Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 16
A Systematic Literature Review of the Humanistic Burden of COPD
Authors Hurst JR , Siddiqui MK , Singh B, Varghese P, Holmgren U , de Nigris E
Received 15 December 2020
Accepted for publication 1 April 2021
Published 10 May 2021 Volume 2021:16 Pages 1303—1314
DOI https://doi.org/10.2147/COPD.S296696
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Russell
John R Hurst,1 Mohd Kashif Siddiqui,2 Barinder Singh,3 Precil Varghese,4 Ulf Holmgren,5 Enrico de Nigris6
1UCL Respiratory, University College London, London, UK; 2HEOR and RWE Analytics, Regulatory Access, Parexel International Ltd, Mohali, India; 3HEOR Evidence Evaluation, Parexel International Ltd, Mohali, India; 4Biopharmaceuticals Medical, Respiratory and Immunology, AstraZeneca, Gothenburg, MD, USA; 5Real World Science and Digital, Biopharmaceutical Medical, AstraZeneca, Gothenburg, Sweden; 6Global Product and Portfolio Strategy, AstraZeneca, Cambridge, UK
Correspondence: John R Hurst
UCL Respiratory, Royal Free Campus, London, NW3 2QG, UK
Tel +44 203 108 7761
Email [email protected]
Background: Chronic obstructive pulmonary disease (COPD) is a leading cause of morbidity and mortality worldwide, causing substantial economic and social burden.
Objective: This review assessed the patient-reported humanistic burden associated with moderate to very severe COPD, specifically the impact on health-related quality of life (HRQoL), symptoms, limitations in daily life, and emotional implications, through the use of HRQoL instruments.
Methods: A systematic review was conducted to retrieve relevant clinical data from published literature using a representative sample of countries where healthcare systems provide wide availability of COPD medications and/or universal coverage includes respiratory medicines (Australia, Canada, China, France, Germany, Italy, Spain, the UK, and the USA). The primary inclusion criteria were patients with moderate to very severe COPD. HRQoL was quantified with non-disease-specific and disease-specific questionnaires.
Results: In total, 82 studies from 95 publications presented HRQoL data from patients with moderate to very severe COPD. Patient-reported HRQoL declined with worsening airflow limitation, advancing GOLD group, and increasing exacerbation frequency. Both increasing frequency of hospitalization for COPD exacerbations and recurrent hospitalization adversely impacted HRQoL. Comorbidity incidence was higher in patients with increased airflow limitation. It was associated with a further decline in HRQoL and increased depression and anxiety, particularly as disease-associated pain worsened. Physical activity improved HRQoL over time.
Conclusion: This review highlighted the impact of exacerbations and associated hospitalizations on the humanistic burden of COPD. These findings underline the importance of managing COPD actively, including prompt and appropriate use of pharmacological and non-pharmacological therapies that can improve symptoms and reduce the risk of exacerbations, thereby lessening the humanistic burden. Future reviews could consider a broader range of countries and publications to further assess the humanistic impact of COPD in low- and middle-income economies.
Keywords: chronic obstructive pulmonary disease, quality of life, humanistic burden, patient-reported outcomes
Background
Persistent respiratory symptoms and airflow limitation characterize chronic obstructive pulmonary disease (COPD).1 It is a leading cause of both morbidity and mortality worldwide, which leads to a substantial economic and social burden.1,2 In 2017, there were approximately 300 million cases of COPD reported globally,3 with approximately 3.2 million COPD-related deaths,4 ranking the disease seventh in a global list of causes of disability,4 and third in the leading global causes of death.5
Risk factors for COPD include tobacco smoking, environmental factors (such as air pollution and a reduction in air quality due to the burning of biomass fuels), and genetic susceptibility.6,7 The burden of COPD is projected to increase in the coming decades due to continued exposure to environmental COPD risk factors and an aging population.8
Currently available treatments are directed toward improving symptoms, functional capacity, and quality of life while reducing the COPD exacerbation risk. Stable COPD is typically managed using non-pharmacological means, including smoking cessation, increasing physical activity (including pulmonary rehabilitation), other lifestyle changes, and pharmacological therapy.1
The cornerstones of pharmacological therapy for COPD are long-acting bronchodilators (long-acting muscarinic antagonists and long-acting β2 agonists), which function to relax the smooth muscle of the airways and reduce lung hyperinflation. Together, these can be used individually or in combination with inhaled corticosteroids (ICS) as dual or triple therapy.1 ICS target the inflammatory aspects of COPD, and the magnitude of their effect can be predicted by measuring blood eosinophil levels. Triple therapy is typically reserved for patients with a high symptom burden and a high risk of exacerbations despite previous combination therapies.1,9
The objective of this systematic literature review (SLR) was to further the understanding of the humanistic burden of moderate to very severe COPD, with no restrictions on interventions or comparators, using health-related quality of life (HRQoL) instruments, and examining the impact of symptoms, limitations in daily life, emotional implications, and stress on individuals affected. The SLR was based on data from non-interventional, cohort, case-control and registry/database studies conducted in nine countries (Australia, Canada, China, France, Germany, Italy, Spain, the UK, and the USA).
Methods
Identification of Studies
An SLR was conducted to retrieve relevant clinical data from published literature. Searches of Embase®, MEDLINE®, and MEDLINE® In-Process were run from January 1 2006 until March 30 2020; only articles published in English were included. Bibliographic searching of selected Cochrane reviews and/or systematic reviews, identified during the screening, was conducted to identify any additional published literature not retrieved through previous database searches. The search strategies are shown in Tables S1–3.
Additionally, abstracts from the American College of Chest Physicians, the American Thoracic Society, the European Respiratory Society, the International Society for Quality of Life Research, and the International Society for Pharmacoeconomics and Outcomes Research conference proceedings from 2018 to 2020 were hand searched.
Due to the large amount of data identified, the studies included in the SLR were limited to nine countries; Australia, Canada, China, France, Germany, Italy, Spain, the UK, and the USA. These countries were selected to provide a representative sample of countries across Europe, Asia and North America. A further criterium for inclusion was that the country’s healthcare system provides wide access to COPD medications and/or has universal healthcare coverage that includes respiratory medicines.
Studies examined included patients ≥40 years of age with moderate to very severe COPD (% predicted forced expiratory volume in 1 second [FEV1] ≤80%), with no restrictions on sex, race, interventions, or comparators; data for patients with mild COPD were excluded. The selection criteria of the studies are summarized in Table 1. Literature reviews and previous systematic reviews were excluded in order to focus solely on primary data sources.
 |
Table 1 PICOS for the Inclusion of Studies in the Humanistic Burden Review |
Data Collection and Extraction Phase
For the first pass, citations were screened by a single reviewer based on the abstract supplied with each citation; an independent reviewer conducted a quality check (QC). Citations that did not match the eligibility criteria were excluded; where unclear, citations were included. Duplicates of citations (due to overlap in the coverage of the databases) were also excluded.
For the second pass, the eligibility criteria were applied to the full-text citations. Each full-text was screened by a single reviewer, followed by an independent QC. The data presented in the studies included after this stage were extracted to data extraction grids by a single reviewer to ensure that data were extracted uniformly and were comparable across trials. A further independent QC was then conducted. Where a single study was described by more than one publication, the data were compiled into a single entry in the data extraction sheet to avoid duplication.
Appraisal/Grading of Included Studies
A critical appraisal was conducted using 10 criteria previously described by Gill and Feinstein10 and further modified by Moons et al.11 The number of studies complying with each specific criterion was counted. A summary score (number of criteria fulfilled/total number of criteria) was calculated, indicating how well each study performed on the respective criteria, ranging from 0 (complying with none of the criteria) to 100 (complying with all the criteria). This information is summarized in Table S5.
HRQoL and Symptoms Questionnaires
The included studies used a range of patient-reported HRQoL data (Table 2) from the disease-specific St. George’s Respiratory Questionnaire (SGRQ), the COPD Assessment Test™ (CAT), the Clinical COPD Questionnaire (CCQ), the Chronic Respiratory Disease Questionnaire (CRQ), the Medical Research Council dyspnea scale (MRC), and the Exacerbations of Chronic Pulmonary Disease Tool (EXACT). Additionally, several non-disease-specific questionnaires reported HRQoL data (Table 2): the 36-item short-form survey (SF-36), 12-item short-form survey (SF-12), and EuroQol five dimensions visual analog scale (EQ-5D VAS).
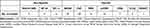 |
Table 2 Tools Used to Assess the HRQoL Across Included Studies |
Assessments
Disease severity was assessed based on airflow limitation, exacerbations, physical activity, and comorbidities.
Airflow Limitation
Disease severity in COPD is most commonly defined by the degree of airflow limitation, measured by the percentage of predicted post-bronchodilator FEV1, and is classified into four stages by GOLD.1
COPD Stratified by GOLD Groups A–D
GOLD groups A–D are used to classify patients based on symptom burden (through the assessment of dyspnea using a modified MRC scale [mMRC] or symptoms using CAT) and exacerbation history (previous history of moderate or severe exacerbations) to aid treatment decisions. Symptom burden is lower in GOLD groups A and C (mMRC 0–1, CAT <10) compared with GOLD groups B and D (mMRC ≥2, CAT ≥10), and exacerbation risk is lower in GOLD groups A and B (0/1 exacerbation event) compared with GOLD groups C and D (≥1 exacerbation event leading to hospitalization or ≥2 that did not).1
Exacerbations and Hospitalization
The most recent GOLD report defines COPD exacerbations as an acute worsening of respiratory symptoms that requires additional therapy and categorizes them as mild, moderate, or severe.1 Mild exacerbation events may be managed with an increase in short-acting rescue medication but are often not reported in clinical practice or clinical trials; moderate exacerbations require treatment with short-acting rescue medication plus antibiotics and/or oral steroids, and severe exacerbations require treatment in the emergency room or hospitalization (and may lead to death).12
Physical Activity
Physical activity was commonly measured as the physical component of non-disease-specific questionnaires such as the SF-36 and SF-12, where a physical health composite score (PCS) can be determined from the individual domains.
Comorbidities
Physical comorbid diseases were measured similarly to physical activity, as the PCS of non-disease-specific questionnaires, and mental comorbidities used the mental health composite score (MCS) of non-disease-specific questionnaires.
Results
Study Selection
The initial database searches identified 17,708 publications, of which 2740 were subsequently removed due to duplication. Screening of article titles and abstracts reduced the number of eligible publications to 2874, and bibliographic searching identified a further two citations; following review of the full articles, a further 2754 publications were excluded. In total, 122 studies were identified and, after linking, 95 publications reporting data from 82 studies were included in the review (Figure 1).
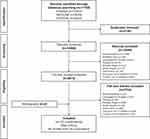 |
Figure 1 Flow of studies through the humanistic burden SLR. Abbreviation: SLR, systematic literature review. |
Study Characteristics
The studies included either non-disease-specific or disease-specific HRQoL data. The data were predominantly reported in cross-sectional (40 studies) or prospective observational studies (33 studies); 50 studies were multicenter, 18 studies were single-center, and the setting could not be ascertained in the remaining 14 studies.
The majority of studies in the review were conducted in the USA and Spain (19 studies each), followed by the UK and China (11 studies each). Studies included in the review reported HRQoL primarily using SGRQ followed by CAT, MRC/mMRC, SF-12, SF-36, and EQ-5D VAS (Table 2). The patient numbers varied widely between studies ranging from 14–10,711 patients13,14 (Table S4).
The mean age of patients was reported by 65 studies and ranged from 57 to 76 years of age. Patient characteristics are summarized in Table S4.
Critical Appraisal of Studies
Only 6 studies (7%) provided a definition of quality of life (QoL, Table 3), while 72 studies (88%) explicitly stated the domains constituting QoL. Thirteen studies (16%) reported why the specific measurement was chosen. Forty-seven studies (57%) assessed QoL with a single-item instrument or with a composite score of multiple-item tools to provide an overall score. Five studies (6%) allowed patients to self-rate their perceived QoL. Seven studies (9%) distinguished between overall QoL and HRQoL. None of the studies included provided a way for the respondents to select supplemental items important to them. However, one study (1%) used an instrument allowing respondents to rate the importance of respective items in the instrument. Summary scores for individual studies ranged from 0 to 62.5, with a median score of 25 (quartile 1=12.5; quartile 3=25). A score of 100 indicated compliance with all ten criteria. Only 4 studies had a summary score of 50 or higher.
 |
Table 3 Summary of Studies Meeting and Adhering to HRQoL Criteria |
Airflow Limitation
Studies reported the effects of airflow limitation on HRQoL using both disease-specific and non-disease-specific questionnaires, primarily using SGRQ followed by CAT, mMRC, SF-12, SF-36, and EQ-5D–VAS (Table 2).15–37 Overall, the highest SGRQ values (greatest impairment) were reported in patients with severe/very severe airflow limitation compared with other patients.20,24,35 Vaz Fragoso et al showed SGRQ total score was higher in patients with severe COPD compared with patients with moderate COPD (41.8 [95% confidence interval (CI) 39.0–44.7] vs 30.0 [95% CI 26.6–33.3]).24 Further data revealed a weak positive correlation between CAT score and severity of airflow obstruction.15,26,28
A large body of evidence across all nine countries and all instruments showed that, in general, the HRQoL of patients with COPD deteriorated with increased severity of airflow limitation. However, there was a wide variation between individual patients.18,19,25,27,38–40
COPD Stratified by GOLD Groups A–D
A study by Lopez-Campos used GOLD groups defined by MRC dyspnea score to study the relationship between the GOLD group and HRQoL (CAT score).41 CAT score was highest for GOLD D patients (high symptom burden/high exacerbation risk, 21.8), followed by GOLD B (high symptom burden/low exacerbation risk, 18.2; p<0.001 vs GOLD D), GOLD C (low symptom burden/high exacerbation risk, 17.6) then GOLD A (low symptom burden/low exacerbation risk, 12.7; p<0.001 vs GOLD B; Figure 2); this indicated that both symptom burden and exacerbation risk had a negative impact on HRQoL.41 Patients who moved from GOLD B to D had significantly higher SGRQ total score and CAT score at baseline than patients who remained in GOLD group B at follow-up (SGRQ total score 50.0 vs 40.1, p=0.019; CAT score 21.0 vs 14.0, p=0.006), indicating a worsening in HRQoL. At 1-year follow-up, patients who had experienced a moderate to severe exacerbation and progressed to GOLD D reported significantly worse CAT score than those who had not (20.0 vs 15.5, p=0.018), suggesting that exacerbations increase symptom burden and reduce HRQoL.42 Patients categorized as having a high symptom burden (GOLD B and D) had higher SGRQ total scores than those with a low symptom burden (GOLD A and C), highlighting the impact on HRQoL.43 Further to this, when assessed using CRQ, HRQoL was significantly better for patients in GOLD A and C compared with GOLD B and D.44 GOLD B patients have also been shown to have lower mean SF-36 PCS and MCS compared with GOLD C patients,45 providing further evidence that symptomatic patients have a reduced HRQoL compared with patients with a low symptom burden.
 |
Figure 2 Mean CAT scores segregated according to GOLD stage, exacerbation history, and comorbidities. Adapted from Lopez-Campos JL, et al. Evaluation of the COPD Assessment Test and GOLD patient types: a cross-sectional analysis. Int J Chron Obstruct Pulmon Dis. 2015;10:975–984. Dove Medical Press Limited.41 Abbreviations: CAT, COPD Assessment Test; GOLD, Global Initiative for Chronic Obstructive Lung Disease; NS, not significant. |
The included studies showed that the greatest impact on HRQoL was in patients with high symptom burden and, in particular, patients categorized as GOLD D.
Exacerbations and Hospitalization
CAT scores were strongly associated with annual exacerbation frequency46 and increased as the number of exacerbations increased (Figure 2).41 However, the CAT score was not associated with increased hospitalization risk.47 The baseline severity of airflow limitation was an independent determinant for increased CAT score during severe exacerbation (p=0.013). Patients with recurrent hospitalizations showed slower recovery compared with patients hospitalized less frequently over a 3-month observational period.48 Fernández-García et al reported that patients with a hospital stay of ≥7 days had worse CAT scores than patients with a hospital stay of <7 days (20.1 vs 18; p=0.02).32
Bourbeau et al assessed patients with moderate to very severe COPD (mean pre-bronchodilator FEV1 of 45% predicted) to evaluate the impact of exacerbations upon HRQoL.38 Exacerbation events of any severity were associated with statistically significant decreases in the mean changes in SGRQ activity and impact domains at onset, during the first and second weeks post-exacerbation. A clinically significant deterioration in SGRQ impact scores (an increase in score of ≥4 from baseline) was seen in 71% of patients at the onset of an exacerbation, decreasing to 55% at 1 week post-exacerbation and again to 37% at 2 weeks post-exacerbation.38
Assessment of patients over 6 months indicated that the number of exacerbations was associated with HRQoL. Improvements in HRQoL were reported in patients who had experienced either no exacerbations (SGRQ total score mean change of –6.2 at 1 month and –6.9 at 6 months after initiating treatment) or only one exacerbation (SGRQ total score mean change of –4.7 at 1 month and –4.2 at 6 months after initiating treatment). In contrast, HRQoL did not improve in patients who experienced ≥2 exacerbations. However, these patients’ health status remained unchanged during the 6-month study period.38 A cross-sectional study reported significantly higher SGRQ-C (a shorter, COPD-specific form of the SGRQ questionnaire) total scores in patients with recent severe vs moderate exacerbation (70.3 ± 19.9 vs 61.7 ± 20.1, p<0.001). SGRQ-C was also significantly higher in patients with very severe vs severe exacerbation (70.1 ± 21.3 vs 61.1 ± 19.0, p<0.001). Thus, increased exacerbation severity negatively affected the HRQoL.49
The frequency of hospitalization has been related to a reduction in HRQoL reported by both disease-specific and non-disease-specific questionnaires. SGRQ score was strongly associated with the number of hospitalizations, with lower scores correlating to fewer hospitalizations in the previous year.50 In a 5-year study, no changes in HRQoL were observed among patients not hospitalized for COPD exacerbations.19 In contrast, a significant decline in HRQoL was observed in patients with ≥3 hospitalizations due to an exacerbation during 5 years of follow-up.51 Similarly, the largest changes were observed among patients with ≥3 hospitalizations, determined by a large decrease in the SF-36 PCS score. However, hospitalization following an exacerbation resulted in a decline in HRQoL over the study period regardless of the initial severity of the disease.51 In terms of mortality, patients who did not survive the 5-year follow-up period (27.2%) had a higher SGRQ total score (mean 47.3 ± 16.1 vs 38.2 ± 18.2, p<0.0001) and higher incidence of severe airflow limitation (15.7% vs 3.2%) at baseline compared with patients who survived.51
Following adjustment by percentage predicted FEV1, age, comorbidities, and baseline HRQoL, a multivariate analysis found that hospitalizations were an independent predictor of the change in HRQoL when assessed by SGRQ total score (4.9 [1–2 hospitalizations, p=0.01] vs 15.3 [≥3 hospitalizations, p<0.0001]). When using the SF-36 questionnaire, the decline in physical component was independently associated with hospital admission (–2.7 with 1–2 hospitalizations [p=0.004]; –5.2 with ≥3 hospitalizations [p=0.0005] vs no hospitalizations), whereas a decline in the mental component was only an independent predictor in patients experiencing ≥3 hospitalizations (–5.0 vs no hospitalizations, p=0.01).51
Data collated in this review indicate that patients who experienced moderate to severe exacerbations, or had a history of exacerbations, had worse HRQoL than patients with stable COPD not experiencing these events. Furthermore, the number of exacerbations experienced by a patient and hospitalization frequency were correlated with a worsening in HRQoL.
Physical Activity
Changes in HRQoL in association with physical activity were reported in seven publications using SGRQ, CAT, SF-12, CCQ, and SF–36.19,34–37,51–53 A strong relationship was reported between physical activity and HRQoL, as determined by the association with the number of steps/day and SGRQ activity scores in patients who were physically active compared with those who were not.52 Ramon et al performed a pooled analysis investigating the usefulness of self-reported walking time to identify patients with COPD at high risk of inactivity and determined that self-reported walking time decreased with an increase in CAT score.53
The physical function and physical role scores of SF-36 have been shown to decrease with improved airflow limitation, indicating an improvement in HRQoL. SF-36 PCS and MCS scores declined in all categories over time, regardless of physical activity. However, the largest decline in HRQoL was observed in those patients who reported a decrease in physical activity at the 5-year follow-up.51
Overall, the body of evidence showed that increased airflow limitation is associated with greater physical overall decline. Higher levels of physical activity are associated with a positive impact on HRQoL in patients with COPD.
Comorbidities
Patients with physical comorbidities such as heart disease, diabetes,14 or anaemia,54 showed significantly impaired HRQoL compared with patients without the comorbid disease, as indicated by a decrease in the PCS of both SF-12 and SF-36, but not the MCS.14,54 An increase in CAT score was positively correlated with the number of comorbidities (15.7 with no comorbidities vs 23.1 for those patients with ≥4 comorbidities; Figure 2).41
Mental health status deteriorates with increased COPD severity;55 patients with moderate to very severe airflow limitation and comorbid mental disorders, such as depression or anxiety, had reduced HRQoL compared with patients with airflow limitation but without comorbid disease.56 Patients with greater bodily pain reported a lower HRQoL than patients with little pain (mean SF-12 MCS score 46.4 vs 54.2, p<0.0001).57 Patients with comorbid depression and anxiety have demonstrated significantly greater SGRQ total scores (55.3 for comorbid depression vs 40.4 for those without, and 61.5 for comorbid anxiety vs 40.6 for those without, p<0.05) across all sub-domains of the questionnaire.58
Two studies reported the relationship between HRQoL, airflow limitation, and sleep quality in patients with COPD. Dignani et al determined that sleep quality is associated with HRQoL and worsened with airflow limitation.18 Furthermore, Shah et al reported that sleep disturbances can lead to increased exacerbation frequency and healthcare resource utilization.59
In summary, the data found during this review indicated that comorbidities were associated with a reduction in HRQoL. In particular, mental health-related comorbidities were increasingly cited as airflow limitation severity increased, further decreasing HRQoL in patients with COPD.
Strengths and Limitations
To provide a representative sample of the worldwide burden of COPD while restricting the data to a manageable volume, the review focused on nine countries from Europe, Asia, Australasia and North America. Each included country was required to have a healthcare system that provided wide access to available COPD treatments and/or a universal coverage that included respiratory medicines. While country-specific or cultural differences were beyond the scope of the review, this is an area that could be explored with further research. China is classified by the World Bank as an upper middle-income economy, which distinguishes it from the other high-income economies in this review.60 China was included based on ongoing changes to its healthcare system such as increased public health insurance coverage.61 Inclusion was also in consideration of the exposure of individuals in China to important COPD risk factors such as tobacco smoking and air pollution related to biomass fuel usage.62 Focusing the scope of the review on specific countries potentially eliminated important data, but it also meant that the review could not report the humanistic burden in low-/middle-income countries, where the World Health Organization reports that approximately 90% of COPD-related deaths occur per annum.63 Also, only English language studies published from 2006 onwards were investigated, which may have eliminated important data from studies in other languages. Studies from prior to 2006 were deemed to be less relevant and, therefore, beyond the scope of this analysis.
There were wide variations regarding study size, COPD severity definitions, study design, and HRQoL instruments used. In addition, there may have been differences in cultural attitudes to COPD across the countries included that could have affected the assessment and reporting of HRQoL. While this makes direct comparisons difficult, all the data agree that increased COPD severity negatively impacts HRQoL.
Discussion and Conclusions
This review demonstrated that moderate to very severe COPD has a significant impact on HRQoL through increased COPD symptoms, daily life limitations, worsening mental health, and reduction in physical activity and sleep quality, resulting in a considerable humanistic burden. Moreover, a progressive increase of COPD-associated pain (potentially manifesting as comorbid depression) is likely to lead to a further decline in HRQoL,57 and patients with comorbid heart disease or diabetes had significantly impaired HRQoL when compared with patients without comorbid disease.14 Exacerbations and a decline in lung function represent a large component of the humanistic burden and require specific management to prevent and control their occurrence. Patients with lower symptom burden in GOLD A and C reported a better HRQoL than patients in GOLD B and D, who are defined as having a higher symptom burden. Subsequently, patients in GOLD D had the worst HRQoL of any GOLD group.
As there is currently no way to reverse established pathology in COPD, disease management aims to reduce the symptom burden and the risk of exacerbations and mortality, all of which have been shown to impact HRQoL negatively. Both pharmacological and non-pharmacological therapies are vital in the management of COPD. The active management of COPD can prevent exacerbation events.
This review highlights the importance of active management for patients with COPD, along with treatments that reduce the risk of exacerbations and the rate of decline in lung function while improving symptoms. Active management should be individualized to specific patient needs, and focus on both COPD and its associated comorbidities, which have an important impact on HRQoL. Pulmonary rehabilitation and lifestyle intervention, including increasing physical activity, are also a critical consideration to reduce the humanistic burden of COPD. Prompt and appropriate use of pharmacological and non-pharmacological therapies have the potential to reduce the cumulative long-term effects of exacerbations and the impact of COPD, thereby improving patient HRQoL and reducing the humanistic burden.
Future research may consider in more detail the impact of specific non-pharmacological interventions on HRQoL in COPD such as pulmonary rehabilitation, smoking cessation, domiciliary oxygen therapy, influenza/pneumococcal vaccinations and community-based multidisciplinary care, in addition to pharmacological interventions. As well as examining differences by country, expanding the scope to consider low- and middle-income economies could provide additional insights into differences in the humanistic burden of COPD that could further guide active COPD management in clinical practice.
Abbreviations
CAT, COPD Assessment Test; CCQ, Clinical COPD Questionnaire; COPD, chronic obstructive pulmonary disease; CRQ, Chronic Respiratory Questionnaire; EQ-5D VAS, EuroQol five dimensions questionnaire visual analog scale; EXACT, EXAcerbations of Chronic pulmonary disease Tool; FEV1, forced expiratory volume in 1 second; GOLD, Global Initiative for Chronic Obstructive Lung Disease; HRQoL, health-related quality of life; ICS, with inhaled corticosteroids; mMRC, modified Medical Research Council Dyspnea Scale; MRC, Medical Research Council Dyspnea scale; NA, not applicable; NS, not significant; PICOS, Population, Intervention, Comparator, Outcomes, Study design; QC, quality check; SF-12, 12-item short-form survey; SF-36, 36-item short-form survey; SGRQ, St. George's Respiratory Questionnaire; SLR, systematic literature review.
Data Sharing Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Consent for Publication
All authors provide consent for publication.
Acknowledgments
We thank Meenu Verma of Parexel International for her valuable contributions to the study. This study was supported by AstraZeneca. Medical writing support, under the direction of the authors, was provided by Jake Casson, PhD, CMC Connect, McCann Health Medical Communications, funded by AstraZeneca in accordance with Good Publication Practice (GPP3) guidelines.64
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Funding
This review was supported by AstraZeneca.
Disclosure
JRH reports personal payments and payments to UCL for educational and advisory work and support to attend meetings, and grant support to UCL from pharmaceutical companies that make medicines to treat COPD, including AstraZeneca. MKS is an employee of Parexel International. BS is a former employee of Parexel International. PV, UH, and EdN are employees of AstraZeneca and hold stock and/or stock options in the company.
References
1. Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. 2021 report. 2021; Available from: https://goldcopd.org/wp-content/uploads/2020/11/GOLD-REPORT-2021-v1.0-16Nov20_WMV.pdf.
2. Lozano R, Naghavi M, Foreman K, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2095–2128. doi:10.1016/S0140-6736(12)61728-0
3. James SL, Abate D, Abate KH, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1789–1858.
4. Roth GA, Abate D, Abate KH, et al. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1736–1788.
5. World Health Organization. Burden of COPD. 2019; Available from: https://www.who.int/respiratory/copd/burden/en/.
6. Molfino NA. Genetic predisposition to accelerated decline of lung function in COPD. Int J Chron Obstruct Pulmon Dis. 2007;2(2):117.
7. Lopez AD, Shibuya K, Rao C, et al. Chronic obstructive pulmonary disease: current burden and future projections. Eur Respir J. 2006;27(2):397–412. doi:10.1183/09031936.06.00025805
8. Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3(11):e442. doi:10.1371/journal.pmed.0030442
9. Brusselle G, Price D, Gruffydd-Jones K, et al. The inevitable drift to triple therapy in COPD: an analysis of prescribing pathways in the UK. Int J Chron Obstruct Pulmon Dis. 2015;10:2207–2217. doi:10.2147/COPD.S91694
10. Gill TM, Feinstein AR. A critical appraisal of the quality of quality-of-life measurements. JAMA. 1994;272(8):619–626. doi:10.1001/jama.1994.03520080061045
11. Moons P, Van Deyk K, Budts W, De Geest S. Caliber of quality-of-life assessments in congenital heart disease: a plea for more conceptual and methodological rigor. Arch Pediatr Adolesc Med. 2004;158(11):1062–1069. doi:10.1001/archpedi.158.11.1062
12. Burge S, Wedzicha JA. COPD exacerbations: definitions and classifications. Eur Respir J. 2003;21(Supplement 41):46s–53s. doi:10.1183/09031936.03.00078002
13. Knolle M, Challis B, Pearce L, Laroche C, Pulimood T. Admission avoidance by hospital at home for exacerbations of COPD by a nurse led team in the east of England. Am J Respir Crit Care Med. 2011;183(1):1073–1449.
14. Garrido PC, de Miguel Díez J, Gutiérrez JR, et al. Negative impact of chronic obstructive pulmonary disease on the health-related quality of life of patients. Results of the EPIDEPOC study. Health Qual Life Outcomes. 2006;4(1):31. doi:10.1186/1477-7525-4-31
15. Almadana V, Sanchez J, Gómez-Bastero A, Valido A, Pavón M, Montemayor T. COPD assessment test (CAT) in the evaluation of COPD. Eur Respir J. 2012;40.
16. Chen J, Wong CK, McGhee SM, Pang PK, Yu WC. A comparison between the EQ-5D and the SF-6D in patients with chronic obstructive pulmonary disease (COPD). PLoS One. 2014;9(11):e112389. doi:10.1371/journal.pone.0112389
17. Dhamane AD, Witt EA, Su J. Associations between COPD severity and work productivity, health-related quality of life, and health care resource use: a cross-sectional analysis of national survey data. J Occup Environ Med. 2016;58(6):e191–e197. doi:10.1097/JOM.0000000000000735
18. Dignani L, Toccaceli A, Lucertini C, Petrucci C, Lancia L. Sleep and quality of life in people with COPD: a descriptive-correlational study. Clin Nurs Res. 2016;25(4):432–447. doi:10.1177/1054773815588515
19. Esteban C, Quintana JM, Egurrola M, et al. Classifying the severity of COPD: are the new severity scales better than the old? Int J Tuberc Lung Dis. 2009;13(6):783–790.
20. Joo MJ, Lee TA, Bartle B, van de Graaff WB, Weiss KB. Patterns of healthcare utilization by COPD severity: a pilot study. Lung. 2008;186(5):307–312. doi:10.1007/s00408-008-9095-5
21. Mewes R, Rief W, Kenn K, Ried J, Stenzel N. Psychological predictors for health-related quality of life and disability in persons with chronic obstructive pulmonary disease (COPD). Psychol Health. 2016;31(4):470–486. doi:10.1080/08870446.2015.1111369
22. Moro JMR-G, Izquierdo JL, Antón E, de Lucas P, Martín A, Group MS. Health-related quality of life in outpatient women with COPD in daily practice: the MUVICE Spanish study. Respir Med. 2009;103(9):1303–1312. doi:10.1016/j.rmed.2009.04.002
23. Soler-Cataluña JJ, Sauleda J, Valdés L, et al. Prevalence and perception of 24-hour symptom patterns in patients with stable chronic obstructive pulmonary disease in Spain. Arch Bronconeumol. 2016;52(6):308–315. doi:10.1016/j.arbres.2015.11.010
24. Vaz Fragoso CA, McAvay G, Van Ness PH, et al. Phenotype of spirometric impairment in an aging population. Am J Respir Crit Care Med. 2016;193(7):727–735. doi:10.1164/rccm.201508-1603OC
25. Wacker ME, Jorres RA, Karch A, et al. Assessing health-related quality of life in COPD: comparing generic and disease-specific instruments with focus on comorbidities. BMC Pulm Med. 2016;16(1):70. doi:10.1186/s12890-016-0238-9
26. Wiklund I, Berry P, Lu KX, Fang J, Fu C. The Chinese translation of COPD assessment test™ (CAT) provides a valid and reliable measurement of COPD health status in Chinese COPD patients. Am J Respir Crit Care Med. 2010;181(1).
27. Wu M, Zhao Q, Chen Y, Fu C, Xu B. Quality of life and its association with direct medical costs for COPD in urban China. Health Qual Life Outcomes. 2015;13:57. doi:10.1186/s12955-015-0241-5
28. Gupta N, Pinto L, Benedetti A, et al. The COPD assessment test: can it discriminate across COPD subpopulations? Chest. 2016;150(5):1069–1079. doi:10.1016/j.chest.2016.06.016
29. Merino M, Villoro R, Hidalgo-Vega Á, Carmona C. Health-related quality of life of patients diagnosed with COPD in extremadura, Spain: results from an observational study. Health Qual Life Outcomes. 2019;17(1):1–10. doi:10.1186/s12955-019-1244-4
30. Beaumont M, Couturaud F, Jego F, et al. Validation of the French version of the London chest activity of daily living scale and the dyspnea-12 questionnaire. Int J Chron Obstruct Pulmon Dis. 2018;13:1399–1405. doi:10.2147/COPD.S145048
31. Bonfitto I, Moniello G, Pascucci M, et al. Mood disorders in elderly patients hospitalized for acute exacerbation of COPD. J Gerontol. 2017;4:13.
32. Fernández-García S, Represas-Represas C, Ruano-Raviña A, et al. Social and clinical predictors associated with prolonged hospital stays for patients with severe exacerbation of chronic obstructive pulmonary disease. Rev Clin Esp. 2020;220(2):79–85. doi:10.1016/j.rce.2019.05.003
33. Ivziku D, Clari M, Piredda M, De Marinis MG, Matarese M. Anxiety, depression and quality of life in chronic obstructive pulmonary disease patients and caregivers: an actor–partner interdependence model analysis. Qual Life Res. 2019;28(2):461–472. doi:10.1007/s11136-018-2024-z
34. Vaske I, Kenn K, Keil DC, Rief W, Stenzel NM. Illness perceptions and coping with disease in chronic obstructive pulmonary disease: effects on health-related quality of life. J Health Psychol. 2017;22(12):1570–1581. doi:10.1177/1359105316631197
35. Xiang Y, Wong T, Tsoh J, et al. Quality of life in older patients with chronic obstructive pulmonary disease (COPD) in Hong Kong: a case‐control study. Perspect Psychiatr Care. 2015;51(2):121–127. doi:10.1111/ppc.12073
36. Yang Y, Li Q, Mao J, Mao Z. Fatigue and health‐related quality of life among patients with chronic obstructive pulmonary disease in China. Clin Respir J. 2020;14(2):109–115. doi:10.1111/crj.13107
37. Zhou Z, Zhou A, Zhao Y, Duan J, Chen P. A comparison of the assessment of health status between CCQ and CAT in a Chinese COPD clinical population: a cross-sectional analysis. Int J Chron Obstruct Pulmon Dis. 2018;13:1675. doi:10.2147/COPD.S161225
38. Bourbeau J, Ford G, Zackon H, Pinsky N, Lee J, Ruberto G. Impact on patients’ health status following early identification of a COPD exacerbation. Eur Respir J. 2007;30(5):907–913. doi:10.1183/09031936.00166606
39. Di Marco F, Verga M, Reggente M, et al. Anxiety and depression in COPD patients: the roles of gender and disease severity. Respir Med. 2006;100(10):1767–1774. doi:10.1016/j.rmed.2006.01.026
40. Yeo J, Karimova G, Bansal S. Co-morbidity in older patients with COPD–its impact on health service utilisation and quality of life, a community study. Age Ageing. 2006;35(1):33–37. doi:10.1093/ageing/afj002
41. Lopez-Campos JL, Fernandez-Villar A, Calero-Acuna C, et al. Evaluation of the COPD assessment test and GOLD patient types: a cross-sectional analysis. Int J Chron Obstruct Pulmon Dis. 2015;10:975–984. doi:10.2147/COPD.S82781
42. Lawrence PJ, Kolsum U, Gupta V, et al. Characteristics and longitudinal progression of chronic obstructive pulmonary disease in GOLD B patients. BMC Pulm Med. 2017;17(1):42. doi:10.1186/s12890-017-0384-8
43. Han MK, Muellerova H, Curran-Everett D, et al. GOLD 2011 disease severity classification in COPDGene: a prospective cohort study. Lancet Respir Med. 2013;1(1):43–50. doi:10.1016/S2213-2600(12)70044-9
44. Adams S, Fan V, Nguyen H, et al. Clinical outcomes in chronic obstructive pulmonary disease are associated with perception of dyspnea more than exacerbation risk or disease severity measured by lung function. Chest. 2012;142(4):676A. doi:10.1378/chest.1389751
45. Chen Y, Yao W, Kang J, et al. Distribution and significance of GOLD 2011 disease severity classification in patients with COPD in China: a national cross-sectional survey. Eur Respir J. 2013;42:P1870. doi:10.1183/09031936.00046013
46. Kelly J, Crowley O, Smith C, et al. Determinants of the COPD assessment test (CAT) score in clinical practice. Am J Respir Crit Care Med. 2011;183(1).
47. Sloots JM, Barton CA, Buckman J, et al. The predictive value of an adjusted COPD assessment test score on the risk of respiratory-related hospitalizations in severe COPD patients. Chron Respir Dis. 2017;14(1):72–84. doi:10.1177/1479972316687099
48. Feliz-Rodriguez D, Zudaire S, Carpio C, et al. Evolution of the COPD assessment test score during chronic obstructive pulmonary disease exacerbations: determinants and prognostic value. Can Respir J. 2013;20(5):e92–e97. doi:10.1155/2013/398120
49. Solem CT, Sun SX, Sudharshan L, Macahilig C, Katyal M, Gao X. Exacerbation-related impairment of quality of life and work productivity in severe and very severe chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2013;8:641–652. doi:10.2147/COPD.S51245
50. McKellar A, Cottrell WN, Whelan A. BODE score is a useful predictor of hospital admission in rural patients with chronic obstructive pulmonary disease. Respirology. 2008;13(3):438–443. doi:10.1111/j.1440-1843.2007.01169.x
51. Esteban C, Quintana J, Moraza J, et al. Impact of hospitalisations for exacerbations of COPD on health-related quality of life. Respir Med. 2009;103(8):1201–1208. doi:10.1016/j.rmed.2009.02.002
52. McGlone S, Venn A, Walters EH, Wood-Baker R. Physical activity, spirometry and quality-of-life in chronic obstructive pulmonary disease. COPD. 2006;3(2):83–88. doi:10.1080/15412550600651263
53. Ramon MA, Esquinas C, Barrecheguren M, et al. Self-reported daily walking time in COPD: relationship with relevant clinical and functional characteristics. Int J Chron Obstruct Pulmon Dis. 2017;12:1173–1181. doi:10.2147/COPD.S128234
54. Krishnan G, Grant BJ, Muti PC, et al. Association between anemia and quality of life in a population sample of individuals with chronic obstructive pulmonary disease. BMC Pulm Med. 2006;6:23. doi:10.1186/1471-2466-6-23
55. Menn P, Weber N, Holle R. Health-related quality of life in patients with severe COPD hospitalized for exacerbations– comparing EQ-5D, SF-12 and SGRQ. Health Qual Life Outcomes. 2010;8:39. doi:10.1186/1477-7525-8-39
56. Kühl K, Schurmann W, Rief W. Mental disorders and quality of life in COPD patients and their spouses. Int J Chron Obstruct Pulmon Dis. 2008;3(4):727–736. doi:10.2147/COPD.S3375
57. Jackson B, Coultas DB, Russo R, et al. Health impact of pain among a representative sample of outpatients with COPD. Am J Respir Crit Care Med. 2014;189.
58. Lou P, Zhu Y, Chen P, et al. Prevalence and correlations with depression, anxiety, and other features in outpatients with chronic obstructive pulmonary disease in China: a cross-sectional case control study. BMC Pulm Med. 2012;12:53. doi:10.1186/1471-2466-12-53
59. Shah A, Ayas N, Tan WC, et al. Sleep quality and nocturnal symptoms in a community-based COPD cohort. COPD. 2020;17(1):40–48. doi:10.1080/15412555.2019.1695247
60. World Bank Country and Lending Groups. 2021; Available from: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups.
61. Meng Q, Mills A, Wang L, Han Q. What can we learn from China’s health system reform? BMJ. 2019;365:l2349. doi:10.1136/bmj.l2349
62. Zhu B, Wang Y, Ming J, Chen W, Zhang L. Disease burden of COPD in China: a systematic review. Int J Chron Obstruct Pulmon Dis. 2018;13:1353–1364. doi:10.2147/COPD.S161555
63. World Health Organization. Chronic obstructive pulmonary disease (COPD). 2017. Available from: https://www.who.int/news-room/fact-sheets/detail/chronic-obstructive-pulmonary-disease-(copd).
64. Battisti WP, Wager E, Baltzer L, et al. Good publication practice for communicating company-sponsored medical research: GPP3. Ann Intern Med. 2015;163(6):461–464. doi:10.7326/M15-0288
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
