ultrasound of the abdomen and duplex scan were both unremarkable. Malignancies were included in the differential; however, CT of chest and abdomen without contrast, nuclear bone scan, and scrotal ultrasound were negative.
 |
Figure 1 Patient’s appearance upon admission with diffuse exfoliative maculopapular rash shown on the (A) head, (B) forehead, (C) abdomen, (D) arms and (E) legs. |
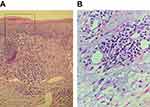
The patient indicated that he was diagnosed with hepatitis B two months earlier. He was started on emtricitabine/tenofovir at that time. Records obtained from the outside hospital showed that the patient’s liver enzymes were normal three weeks earlier, but revealed an eosinophil count of 25% with a repeat of 33% and an absolute eosinophil count of 7.46 K/µL. The patient was managed with normal saline, methylprednisolone 60mg every 6 hrs daily and benadryl and famotidine for itching. His tenofovir was discontinued. A skin biopsy was obtained, which showed spongiotic dermatitis with eosinophilia (See Figure 2A and B). Blood samples were tested for the presence of anti-human herpes virus 6 antibodies, but results showed none were detected.
During his hospital stay, the patient developed Raynaud’s of the tongue following ingestion of cold water (see Figure 3A and B). This was followed by Raynaud’s of the nose and left fifth finger. The patient remained in the hospital for close observation and the rash showed marked improvement after four days of therapy. Over the span of 10 days, the patient’s rash resolved and his liver enzymes normalized. The patient has remained off of tenofovir and emtricitabine. For an alternate hepatitis B treatment, the patient was given entecavir. He has not had a recurrence of DRESS a year following his hospital discharge.
 |
Figure 3 (A) Normal appearance of the patient’s tongue. (B) Raynaud’s phenomena of the tongue with central whitening of the lingua after drinking cold water. |
Discussion
In 1936, drug-induced hypersensitivity syndrome was first described in patients who were being treated with anticonvulsants.6 This was eventually further differentiated by Bouqet et al, who introduced the term DRESS syndrome to describe the reaction that occurs within two months of drug initiation with cutaneous eruptions, hematologic disturbances, and systemic involvement.7 While the pathogenesis is not fully understood, authors suggest that it involves the following: deficiencies or abnormalities of enzymes that detoxify medication metabolites; an association with reactivation of the herpesvirus family; and an ethnic susceptibility with particular human leukocyte antigens (HLA) alleles.8
Similar to most severe allergic reactions, DRESS syndrome can present with a rash, diffuse swelling, and eosinophilia. Distinctive of DRESS, however, is the occurrence of systemic involvement such as inflammation of the liver, kidneys, heart, or other organs.9 The appearance of symptoms is usually after a delay of 2–6 weeks of initiation of the causative drug.5 A prospective observational study published by Kardun et al, in 2013, analyzed the spectrum of signs and symptoms in DRESS syndrome. Results showed that all patients had a skin eruption with 79% of cases presenting with a rash that involved >50% of the body surface area and polymorphous features in 85% of cases.2 However, DRESS-induced Raynaud’s of the tongue has never been reported. Raynaud’s of the tongue has traditionally been described in association with or without underlying connective tissue disorders.10 Since Raynaud’s phenomena can be seen in hepatitis B, it is possible that the above-described occurrence may have been related to this condition. Given the timing of its presentation, it may also be a new rheumatological feature in an already complex syndrome.11
Diagnosing DRESS requires a high index of suspicion while keeping in mind the latency period, variety of symptoms and exclusion of other comparable non-drug conditions.1 Multiple guidelines have been established to help standardize the diagnosis of DRESS. Kardaun et al of the Severe Cutaneous Adverse Reactions (RegiSCAR) group proposed a scoring system in 2007 utilizing clinical and biological components. The criteria include a fever greater than 38.5°C; eosinophilia; skin involvement; enlarged lymph nodes; atypical lymphocytosis; organ involvement; time to resolution greater than 15 days; and the evaluation of other potential causes. Each criterion is given a score of minus one point, zero points, one point or two points. According to this system, a final score of less than two indicates no case, a final score of between two and three indicates a possible case, a final score of between four and five indicates a probable case, and a final score of greater than five indicates a definite case.12 In our case, the patient had a score of four points (one point each for eosinophilia, skin rash suggestive of DRESS, liver involvement, and evaluation of other potential causes), indicating a “probable case” of DRESS per the RegiSCAR scoring guidelines.
Another set of diagnostic criteria that have been accepted for use was proposed by a Japanese consensus group in 2006. It has seven components that are similar to those in the RegiSCAR criteria but with the main difference being that it includes human herpes 6 reactivation.13 Utilizing this criterion may prove difficult because of the emphasis on HHV-6 (human herpesvirus type 6), and tests like the measurement of IgG titer anti-HHV-6 are not yet commonly available.8
A skin biopsy can support the diagnosis but it is not specific. In the majority of cases, it can show varying grades of basal vacuolization, lymphocyte exocytosis, dyskeratosis, dermal edema & superficial perivascular inflammation with predominantly eosinophils.1 This presence of eosinophils is denser compared to other drug reactions.6 Our patient’s skin biopsy showed spongiotic dermatitis with eosinophilia. Other differentials to consider include Stevens–Johnson syndrome, toxic epidermal necrolysis, infectious mononucleosis, anti-retroviral syndrome, systemic lupus erythematosus, hypereosinophilic syndrome and Kawasaki disease amongst others.3,6
Various medications have been implicated in triggering DRESS syndrome with phenytoin, carbamazepine, and phenobarbital being the most common.14 It has also been associated with antiretroviral therapy15; however, tenofovir-induced DRESS has been reported only once in literature.4 Our patient was started on tenofovir two months earlier, developed a skin eruption with liver failure shortly thereafter, was found to have elevated eosinophils in his blood, a skin biopsy showing spongiotic dermatitis with eosinophilia, and a complete resolution of symptoms within 10 days of discontinuation of the medication. We state that our patient developed DRESS secondary to tenofovir. Although we did not perform the patch test, it may aid in recognizing the culprit drug and confirming it in 32–64% of cases.16
Once DRESS syndrome is recognized, it becomes vital to withdraw the offending agent immediately. Pharmacological treatment has not been established by randomized clinical trials and is currently based on case reports and retrospective studies.9 Mild cases or those without life-threatening organ failure can be treated with topical corticosteroids.17 The French Society of Dermatology recommends that more severe cases with involvement of one or more organs be treated with systemic corticosteroids.18 This has proven to be effective with improvement in clinical and lab parameters within days of administration.9 If despite systemic steroid use there is symptomatic progression, then other therapeutic options to consider include pulsed methylprednisone, intravenous immunoglobulin (IVIG), plasmapheresis or any of these in combination.8
Conclusion
Symptom delay, multiorgan involvement and significant mortality make DRESS syndrome an important differential for physicians to consider. A lack of awareness can risk a delay in diagnosis and treatment of individual symptoms before withdrawing the offending agent. This is the second reported case of tenofovir-induced DRESS syndrome. Additionally, this is the first recorded event of Raynaud’s of the tongue associated with DRESS syndrome.
Institutional Approval And Consent For Publication
Institutional approval was not required to publish the case details. Written informed consent was obtained from the patient for publication of this case report and any images relevant to the case.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Choudhary S, McLeod M, Torchia D, Romanelli P. Drug Reaction with Eosinophilia and Systemic (DRESS) Symptoms. J Clin Aesthet Dermatol. 2013;6(6):31–37.
2. Kardaun SH, Sekula P, Valeyrie-Allanore L, et al. Drug reaction with eosinophilia and systemic symptoms (DRESS): an original multisystem adverse drug reaction. Results from the prospective RegiSCAR study. Br J Dermatol. 2013;169(5):1071–1080. doi:10.1111/bjd.12501
3. Criado PR, Avancini J, Santi CG, Amoedo Medrado AT, Rodrigues CE, de Carvalho JF. Drug reaction with eosinophilia and systemic symptoms (DRESS): a complex interaction of drugs, viruses and the immune system. Isr Med Assoc J. 2012;14(9):577–582. doi:10.3390/ijms18061243
4. Bayonne Kombo ES, Gathse A. Syndrome d’hypersensibilité médicamenteuse au ténofovir ou DRESS chez une patiente infectée par le VIH. Med Mal Infect. 2013;43(3):134–135. doi:10.1016/j.medmal.2013.01.008
5. Cacoub P, Musette P, Descamps V, et al. The DRESS syndrome: a literature review. Am J Med. 2011;124(7):588–597. doi:10.1016/j.amjmed.2011.01.017
6. Cardoso CS, Vieira AM, Oliveira AP. DRESS syndrome: a case report and literature review. BMJ Case Rep. 2011;2–5. doi:10.1136/bcr.02.2011.3898
7. Bocquet H, Bagot M, Roujeau JC. Drug-induced pseudolymphoma and drug hypersensitivity syndrome (drug rash with eosinophilia and systemic symptoms: DRESS). Semin Cutan Med Surg. 1996;15(4):250–257. doi:10.1016/S1085-5629(96)80038-1
8. Paulo RC, Criado RFJ, Avancini JDM. Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS)/Drug-Induced Hypersensitivity Syndrome (DIHS): a review of current concepts*. An Bras Dermatol. 2012;3(87):435–449. doi:10.1155/2012/705190
9. Hall DJ, Fromm JS. Drug reaction with eosinophilia and systemic symptoms syndrome in a patient taking phenytoin and levetiracetam: a case report. J Med Case Rep. 2013;7:1–5. doi:10.1186/1752-1947-7-2
10. Bridges MJ, Kelly CA. Raynaud’s phenomenon affecting the tongue of a patient with scleroderma [3]. Ann Rheum Dis. 2002;61(5):472. doi:10.1136/ard.61.5.472
11. Kappus MR, Sterling RK. Extrahepatic manifestations of acute hepatitis B virus infection. Gastroenterol Hepatol (N Y). 2013;9(2):123–126.
12. Peyrière H, Dereure O, Breton H, et al. Variability in the clinical pattern of cutaneous side-effects of drugs with systemic symptoms: does a DRESS syndrome really exist? Br J Dermatol. 2006;155(2):422–428. doi:10.1111/j.1365-2133.2006.07284.x
13. Shiohara T, Iijima M, Ikezawa Z, Hashimoto K. The diagnosis of a DRESS syndrome has been sufficiently established on the basis of typical clinical features and viral reactivations [21]. Br J Dermatol. 2007;156(5):1083–1084. doi:10.1111/j.1365-2133.2007.07807.x
14. Oelze LL, Pillow MT. Phenytoin-induced drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome: a case report from the emergency department. J Emerg Med. 2013;44(1):75–78. doi:10.1016/j.jemermed.2011.05.052
15. Brandariz D, Smithson A, Anton-Vazquez V, Drug reaction with eosinophilia and systemic symptoms related to antiretroviral treatment in human immunodeficiency virus patients. Indian J Sex Transm Dis. 2017;38(2):163–170. doi:10.4103/ijstd.IJSTD_70_17
16. Zinn Z, Gayam S, Ba MPC, Honari G, Teng J. Patch testing for nonimmediate cutaneous adverse drug reactions. J Am Acad Dermatol. 2017;78(2):421–423. doi:10.1016/j.jaad.2017.08.049
17. Funck-Brentano E, Duong TA, Bouvresse S, et al. Therapeutic management of DRESS: a retrospective study of 38 cases. J Am Acad Dermatol. 2015;72(2):246–252. doi:10.1016/j.jaad.2014.10.032
18. Descamps V, Ben Saïd B, Sassolas B, et al. Prise en charge du drug reaction with eosinophilia and systemic symptoms (DRESS). Ann Dermatol Venereol. 2010;137(11):703–708. doi:10.1016/j.annder.2010.04.024
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.