Back to Journals » Clinical Ophthalmology » Volume 14
A Survey on the Impact of COVID-19 on Lacrimal Surgery: The Asia-Pacific Perspective
Authors Nair AG , Narayanan N , Ali MJ
Received 2 September 2020
Accepted for publication 30 September 2020
Published 4 November 2020 Volume 2020:14 Pages 3789—3799
DOI https://doi.org/10.2147/OPTH.S279728
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Akshay Gopinathan Nair,1,2 Natasha Narayanan,3 Mohammad Javed Ali4
1Ophthalmic Plastic Surgery and Ocular Oncology Services, Aditya Jyot Eye Hospital, Mumbai 400 031, India; 2Advanced Eye Hospital & Institute, Navi Mumbai 400 705, India; 3Temple University, Philadelphia, PA 19122, USA; 4Govindram Seksaria Institute of Dacryology, L.V. Prasad Eye Institute, Hyderabad, Telangana 600 034, India
Correspondence: Akshay Gopinathan Nair
Ophthalmic Plastic Surgery and Ocular Oncology Services, Aditya Jyot Eye Hospital, 153 Major Parmeswaran Road, Wadala, Mumbai 400 053, India
Tel +91-22-2417 7600
Email [email protected]
Aim: To assess the impact of the COVID-19 pandemic-related lockdown on lacrimal surgery among oculoplastic surgeons in the Asia-Pacific region.
Methods: An institutional board review approved anonymous electronic survey was sent out via email to oculoplastic surgeons across the Asia-Pacific region. All responses were tabulated and analysed.
Results: A total of 259 valid responses were received. Nearly 87% of the surgeons agreed that lacrimal procedures were associated with a high risk of COVID-19 transmission. In all, at the time of taking the survey, 151/259 (58.3%) of the surgeons were not performing any lacrimal surgeries in view of the COVID-19 pandemic and 71/259 (27.4%) of the respondents were only performing emergency lacrimal surgeries. External dacryocystorhinostomy was the most commonly performed lacrimal procedure across the region and lacrimal procedures contributed to at least 25% of the income for nearly a third of the respondents. Majority of the respondents were female (52.9%), but a significantly higher proportion of male oculoplastic surgeons were still performing lacrimal surgeries during the lockdown. Over 75% of respondents indicated that resuming lacrimal procedures is important to their practice.
Conclusion: The survey showed that there was a general agreement among the surveyed oculoplastic surgeons in the Asia-Pacific region that lacrimal procedures were associated with a high risk of COVID-19 transmission and over 85% of them of had either stopped performing elective lacrimal surgeries altogether or were providing only emergent care. It is likely that not performing elective lacrimal procedures, COVID-19 has financially impacted a high percentage of the surveyed oculoplastic surgeons.
Keywords: dacryocystorhinostomy, dacryology, coronavirus, epiphora, economic impact
Introduction
In 2019, a large cluster of cases of pneumonia of unknown cause was seen in Wuhan, China.1 Subsequently, in 2020, through genomic sequencing, it was found that these cases were caused by a novel virus, which was called Severe Acute Respiratory Syndrome Coronavirus 2 (SARS‑CoV‑2) or Coronavirus (2019‑nCoV).1,2 Soon, over the course of months, Coronavirus – 2019 disease (COVID-19) spread globally and became the defining global health crisis of our time. As of July 31st, 2020, the total number of COVID-19 cases globally has exceeded 17 million with over 6,00,000 dead due to the disease. COVID-19 is particularly contagious and has airborne spread potential.2 Studies suggest that the virus stays in the air for 3 hrs and on surfaces for up to 72 hrs.3 Due to their close proximity to patients, who could be asymptomatic – ophthalmologists are at increased risk of contracting the virus.4,5 On the slit lamp, the distance between the patient and the examining ophthalmologist is less than 20 cm and even closer during other procedures such as direct ophthalmoscopy and lacrimal irrigation.2 For ophthalmologists, particularly those dealing with orbital, sinus and lacrimal surgery, the potential for virus exposure is even greater because the coronavirus resides in the nasopharynx and the upper airway. In the nasal cavity, the viral load is greater than in the throat. Creating a safe environment for patients, surgeons and ancillary staff have become difficult because commonly performed oculoplastic surgeries such as orbital decompressions, fracture repair and dacryocystorhinostomy (DCR) – both external and endoscopic are aerosol-generating procedures.4,5 Therefore, the risk of exposure and subsequent infection is higher for oculoplastic surgeons (and otolaryngologists), compared to other specialists.2,4
International ophthalmic societies and associations, especially oculoplastic surgery societies have issued guidelines on urgency of care, patient triage, social distancing, and personal protective equipment (PPE) usage when caring for patients with oculoplastic disorders during the COVID-19 pandemic.2,5,6 In the Asia-Pacific region, the Asia-Pacific Society of Ophthalmic Plastic and Reconstructive Surgery (APSOPRS), Oculoplastics Association of India (OPAI), and Philippine Society of Ophthalmic Plastic and Reconstructive Surgery (PSOPRS) had issued COVID-19 recommendations for their members.2 At the time of writing this manuscript, many countries in the Asia-Pacific region were recording daily highs for the number of newly diagnosed COVID-19 cases indicating that the peak of the disease had not yet passed.
Most guidelines issued by societies stressed on the importance of triaging and intervening only in cases that required emergent care. In lacrimal surgery, that meant intervening only in cases of dacryoceles, lacrimal abscesses, acute lacrimal drainage trauma, lacrimal sac malignancies, and infected mucopyoceles.2,6 Dacryocystorhinostomy (DCR) without any acute/chronic dacryocystitis and probing of the nasolacrimal duct for cases of congenital nasolacrimal duct obstruction were to be deferred. While knowledge of current COVID-19 guidelines will allow oculoplastic surgeons to follow the best medical and surgical practices recommended; it is not known how many oculoplastic surgeons actually implemented and followed these guidelines and how COVID-19 impacted their practices. With this background, the present study was conceptualized and conducted in an attempt to obtain data on the impact of COVID-19 on the practice of lacrimal surgery in the Asia-Pacific region.
Methods
A survey that included questions on practice patterns and trends during the COVID-19 pandemic was mailed to members of the Asia-Pacific Society of Ophthalmic Plastic and Reconstructive Surgery through an official email communication in June 2020 as well as shared on multiple groups on the cross-platform messaging application—WhatsApp. The accompanying description clearly explained the nature of the survey and its questions. It contained a hyperlink to an electronic survey hosted by a third-party website: www.surveymonkey.com. Subsequently, a reminder to take the survey was sent after 2 weeks. Prior to taking the survey, a written consent form was presented to all participants entering the survey, which clearly mentioned that participation in the survey was voluntary. They were informed that the responses will be confidential and no identifying information such as name, email address or IP address would be collected. Only after obtaining written informed consent to participate were the respondents allowed to proceed to the survey. The survey contained 18 questions, most of which, were of multiple-choice nature. Respondents were also asked questions that included demographic information of age, years of practice and practice setting. All questions required a response and the survey was anonymized and did not contain any identifying information. Institutional Review Board approval was obtained at Aditya Jyot Eye Hospital, Mumbai, India before the commencement of the study. Association between categorical variables was assessed using Fisher exact test or Chi-squared test. Continuous data were analyzed using nonparametric test, that is Mann–Whitney test. We considered a P<0.05 as statistically significant. All statistical analysis was performed with GraphPad Prism 6 (GraphPad Inc, La Jolla, CA).
Results
A total of 312 responses were received, of which 53 surgeons did not perform lacrimal procedures at all and therefore were excluded from the analysis. A total of 259 valid responses from respondents from 20 countries in the Asia-Pacific region were analyzed (Table 1). The mean age of the respondents was 45.8 years (SD: ± 9.4; range: 29 to 68). In all, 137/259 respondents were female (52.9%) and 122 were male. It was noted that 93/259 (35.9%) of all respondents had an exclusively oculoplastic practice; 158/259 (61%) performed cataract and/or refractive surgeries in addition to oculoplastic procedures and 8/259 (3.1%) practiced other ophthalmic specialties in addition to oculoplasty. The respondents were asked to quantify the number of years in practice: 61/259 (23.6%) of the respondents were in practice for less than 5 years, whereas 94/259 (36.3%) were in practice for 15 years or more (Figure 1).
 |
Table 1 Country-Wise Breakup of the Responses Received |
 |
Figure 1 Distribution of responses for number of years in practice. |
The respondents were asked to quantify the proportion that lacrimal surgeries constituted of their entire surgical volume (Figure 2): 90/259 (34.8%) indicated that lacrimal diseases constituted between 11% and 25% of their practice; 79/259 (30.5%) indicated that lacrimal diseases constituted between 26% and 50% of their practice. In our survey, 142/259 (54.8%) of the surgeons performed endoscopic lacrimal procedures; however, external DCR was the most commonly performed lacrimal procedure with (168/259) 64.9% of the responses indicating so (Figure 3). Local anesthesia with or without sedation was the most frequently employed mode of anesthesia for lacrimal procedures 152/259 (58.7%). General anesthesia was the most common form of anesthesia for the remaining 41.3% (107/259) of the respondents. The respondents were asked on an average – what percentage of their income was generated by lacrimal procedures: the most common response was between 11% and 25% with 93/250 (35.9%) responses (Figure 4). Here, 87/259 (33.6%) indicated that lacrimal procedures accounted for 10% or less of their income; and cumulatively, for 79/259 (30.5%) of the respondents, lacrimal procedures accounted for at least 26% of their total income.
 |
Figure 2 Distribution of responses quantifying the proportion of total cases that lacrimal surgeries form. |
 |
Figure 3 Distribution of responses depicting the most commonly performed lacrimal surgeries. |
 |
Figure 4 Distribution of responses quantifying the proportion of income that lacrimal surgeries generate. |
Respondents were specifically asked regarding their practice during the COVID-19 pandemic lockdown (Figure 5). 151/259 (58.3%) of the surgeons were not performing any lacrimal surgeries at the time of the survey in view of the pandemic; 71/259 (27.4%) of the respondents were only performing emergency lacrimal surgeries; 23/259 (8.9%) were performing lacrimal surgeries as before, but with additional precautions and 14/259 (5.4%) were performing lacrimal surgeries as before without additional precautions. In our survey, a majority of the respondents were female (52.9%). But a significantly high proportion of male surgeons were still operating cases during the pandemic as compared to the female respondents (50.8% vs 33.6%; p=0.005). Additionally, the mean age of the male surgeons who were operating was significantly higher than the mean age of the female surgeons who were operating (46.5 years vs 42.3 years; p=0.01).
 |
Figure 5 Distribution of responses showing the responses of surgeons regarding lacrimal surgeries during the COVID-19 pandemic. |
Those surgeons who were performing surgeries were asked the source(s) for recommendations regarding operating during the COVID-19 pandemic: 112 (43.2%) indicated that they were relying on information from local and regional ophthalmic societies; 66 (25.5%) respondents indicated that peer-reviewed medical literature was their source for guidelines and 36 (13.9%) respondents indicated that sought information from their colleagues and peers.
Respondents were asked how they felt about the following statement: Lacrimal procedures are high-risk procedures with regard to the transmission of COVID-19: 132/259 (51.0%) strongly agreed with the statement; 95/259 (36.7%) somewhat agreed and only 4/259 (1.5%) strongly disagreed with the statement (Figure 6). They were also asked how they felt about the following statement: “Resumption of lacrimal procedures is important for my overall practice”: 101/259 (39.0%) of the responding surgeons somewhat agreed with the statement and 94/259 (36.3%) of the respondents strongly agreed with the statement. The respondents were asked how they felt about the statement: “Diagnostic endoscopy/irrigation can be a risk for the physician (with regard to COVID-19 transmission)” (Figure 7). In all, 110/259 (42.5%) of the respondents agreed and 97/259 (37.5%) of surgeons strongly agreed with the statement. The final question was: “Are you aware of the Povidone Iodine protocol for lacrimal surgeries?” and 162/259 (62.6%) indicated that they were aware of this protocol; 58/259 (22.4%) were not aware and 39/259 (15%) were not sure. Figure 8 enumerates all the questions in the questionnaire.
 |
Figure 6 The responses of the surveyed surgeons to the statement, “Lacrimal procedures are high-risk procedures with regard to transmission of COVID-19.”. |
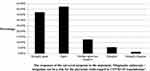 |
Figure 7 The responses of the surveyed surgeons to the statement, “Diagnostic endoscopy/irrigation can be a risk for the physician (with regard to COVID-19 transmission)”. |
 |
Figure 8a Continued. |
 |
Figure 8b List of questions in the questionnaire. |
Discussion
As a result of the COVID-19 pandemic, most governments across the world put in place lockdowns as a measure to limit the movement of people. Elective surgeries were also deferred, and most medical establishments were seeing only emergencies. The rationale behind deferring elective surgeries is that even an asymptomatic patient when placed under the stress of surgery and general anesthesia can turn a simple procedure into a complicated situation. Every surgical intervention can potentially weaken the immune system leading to complications that may require hospitalization and possibly intensive care.6,7 A survey by Nair et al showed that the majority of ophthalmologists were not seeing patients during the COVID‑19 pandemic lockdown, with near‑total cessation of elective surgeries. Emergency services were still being attended to by 27.5% of ophthalmologists who responded. Most of the responding ophthalmologists were unclear about when and how to resume surgeries upon easing off of the COVID‑19-related restrictions.8
In our survey, the mean age of the male surgeons who were operating was significantly higher than the mean age of the female surgeons who were performing lacrimal surgeries. This is extremely relevant with the background knowledge that while men and women have the same prevalence, men with COVID-19 are more at risk for worse outcomes and death.9 Additionally, of all the cases of physician deaths from COVID-19 associated with front-line work, 90% of the deceased physicians were male.10
Referrals for epiphora form a significant portion of patients seen at oculoplastic clinics. Das et al diagnosed 20,102 patients with lacrimal drainage disorders across a network of eye hospitals in India between 2013 and 2017. In all, 69.1% of these patients presented with epiphora as their presenting complaint. Of these, 51.6% were primary acquired nasolacrimal duct obstruction and 26.8% were congenital nasolacrimal duct obstruction—indicating that patients requiring surgical intervention formed a significant chunk of the lacrimal practice.11 Tan and colleagues conducted a study to assess the prevalence of eyelid, lacrimal, orbital conditions in a tertiary care hospital.12 Over an 8-month period, 623 patients were seen over 906 visits. It was reported that 121 cases of lacrimal system-related conditions were seen, making up 16.3% of the total cases. It was also reported that lacrimal surgeries comprised 13.1% of all oculoplastic surgeries performed. In contrast, in our survey, 90/259 (34.8%) indicated that lacrimal diseases constituted between 11% and 25% of their practice. However, there are variations seen here: lacrimal diseases constituted over 25% of the surgical volume for a combined total of 43.2% of the surveyed surgeons. This corresponds with the reported income generated by lacrimal surgeries. 93/259 (35.91%) indicated that lacrimal surgeries accounted for 11–25% of the total income generated from surgeries. For nearly a third of the respondents, lacrimal surgeries accounted for more than 25% of their income. Having a higher proportion of income generated from lacrimal surgeries was not found to be associated with whether the surgeon was performing lacrimal surgeries during the lockdown (p=0.4).
In all - 58.3% of the surgeons were not performing any lacrimal surgeries at the time of the survey with 27.4% of the respondents were performing only emergency lacrimal procedures. On further analysis, it was noted that of all the surgeons who indicated that lacrimal surgeries generated at least 25% or more of their income prior to the lockdown, 57.3% were not performing any lacrimal surgeries during the COVID pandemic. These figures suggest that a fairly large proportion of oculoplastic surgeons’ incomes were significantly affected due to the COVID-19 situation. This is validated by 195/259 (75.3%) of the respondents agreeing with the statement: “Resumption of lacrimal procedures is important for my overall practice.”
In this survey, 54.8% of the respondents said that they performed endoscopic lacrimal procedures; however, external DCR was the most common lacrimal surgery performed for 64.9% of the respondents from the Asia-Pacific region. In contrast, a survey conducted in 2015 among Indian oculoplastic surgeons showed that 24% of them were trained in and could perform endoscopic procedures but 86% chose external DCR as their preferred surgical treatment in NLDO.13 A survey of the members of the American Society of Ophthalmic Plastic and Reconstructive Surgeons (ASOPRS) in 2010 showed a similar trend: 83% of the respondents preferred the external approach for performing a DCR.14 Barmettler et al reported in a similar survey of ASOPRS members in 2012 that a significantly higher proportion of surgeons offered external DCR as opposed to those who offered endonasal DCR.15 Most COVID-19 guidelines indicate that routine DCRs should be deferred till the decline of the pandemic. However, for indications that may require it, it is preferable to use the external route.6 The nasal tissues have demonstrated shedding of SARS-CoV-2 virus, and nasal interventions are potential aerosol generators.16–18 This places lacrimal surgeons at a high risk for virus transmission. This risk can be compounded while performing endoscopic procedures due to the face-to-face position with patients during examination and sneezing and coughing that can be induced by the procedure.18 In our survey, most oculoplastic surgeons recognized this increased risk as 87.6% of the respondents agreed in some form with the statement: ‘Lacrimal procedures are high-risk procedures with regard to the transmission of COVID-19ʹ and 79.9% agreed that diagnostic endoscopy/irrigation can be a risk for the physician with regard to COVID-19 transmission.
Another collateral victim of the COVID-19 pandemic is ophthalmology training. A survey by Mishra et al showed that 80.7% (578/716) of the surveyed ophthalmology trainees felt that the COVID-19 pandemic lockdown had negatively impacted their surgical training.19 In the United States, since COVID cases were reported in each of the 50 states across the country, many training hospitals have responded uniformly: they have reduced their nonessential surgery volume, and are performing only surgeries that are emergent, urgent, or time sensitive.20 In 2020, it is likely that most ophthalmology trainees—residents and fellows, will not be able to fulfil their clinical rotations, complete the minimum required surgical cases and participate in non-operative patient care. Many have already been deputed to emergency medical services and deployed on COVID-19 duty. The most affected will be those in their ultimate or penultimate years of training. Program directors need to be sensitive to the fact that the degree of impact will be inversely correlated to the length of the training program. Six months of reduced clinical activity and surgical training for a first-year resident in a 3-year ophthalmology residency program can be compensated later on in the program. However, in comparison, a 3-month-long loss of surgical training for an oculoplastics fellow who in the last 6 months of a 15 or 24-month long fellowship program is potentially detrimental.21
There is growing evidence that suggests that the use of povidone-iodine on the sino-nasal and oral mucosa may disrupt the SARS-CoV-2 transmission.22–25 There are multiple factors why povidone-iodine can be used safely – primarily low resistance of the virus to povidone-iodine and its excellent safety profile. In addition to the use of povidone-iodine, combined multi-pronged approach starting from screening, triaging and testing strategies, utilization of personal protection equipment and surgical precautions to avoid aerosol creation have been recommended.26 In all, 162/259 (62.55%) of the respondents were aware of the povidone-iodine protocol suggested for lacrimal surgeries; indicating a reasonably high level of information dissemination.
The COVID-19 pandemic represents unprecedented medical and economic challenge healthcare systems around the globe. In many instances, without sustained governmental support, almost all hospitals, particularly smaller ones, will experience financial difficulties.27 The loss of revenue, unpredictability and uncertainty over the resumption of elective surgeries and the fear of getting oneself and one’s family members infected are factors that can affect the mental well-being of physicians.28 In response to the pandemic, recommendations were issued by different oculoplastic/ophthalmic societies suggesting changes to surgical practice to minimize the effect of the COVID-19 pandemic. This survey attempts to quantify the extent to which oculoplastic surgeons have been affected by the COVID-19 pandemic – specifically by the temporary cessation of lacrimal surgeries. Our survey indicates that lacrimal and other endoscopic procedures are recognized as high-risk procedures by oculoplastic surgeons; and such interventions are now being performed in extremely rare circumstances across the Asia-Pacific region which is still in the midst of the COVID-19 pandemic.
Funding
There is no funding to report.
Disclosure
Akshay Gopinathan Nair has received lecture fees from Carl Zeiss Meditec, outside the submitted work. He serves as a consultant for HelpMeSee Inc. Mohammad Javed Ali receives royalties from Springer for the 2nd edition of the textbook “Principles and Practice of Lacrimal Surgery” and treatise “Atlas of Lacrimal Drainage Disorders.” The authors report no other potential conflicts of interest for this work.
References
1. Wang C, Horby PW, Hayden FG, Gao GF. A novel coronavirus outbreak of global health concern. Lancet. 2020;395(10223):
2. Nyugen AX, Gervasio KA, Wu AY. COVID-19 recommendations from ophthalmic and plastic reconstructive surgery societies worldwide. Ophthalmic Plast Reconstr Surg. 2020;36(4):334–345.
3. van Doremalen N, Bushmaker T, Morris DH, et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020;382:1564–1567. doi:10.1056/NEJMc2004973
4. Vukkadala N, Qian ZJ, Holsinger FC, et al. In Response to COVID-19 and the otolaryngologist: preliminary evidence-based review. Laryngoscope. 2020;130(10). doi:10.1002/lary.28672
5. Sengupta S, Honavar SG, Sachdev MS, et al. Writing Committee on behalf of the All India Ophthalmological Society - Indian Journal of Ophthalmology Expert Group for COVID-19 Practice Guidelines. All India Ophthalmological Society – indian Journal of Ophthalmology consensus statement on preferred practices during the COVID-19 pandemic. Indian J Ophthalmol. 2020;68:711–724.
6. Ali MJ, Hegde R, Nair AG, et al. All India Ophthalmological Society - Oculoplastics Association of India consensus statement on preferred practices in oculoplasty and lacrimal surgery during the COVID-19 pandemic. Indian J Ophthalmol. 2020;68:974–980. doi:10.4103/ijo.IJO_1415_20
7. Chadi SA, Guidolin K, Caycedo‑Marulanda A, et al. Current evidence for minimally invasive surgery during the COVID‑19 pandemic and risk mitigation strategies: a narrative review. Ann Surg. 2020;272(2):e118–e124. doi:10.1097/SLA.0000000000004010
8. Nair AG, Gandhi RA, Natarajan S. Effect of COVID-19 related lockdown on ophthalmic practice and patient care in India: results of a survey. Indian J Ophthalmol. 2020;68:725–730. doi:10.4103/ijo.IJO_797_20
9. Jin JM, Bai P, He W, et al. Gender differences in patients with COVID-19: focus on severity and mortality. Front Public Health. 2020;8:152. doi:10.3389/fpubh.2020.00152
10. Ing EB, Xu QA, Salimi A, Torun N. Physician deaths from corona virus (COVID-19) disease. Occup Med (Lond). 2020;70:370–374. doi:10.1093/occmed/kqaa088
11. Das AV, Rath S, Naik MN, Ali MJ. The incidence of lacrimal drainage disorders across a tertiary eye care network: customization of an indigenously developed electronic medical record system—eyeSmart. Ophthalmic Plast Reconstr Surg. 2019;35:354–356.
12. Tan MCJ, Young S, Amrith S, Sundar G. Epidemiology of oculoplastic conditions: the singapore experience. Orbit. 2012;31:107–113. doi:10.3109/01676830.2011.638095
13. Nair AG, Kamal S, Agarwal A. Indian Survey on Practice Patterns of Lacrimal and Eyelid Disorders (iSUPPLE) report 2: mitomycin-C and lacrimal stents in dacryocystorhinostomy. J Craniofac Surg. 2016;27:2015–2019. doi:10.1097/SCS.0000000000003102
14. Nagi KS, Meyer DR. Utilization patterns for diagnostic imaging in the evaluation of epiphora due to lacrimal obstruction: a national survey. Ophthal Plast Reconstr Surg. 2010;26:168–171. doi:10.1097/IOP.0b013e3181b8c747
15. Barmettler A, Ehrlich JR, Lelli G
16. Zou L, Ruan F, Huang M, et al. SARS-CoV-2 viral load in upper respiratory specimens of infected patients. N Engl J Med. 2020;382:1177–1179. doi:10.1056/NEJMc2001737
17. De Luca P, Scarpa A, Ralli M, et al. Nasal, pharyngeal and laryngeal endoscopy procedures during COVID-19 pandemic: available recommendations from national and international societies. Eur Arch Otorhinolaryngol. 2020;277(7):2151–2153. doi:10.1007/s00405-020-06028-1
18. Ali MJ. Coronavirus Disease 2019 (COVID-19) pandemic and lacrimal practice: diagnostic and therapeutic nasal endoscopy and dacryoendoscopy. Ophthalmic Plast Reconstr Surg. 2020;36:417–418. doi:10.1097/IOP.0000000000001756
19. Mishra D, Nair AG, Gandhi RA, et al. The impact of COVID-19 related lockdown on ophthalmology training programs in India—outcomes of a survey. Indian J Ophthalmol. 2020;68:999–1004. doi:10.4103/ijo.IJO_1067_20
20. Bambakidis NC, Tomei KL. Impact of COVID-19 on neurosurgery resident training and education. J Neurosurg. 2020;133(1):10–11. doi:10.3171/2020.3.JNS20965
21. Potts JR
22. Ali MJ, Surgical A. Protocol to Mitigate the SARS-CoV-2 transmission using multifocal povidone-iodine applications in lacrimal surgeries during Coronavirus Disease 2019 (COVID-19) PANDEMIC. Ophthalmic Plast Reconstr Surg. 2020;36:416–417. doi:10.1097/IOP.0000000000001746
23. Pelletier JS, Tessema B, Frank S, Westover JB, Brown SM, Capriotti JA. Efficacy of povidone-iodine nasal and oral antiseptic preparations against severe Acute Respiratory Syndrome-Coronavirus 2 (SARS-CoV-2). Ear Nose Throat J. 2020;014556132095723. doi:10.1177/0145561320957237
24. Suresh V, Sharma S, Aggarwal A. Preanesthetic Povidone-Iodine gargles for patients with COVID-19. J Clin Anesth. 2020;67:110035. doi:10.1016/j.jclinane.2020.110035
25. Bidra AS, Pelletier JS, Westover JB, Frank S, Brown SM, Tessema B. Rapid in‐vitro inactivation of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS‐CoV‐2) using povidone‐iodine oral antiseptic rinse. J Prosthodont. 2020. doi:10.1111/jopr.13209
26. Ali MJ. COVID-19 pandemic and lacrimal practice: multipronged resumption strategies and getting back on our feet. Indian J Ophthalmol. 2020;68(7):1292–1299. doi:10.4103/ijo.IJO_1753_20
27. Khullar D, Bond AM, Schpero WL. COVID-19 and the financial health of US hospitals. JAMA. 2020;323:2127–2128. doi:10.1001/jama.2020.6269
28. Badahdah AM, Khamis F, Mahyijari NA. The psychological well-being of physicians during COVID-19 outbreak in Oman. Psychiatry Res. 2020;289:113053. doi:10.1016/j.psychres.2020.113053
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
