Back to Journals » International Journal of General Medicine » Volume 15
A Study of the Nursing Intervention Based on Self-Efficacy Theory for Patients After Mechanical Heart Valve Replacement: A Randomized Controlled Trial
Authors Jiang F, Lin Y , Li S, Peng Y, Huang X, Chen L
Received 14 December 2021
Accepted for publication 23 March 2022
Published 9 August 2022 Volume 2022:15 Pages 6539—6547
DOI https://doi.org/10.2147/IJGM.S353977
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Fei Jiang,1,* Yanjuan Lin,2,* Sailan Li,1 Yanchun Peng,1 Xizhen Huang,1 Liangwan Chen1
1Heart Medicine Research Center, Fujian Medical University Union Hospital, Fuzhou, 350001, Fujian, People’s Republic of China; 2Nursing Department, Fujian Medical University Union Hospital, Fuzhou, 350001, Fujian, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Yanjuan Lin, Nursing Department, Fujian Medical University Union Hospital, No. 29 of Xinquan Road, Gulou District, Fuzhou, 350001, Fujian, People’s Republic of China, Tel +86-0591-86218332, Email [email protected] Liangwan Chen, Heart Medicine Research Center, Fujian Medical University Union Hospital, No. 29 of Xinquan Road, Gulou District, Fuzhou, 350001, Fujian, People’s Republic of China, Tel +86-0591-86218449, Email [email protected]
Aim: To explore the practicability and efficiency of self-efficacy intervention on the nursing for patients after mechanical heart valve replacement (MHVR), so as to provide a theoretical and data foundation for the implementation of self-efficacy intervention in clinical practice.
Methods: This study adopted a randomized controlled trial (RCT). A total of 140 patients undergoing MHVR were randomly divided into the experimental group (normal nursing + self-efficacy intervention) or the control group (normal nursing only) based on a random number table. The primary goal was to evaluate the effect of self-efficacy theory on the self-efficacy of postoperative MHVR patients by General Self-Efficacy Scale (GSES). The secondary goal was to assess the improvement of mental health of postoperative patients as well as their pain through Symptom Checklist 90 (SCL-90) and the visual analogue scale (VAS). The incidence of infection during hospitalization was analyzed, as well as the medication compliance of patients during 3-month follow-up after discharge.
Results: Finally, 136 patients completed the whole trial. The GSES score of the experimental group was notably superior over the control group (p < 0.001), and the SCL-90 scores were lower over the control group. The VAS score of the experimental group was remarkably lower than that of the control group (p < 0.001). The incidence of infection in the experimental group was lower than that in the control group (p = 0.026). The medication compliance of the experimental group was superior to that of the control group (p = 0.030).
Conclusion: Self-efficacy intervention for patients after MHVR could mobilize their self-efficacy, enhance their postoperative medication compliance, and improve their postoperative recovery. This study provides evidence-based medicine (EBM) evidence for the application of self-efficacy theory to postoperative nursing for patients receiving MHVR.
Keywords: self-efficacy intervention, mechanical valve replacement, nursing
Introduction
For patients with severe valve disease, heart valve replacement (HVR) is considered to be an effective treatment, of which mechanical heart valve replacement (MHVR) was widely adopted in China because mechanical valves were more durable over biological ones.1 Although MHVR effectively eliminates the original valvular disease, postoperative patients must undergo lifelong anticoagulant therapy and adhere to regular follow-up. Therefore, good self-management ability was a must for patients to ensure the therapeutic effect.2–4 At the same time, attention must be paid to the risk of postoperative complications.5 In view of the physical and mental impact and economic burden caused by the surgery and postoperative nursing on postoperative patients, they may suffer from anxiety, depression, become misanthropists or even have suicidal tendencies. Hence, self-management for MHVR patients is of great importance.
Self-efficacy theory is now widely used in clinical practice.6–8 This theory was first defined by Bandura in 1977. Bandura believes that the change of a person’s behavior first requires to improve their self-efficacy, that is, self-efficacy is a prerequisite for behavior change. Randomized trials reported that self-efficacy intervention can not only improve the self-care ability of post-trauma patients, but also reduce depression among patients and improve their life quality.9 According to the theory, the improvement of self-efficacy counts on four aspects, including performance accomplishments, vicarious experience, verbal persuasion, and emotional motivation. According to self-efficacy theory, the continuous accumulation of performance achievements will increase the sense of self-confidence and expectation of success; the accumulation of personal alternative experience is accumulated through the observing the achievements of others’ behaviors; verbal persuasion increases the self-efficacy of patients by carefully explaining the treatment information to patients; emotional motivation helps to eliminate the subjective threat of patients and ease their tension.10 Self-efficacy theory has been valued positively in the areas of eczema control,7 drinking prevention,11 alleviating postpartum depression,12 and treatment of patients with obstructive sleep apnea (OSA).10 However, evidence-based medicine (EBM) evidence still lacks for the postoperative nursing of MHVR patients.
This study proposes the hypothesis that the application of self-efficacy theory to postoperative nursing of MHVR patients could improve patients’ sense of self-efficacy, anticoagulation management compliance, and mental health. Therefore, this study intended to analyze the effect of self-efficacy theory on postoperative outcomes of MHVR patients through a prospective study, and thereby providing EBM evidence for the application of self-efficacy theory in postoperative nursing of MHVR.
Methods
Sample Size Calculation
PASS15.0 software was employed to process the sample size calculation. The power (1-β) was set to 0.9, and the significance level α was set to 0.05 (a two-sided test). The results of preliminary tests indicated that the self-efficacy score of the control group was 2.2 ± 0.79 and the self-efficacy score of the test group was 2.7 ± 0.82, based on which the minimum sample size was calculated as 56 per group. Considering the sample dropout, the dropout rate was set to 20%. Finally, the selected subjects in each group were N = 70.
Subjects of the Study
This study adopted a randomized controlled trial (RCT). 140 patients who underwent MHVR from August 2020 to August 2021 at the Heart Medical Research Center of Fujian Medical University Union Hospital were selected. Participants were randomized in a 1:1 ratio to either the experimental (normal nursing + self-efficacy intervention) or control (normal nursing only) group. This study has been reviewed and approved by the Ethics Center of Fujian Medical University Union Hospital (ethical approvement number: 2020KY0127), and all participants signed informed consents.
The specific inclusion criteria were as follows: (1) Patients who received MHVR for the first time; (2) Patients aged >18 years; (3) Patients or their family willing to participate in the study; (4) Patients with clear consciousness and no mental disease. Exclusion criteria were as follows: (1) Patients with severe brain, liver and kidney and other major organ complications; (2) Patients who did not follow self-efficacy theory education during hospitalization.
Patients Grouping and Intervention Nursing
It was a two-arm parallel RCT distributed in a 1:1 ratio. The patients were randomized to either the experimental or control group (68 cases in each group), based on a random number table. Participants’ baseline information like age, sex, and mechanical valve replacement site were recorded. The experimental group underwent normal nursing and self-efficacy intervention, while the control group was treated with normal nursing only.
Contents of normal nursing were as follows: (1) Cardiac function monitoring: changes in heart rate like tachycardia, bradycardia, atrial fibrillation, and the oxygen saturation of patients were monitored. (2) Normal supplementation like diuresis and potassium. (3) Close monitoring of the patient’s respiratory function: including clearance of respiratory secretions, respiratory rate, and oxygen inhalation and atomization inhalation therapy were given to patients with respiratory sputum and poor breathing. (4) Maintenance of water and electrolyte balance. (5) Anticoagulant drugs were given to patients during hospitalization follow the doctor’s advice. International normalized ratio (INR) was monitored daily to ensure it within the normal range. (6) The patency of chest drainage tube and urinary catheter were checked at regular intervals. (7) Patients were timely urged to turn over to prevent pressure sores.
Self-efficacy interventions: (1) Mastery experience: Patients in the experimental group were given face-to-face mental guidance by nurses with qualification certificate of psychological counselor before treatment. Nurses patiently explained knowledge about MHVR and postoperative nursing tips to each patient. (2) Vicarious experience: Activities were organized on mutual help for heart valve disease (HVD) patients. (3) Verbal persuasion: Nurses could guide patients to divert attention to reduce pain. Patients could be comforted through face-to-face communication with nurses. (4) Physiological and emotional states: Nurses gave lectures on how to relieve patients’ tension and anxiety by taking deep breaths. (5) Family support: Patient’s family communicated with him/her openly and cared about the patient’s physical and mental condition. See Table 1.
 |
Table 1 Contents of Self-Efficacy Intervention |
Indicators for Evaluation
General Self-Efficacy Scale (GSES)
GSES was tested on the first day after admission and the seventh day after operation for each participant. The Chinese version of GSES translated by Wang et al13 was adopted (Supplementary Table A). The scale contains 10 items, with 1–4 scores for each grade of an item (1 score: Not at all true; 2 scores: Hardly true; 3 scores: Moderately true; 4 scores: Exactly true). The total score/10 was the final score for each participant.
Symptom Checklist 90 (SCL-90)
SCL-90 was tested on the first day after admission and the seventh day after operation for each participant (Supplementary Table B).27 The scale included 10 factors: somatization, obsessive-compulsive, interpersonal sensibility, depression, anxiety, anger-hostility, phobic anxiety, paranoid ideation, psychoticism, and additional items.14 A total of 90 items were on the checklist, with 1–5 scores each (1 score: Not At All; 2 scores: A Little Bit; 3 scores: Moderately; 4 scores: Quite A Bit; 5 scores: Extremely). The total score/90 was the final score for each participant.
Visual Analogue Scale (VAS)
VAS was evaluated on the first day and the seventh day after operation for each participant.15 The part between 0 and 10 indicates different degrees of pain (Figure 1). The larger the value, the more severe the pain. The patient was asked to mark their current pain level on the line based on their pain status (i.e. length). 0 indicates no pain, 1 to 3 are mild pain, 4 to 6 are moderate pain, and 7 to 10 are extreme pain.
 |
Figure 1 Visual analogue scale. |
Other Indicators
Infection incidence during hospitalization as well as length of hospital stay were calculated on the discharge day for each participant. In addition, each participant was subject to a 3-month follow-up. The medication status of the participants (whether participants missed doses, or took multiple doses, etc. in the previous 2 weeks) was recorded to evaluate the medication compliance of the participants. Evaluation criteria were identified to evaluate the medication compliance of participants: During the follow-up period, 3 or more times of missing doses, taking doses lower or higher than the standard ones was deemed as poor medication compliance of the participant, otherwise it was deemed as good medication compliance.16
Statistical Analysis
SPSS 26.0 statistical software was applied for data processing and analysis. PASS 15.0 was adopted for randomization as well as for power and significance level testing. Randomization was performed utilizing randomization lists. Continuous variables were in the form of mean ± standard deviation (SD), paired t-test was applied for intra-group difference test, and independent sample t-test was applied for inter-group difference test. Enumeration data were displayed as N (%), and chi-square test or Fisher’s exact test was selected for difference test method. P<0.05 indicated statistically inter- or intra-group significance.
Results
The Comparison of Baseline Data Between Two Groups
140 eligible patients undergoing MHVR were selected in this study and were randomly grouped. 70 patients for both experimental and control groups. In the experimental group, one patient had complications and another patient’s family refused to continue in the study. In the control group, 2 patients had complications. Thus, 136 participants were finally included in the study. The patients grouping routes were manifested in Figure 2.
 |
Figure 2 The routes for patients grouping. |
24 males and 44 females were included in the control group, with the average age of 50.40 ± 9.56 years old. 15 patients of them underwent mechanical aortic valve replacement (MAVR), 38 patients underwent mechanical mitral valve replacement (MMVR), and 15 patients underwent MAVR + MMVR. The left ventricular end-diastolic diameter (LVEDD) was 40.17 ± 3.05 mm, and the left ventricular end-systolic diameter (LVESD) was 31.73 ± 3.03 mm. 34 males and 34 females were included in the test group with the mean age of 49.59 ± 10.71 years old. 23 patients received MAVR, 30 patients received MMVR, and 15 patients received MAVR + MMVR. The LVEDD was 41.12 ± 2.67 mm, and the LVESD was 30.87 ± 2.23 mm. Other baseline levels were manifested in Table 2, and there was no statistical significance in baseline levels of participants between the groups.
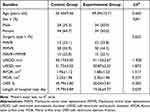 |
Table 2 The Baseline Levels of Participants |
The Comparison of GSES Between Two Groups
This study documented changes in GSES of preoperative and postoperative participants (Table 3). In the control group, the preoperative GSES (pre-GSES) was 2.52 ± 0.37 and the postoperative GSES (post-GSES) was 2.67 ± 0.43, with an intra-group statistical significance (t = −2.227, p=0.029). In the experimental group, the pre-GSES was 2.54 ± 0.49 and post-GSES was 3.16 ± 0.33, with an intra-group statistical significance (t = −8.852, p<0.001). The inter-group post-GSES was statistically significant (t = −7.424, p<0.001).
 |
Table 3 GSES Comparison |
The Comparison of SCL-90 and VAS Between Two Groups
This study recorded changes in SCL-90 of participants before and after surgery (Table 4). In the control group, preoperative SCL-90 (pre-SCL-90) was 1.69 ± 0.26 and postoperative SCL-90 (post-SCL-90) was 1.75 ± 0.26, with no intra-group significance (t = −1.299, p=0.198). In the experimental group, pre-SCL-90 was 1.61 ± 0.27 and post-SCL-90 was 1.42 ± 0.22, with an intra-group significance (t = 5.120, p<0.001). The inter-group difference in post-SCL-90 was statistically significant (t = 7.936, p<0.001). In addition, changes in VAS were documented on the first and the seventh day after surgery (Table 4). In the control group, the pre-intervention VAS (pre-VAS) was 5.47 ± 1.18 and the post-intervention VAS (post-VAS) was 3.41 ± 1.12, with an intra-group significance (t = 10.365, p<0.001). In the experimental group, the pre-VAS was 5.13 ± 1.20 and the post-VAS was 2.56 ± 1.04, with an intra-group significance (t = 12.648, p<0.001). The inter-group difference in post-VAS was statistically significant (t = 4.591, p<0.001).
 |
Table 4 SCL-90 and VAS Comparison Between Groups |
Other Indicators
The incidence of infection during the hospital stay and medication compliance during the follow-up period were evaluated (Table 5). During hospitalization, 12 patients (12/68, 17.6%) in control group and 3 patients (3/68, 4.4%) in experimental group had infection, and there was an inter-group statistical significance (X2 = NA, p=0.026). During the follow-up period, 49 patients (49/68, 72.1%) in the control group and 60 patients (60/68, 88.2%) in the test group reflected good medication compliance, and there was an inter-group statistical significance (X2 = NA, p=0.030).
 |
Table 5 Other Indicators |
Discussion
HVR is mainly divided into mechanical and bioprosthetic according to the different valve materials adopted. The European Society of Cardiology recommends bioprosthetic valve for patients over 70 years old, while mechanical valve is more recommended for younger patients, although mechanical valve means lifelong anticoagulant drug management.17 This prospective study analyzed the clinical significance of self-efficacy theory in MHVR patients and confirmed that self-efficacy intervention on the basis of normal nursing could effectively improve patients’ self-efficacy, mental health, medication compliance, and reduce the incidence of perioperative infection.
At present, self-efficacy intervention has become a supplement to many clinical disease treatments.18 People with strong self-efficacy have higher self-confidence.19 They adapt to abnormal conditions or discomfort during treatment, cooperate better with medical staff, and enjoy higher quality of life.20 In this study, MHVR patients who underwent self-efficacy intervention had a more significant improvement in self-efficacy. And the results of the SCL-90 questionnaire also proved that the mental health of the experimental group was better than that of the control group. This might be an effect of self-efficacy on mental health. McCusker et al9 reported that self-efficacy has a positive impact on the improvement of depression, which was similar to the results of this article. The reason for this result may lies in that the self-efficacy intervention emphasizes relieving the tension of hospitalized patients and relieving the stress of patients through family assistance as well as the assistance of nurses. Razurel et al21 suggested that stress or stress levels are significantly associated with depression and anxiety, and this view also supported our findings.
Patients with MHVR were at increased risk of thrombotic complications while facing INR monitoring problems,22 which seriously affected their life quality and placed a higher demand on patients’ medication compliance. The results of this study confirmed that patients’ medication compliance was significantly improved after self-efficacy intervention. The reason for this might be that patients were subject to systemic self-efficacy intervention. They fully understood MHVR, realized the importance of self-efficacy for controlling the disease progression and improving their prognosis. Thus, their self-efficacy was actively cultivated and medication compliance was enhanced. In a systematic review of the relationship between self-efficacy and medication compliance, it was stated that high levels of self-efficacy can promote medication compliance,23 which was similar to the results of this study. However, Daniali et al24 reported the effect of self-efficacy on medication compliance in patients with chronic diseases, and pointed out that there is no significant correlation between the improvement of self-efficacy and medication compliance of patients, which was different from the results of this study. The reason for this might be due to the different study subjects. In addition, postoperative infections can increase the complexity of patient’s treatment.25 Therefore, the prevention of postoperative infection, which requires constant observation and monitoring, as well as strict adherence to nursing methods, is of great importance. However, it is not always possible for the medical staff to take care of the patient, at which point patients and their caregiver become critical.26 By patients’ improving self-efficacy, strengthening the communication with medical staff, and improving initiative, the infection could be prevented and reduced. Our findings revealed that patients with self-efficacy intervention had a more advantageous incidence of infection during hospitalization, also, the VAS for pain suggested better results. The above results indicated that self-efficacy intervention could improve the postoperative recovery of patients and has a positive effect on the life quality of MHVR patients.
This study still has some limitations. First, the correlation between self-efficacy and the improvement of SCL-90 was not analyzed. Second, due to the difficulty in follow-up, the incidence rate of postoperative complications was not tracked for a long time, including infective endocarditis, thrombosis, bleeding and other events in participants.
In sum, this prospective study discusses the impact of self-efficacy intervention on the recovery of MHVR patients in the perioperative period. For patients undergoing MHVR, postoperative self-efficacy intervention could actively mobilize the patient’s self-efficacy, enhance their postoperative medication compliance, and improve their postoperative recovery. This study provides EBM evidence for the application of self-efficacy intervention to the postoperative nursing of patients undergoing MHVR.
Data Sharing Statement
The data used to support the findings of this study are included within the article.
Ethics Approval and Consent to Participate
This study was conducted in accordance with the Helsinki Declaration II and was approved by the Institutional Review Boards of Fujian Medical University Union Hospital.
Funding
This study was supported by the Project Research Project of Fujian Association for Science and Technology Innovation Think Tank (No.FJKX-A2129) and Fujian Key Laboratory of Cardio-Thoracic Surgery (Fujian Medical University).
Disclosure
The authors declare no conflicts of interest.
References
1. Zhu Z, Li C, Shen J, et al. New internet-based warfarin anticoagulation management approach after mechanical heart valve replacement: prospective, multicenter, randomized controlled trial. J Med Internet Res. 2021;23:e29529. doi:10.2196/29529
2. Roberts G, Razooqi R, Quinn S. Comparing usual care with a warfarin initiation protocol after mechanical heart valve replacement. Ann Pharmacother. 2017;51:219–225. doi:10.1177/1060028016676830
3. Zhang L, Long Y, Xiao H, et al. D-dimer to predict the clinical outcomes in patients with mechanical heart valve replacement during oral anticoagulation therapy. Int Heart J. 2019;60:631–636. doi:10.1536/ihj.18-237
4. Li R, Liang G, Xu Y, Zhuang L. Research progress of nursing human resource allocation in China. Chin Nurs Res. 2016;30:1799–1802.
5. Mve Mvondo C, Pugliese M, Ambassa JC, et al. Mechanical heart valve replacement in a low-middle income region in the modern era: midterm results from a Sub-Saharan center. Thorac Cardiovasc Surg. 2020;68:99–106. doi:10.1055/s-0038-1666873
6. Alimohammadi L, Zarei F, Mirghafourvand M. The effect of counseling based on Bandura’s self-efficacy theory on sexual self-efficacy and quality of sexual life. Women Health. 2020;60:473–486. doi:10.1080/03630242.2019.1662871
7. Cheng NS, Chau JPC, Lo SHS, et al. Effects of a self-efficacy theory-based parental education program on eczema control and parental outcomes. Pediatr Allergy Immunol. 2021;32:535–543. doi:10.1111/pai.13421
8. Tanimura C, Aoto H, Kobayashi N, et al. Effects of a self-efficacy theory-based training program for peers of patients with type 2 diabetes. Yonago Acta Med. 2020;63:282–293. doi:10.33160/yam.2020.11.006
9. McCusker J, Lambert SD, Cole MG, et al. Activation and self-efficacy in a randomized trial of a depression self-care intervention. Health Educ Behav. 2016;43:716–725. doi:10.1177/1090198116637601
10. Kim J, Oh EG, Choi M, et al. Development and evaluation of myofunctional therapy support program (MTSP) based on self-efficacy theory for patients with obstructive sleep apnea. Sleep Breath. 2020;24:1051–1058. doi:10.1007/s11325-019-01957-6
11. Kim JH, Kweon YR. Effects of a problem drinking prevention program developed based on Bandura’s self-efficacy theory in nursing students. Iran J Public Health. 2020;49:186–188.
12. Mohammadi F, Kohan S, Farzi S, Khosravi M, Heidari Z. The effect of pregnancy training classes based on bandura self-efficacy theory on postpartum depression and anxiety and type of delivery. J Educ Health Promot. 2021;10:273. doi:10.4103/jehp.jehp_105_21
13. Wang C, Liu Y. Correlation between general self-efficacy and trait anxiety, state anxiety and test anxiety. Chin J Clin Psychol. 2000;8:229–230.
14. Dang W, Xu Y, Ji J, et al. Study of the SCL-90 scale and changes in the Chinese norms. Front Psychiatry. 2020;11:524395. doi:10.3389/fpsyt.2020.524395
15. Faiz KW. [VAS–visual analog scale]. Tidsskr nor Laegeforen. 2014;134:323. Norwegian. doi:10.4045/tidsskr.13.1145
16. Sin NL, Moskowitz JT, Whooley MA. Positive affect and health behaviors across 5 years in patients with coronary heart disease: the heart and soul study. Psychosom Med. 2015;77:1058–1066. doi:10.1097/PSY.0000000000000238
17. Reineke D, Gisler F, Englberger L, Carrel T. Mechanical versus biological aortic valve replacement strategies. Expert Rev Cardiovasc Ther. 2016;14:423–430. doi:10.1586/14779072.2016.1133293
18. Song W, Wu W, Song Y. Prognostic analysis of different methods in the treatment of cervical cancer patients with lymph node metastasis. Chin J Clin Oncol Rehab. 2018;3:e2011625.
19. Arians N, Lindel K, Krisam J, et al. Prospective phase-II-study evaluating postoperative radiotherapy of cervical and endometrial cancer patients using protons - The APROVE-trial. Radiat Oncol. 2017;12(1). doi:10.1186/s13014-017-0926-5
20. Ettcheto M, Cano A, Busquets O, et al. A metabolic perspective of late onset Alzheimer’s disease. Pharmacol Res. 2019;145:104255. doi:10.1016/j.phrs.2019.104255
21. Razurel C, Kaiser B, Antonietti JP, Epiney M, Sellenet C. Relationship between perceived perinatal stress and depressive symptoms, anxiety, and parental self-efficacy in primiparous mothers and the role of social support. Women Health. 2017;57:154–172. doi:10.1080/03630242.2016.1157125
22. Zhu Z, et al. New warfarin anticoagulation management model after heart valve surgery: rationale and design of a prospective, multicentre, randomised trial to compare an internet-based warfarin anticoagulation management model with the traditional warfarin management model. BMJ Open. 2019;9:e032949. doi:10.1136/bmjopen-2019-032949
23. Nafradi L, Nakamoto K, Schulz PJ, Asnani MR. Is patient empowerment the key to promote adherence? A systematic review of the relationship between self-efficacy, health locus of control and medication adherence. PLoS One. 2017;12:e0186458. doi:10.1371/journal.pone.0186458
24. Daniali SS, Darani FM, Eslami AA, Mazaheri M. Relationship between self-efficacy and physical activity, medication adherence in chronic disease patients. Adv Biomed Res. 2017;6:63. doi:10.4103/2277-9175.190997
25. Liu X, Tao S, Ji H, et al. Risk factors for peripherally inserted central catheter (PICC)-associated infections in patients receiving chemotherapy and the preventive effect of a self-efficacy intervention program: a randomized controlled trial. Ann Palliat Med. 2021;10:9398–9405. doi:10.21037/apm-21-1848
26. Lee KC, Chao YF, Wang YM, Lin PC. A nurse-family partnership intervention to increase the self-efficacy of family caregivers and reduce catheter-associated urinary tract infection in catheterized patients. Int J Nurs Pract. 2015;21:771–779. doi:10.1111/ijn.12319
27. Wang Z. The Symptoms checklist-90. Shanghai Arch Psychiatry. 1984;2:68–70.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
