Back to Journals » Clinical Interventions in Aging » Volume 9
A single blind randomized control trial on support groups for Chinese persons with mild dementia
Authors Young D , Kwok TC , Ng P
Received 1 June 2014
Accepted for publication 9 July 2014
Published 3 December 2014 Volume 2014:9 Pages 2105—2112
DOI https://doi.org/10.2147/CIA.S68687
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Daniel KW Young,1 Timothy CY Kwok,2 Petrus YN Ng1
1Department of Social Work, Hong Kong Baptist University, Kowloon Tong, Hong Kong; 2Department of Medicine and Therapeutics, The Chinese University of Hong Kong, Shatin, Hong Kong
Purpose: Persons with mild dementia experience multiple losses and manifest depressive symptoms. This research study aimed to evaluate the effectiveness of a support group led by a social worker for Chinese persons with mild dementia.
Research methods: Participants were randomly assigned to either a ten-session support group or a control group. Standardized assessment tools were used for data collection at pretreatment and post-treatment periods by a research assistant who was kept blind to the group assignment of the participants. Upon completion of the study, 20 treatment group participants and 16 control group participants completed all assessments.
Results: At baseline, the treatment and control groups did not show any significant difference on all demographic variables, as well as on all baseline measures; over one-half (59%) of all the participants reported having depression, as assessed by a Chinese Geriatric Depression Scale score ≥8. After completing the support group, the depressive mood of the treatment group participants reduced from 8.83 (standard deviation =2.48) to 7.35 (standard deviation =2.18), which was significant (Wilcoxon signed-rank test; P=0.017, P<0.05), while the control group’s participants did not show any significant change.
Conclusion: This present study supports the efficacy and effectiveness of the support group for persons with mild dementia in Chinese society. In particular, this present study shows that a support group can reduce depressive symptoms for participants.
Keywords: support group, mild dementia, Chinese, depression
Introduction
In Hong Kong, ~8.9% persons aged 70 years or older suffer from dementia.1 There were ~70,000 persons with dementia in Hong Kong in 2006, and the number is expected to escalate to 330,000 by the year 2050.2 Among persons with dementia in Hong Kong, about 85% suffer from mild dementia.1 At present, the pharmacological treatments for mild dementia are found to have small benefits on cognitive decline.3 Mild dementia has an adverse impact on the lives of sufferers, including progressive loss of memory, increasingly impaired cognitive impairments, and an increasing inability to conduct daily living activities.4
Depression is common in dementia, and the prevalence of depression in persons with dementia is higher than in those persons without dementia.5 One research study has reported that up to one-half of persons with mild dementia manifested depressive symptoms.6 Depression has negative impacts for persons with mild dementia and their caregivers, including negative impacts on quality of life,7 functional impairment,8 increased risk of early institutionalization,9 and an increased stress level of caregivers.10 The risk and predictive factors for depression in persons with dementia are different from that for depression in persons without dementia.11 It has been suggested that depression is a psychological reaction to cognitive decline.12
While retaining an awareness of their problems, persons with mild dementia experience multiple losses, including the loss of social roles, self-esteem, self-confidence, and they have negative feelings about their illness.13 Under such stressful situations, many persons with mild dementia manifest depressive symptoms.14
Pharmacological interventions, as well as nonpharmacological interventions, are available for treating depression in dementia.15 It is recommended that nonpharmacological interventions be adopted first in treating depression among persons with mild dementia.15 Nevertheless, depression in dementia is underdiagnosed and undertreated.15,16
Recently, a support group, as one kind of nonpharmacological intervention, has been developed in the Western countries (such as in the United States, the United Kingdom, Canada, the Netherlands, and Australia) to help persons with mild dementia cope with the illness and reduce depression.4,17 A support group is generally defined as emphasizing a supportive and nurturing relationship among group participants and leaders.4,18 Many support groups are topical in nature. Group formats vary. Some allow for time with the caregiver, or a family member may be present,19 while others are intended solely for the person with dementia.20 Some groups are structured, time limited, and last for about ten sessions,21 while others are long-term open groups.22 Support groups are often led by health professionals with working experiences with persons with dementia.
Research evidence has indicated that structured and time-limited support groups for persons with mild dementia can be beneficial; the benefits include a decrease in feelings of isolation, better coping skills, an increase in self-efficacy, and a reduction in depression.18–21,23,24 However, the generalization of these research results is limited by the nonrandomized research design, as well as by cultural differences. Only one randomized control study on the support group, which was conducted in the US, supported the efficacy of the support group; it reported that the treatment group, but not the control group, showed significant improvement in terms of quality of life, self-efficacy, and depression for persons with mild dementia.17 More research studies are needed in this area, especially with respect to studies that test the efficacy of the support group in different societies and cultures.
Due to a cultural difference, Chinese persons with mild dementia in Hong Kong have somewhat different concerns regarding their cognitive decline.25 As shown in a local study, Chinese persons with mild dementia in Hong Kong expressed fear with respect to being labeled as mentally ill, losing their status within the family, feeling guilty about becoming dependent, being a family burden, and feelings of helplessness.25 These kinds of fears are due to the stigmatization of dementia and mental illness by traditional Chinese cultural values, especially Confucianism.26
Under traditional Chinese values, after experiencing cognitive decline, persons with dementia fail to perform duties that lead to a loss of face and status within the family and their social systems. After losing face, persons with dementia become devalued within the family and community, which affects their social status and relationships with family members and others. Thus, Chinese persons with mild dementia experience multiple losses, including a loss of face and social status, which leads them to experience depressive symptoms. Thus, it is important for the support group to address these needs of Chinese persons with dementia.
In Hong Kong, local studies on the effectiveness of a support group for persons with mild dementia are lacking. This present study thus aims to evaluate the positive effects of a support group for Chinese persons with mild dementia in the Hong Kong context.
Research methods
A randomized controlled study research design was adopted in the present study. Participants were recruited from three centers for elderly individuals run by nongovernment organizations. Participants who gave their consent to participate in this research project were randomly assigned to a treatment group or a control group. Standardized assessment tools were used for data collection at pretreatment and post-treatment periods by a research assistant who was kept blind to the group assignment of the participants.
Treatment and control group
The support group involved in this study was structured, time limited, and allowed participants to share on different topics. The support group lasted for ten sessions, with one session a week. Each session lasted, on average, 90 minutes. The group was small in nature, with group sizes that ranged from six to eight elderly individuals. Finally, three support groups were held at three local elderly centers so that participants could access it easily. Each support group was led by a social worker who had working experiences with persons with dementia. Promoting the understanding and acceptance of the illness, handling role adjustment, providing coping skills for memory decline, letting go of responsibilities without having guilty feelings, fostering communication skills with family caregivers, and offering emotional support for participants were important elements of this support group. Also, family caregivers were encouraged to join in for two sessions on communication skills and establishing positive relationships between participants and family caregivers. Please refer to Table 1 for the content outline of the structured support group.
  | Table 1 Session outline of the 10-week support group for persons with mild dementia |
On the other hand, participants who were assigned to the control group received standardized educational written material on dementia that provided basic information on dementia.
Subject inclusion criteria
In this study, the inclusion criteria for this study included: 1) aged 60 years or above; 2) having a diagnosis of dementia; 3) having a Mini-Mental State Examination (MMSE) score of 18 or above; 4) aware of their memory loss and had a memory complaint; and 5) were able to participate independently in a group setting. Those participants who did not receive any diagnosis of dementia were assessed by a screening tool (ie, the Hong Kong List Learning Test [HKLLT]27) as having probable dementia. The HKLLT can reliably identify elderly people who are suffering from mild dementia with satisfactory reliability and validity, and it is one of the most commonly used memory assessment tools at local major public hospitals.27 On the other hand, the cognitive ability of participants was assessed by the MMSE (Cantonese version), which had been tested with satisfactory reliability and validity.28
The ethical issues of this study were approved by the Research Committee of Hong Kong Baptist University. Data collection began and was completed in 2013.
Assessment tools
Chinese Geriatric Depression Scale (GDS)
The GDS provides an assessment of the mood changes of participants.29 The reliability and validity of the Chinese version of the GDS have been tested to be satisfactory.29 Although there have been reservations on using the GDS to assess depressive symptoms among persons with moderate to severe dementia, the GDS has been validated for assessing depressive symptoms for persons with mild dementia.30 A recent research study also provides evidence to support the use of GDS to assess the depressive symptoms of persons with mild dementia,31,32 including Chinese persons with mild dementia.33 In this study, the GDS-15, which consists of 15 items, was used to measure depressive symptoms among participants. A cut-off point of ≥5 is indicative of significant depressive symptoms in the original form,34 while a cut-off point of ≥8 has been adopted for the Chinese version of the GDS in the Hong Kong context.29 In this study, a cut-off point of ≥8 was adopted as being indicative of significant clinical depression for the Chinese participants.
Rosenberg Self-Esteem Scale (RSES) (Chinese version)
The RSES has been widely used in many countries and has been translated into many languages, including Chinese.35 It consists of ten items. Each item is rated with a score on a 4-point scale ranging from strongly agree to strongly disagree. The reliability and validity of the Chinese version of the RSES have been tested to be satisfactory.35
General Self-Efficacy scale (GSE) (Chinese version)
The GSE was used to measure the self-efficacy of the studied subjects.36 The scale has been translated into various languages, and its Chinese version has been tested with satisfactory validity and reliability.36 Each item is rated by the studied subjects on a 4-point scale. Scores are summed over the items such that higher scores indicate a higher level of self-efficacy.
Index for Managing Memory Loss (IMMEL)
The IMMEL is a checklist of coping skills designed to assess the coping skills of people with dementia.37 The IMMEL consists of six items: “I laugh about my memory problems”; “I use lists to help me remember”; “I think my memory problems are a normal part of growing older”; “I talk about my memory problems to someone that I trust”; “I get angry about my memory problems”; and “I bottle my feelings about my memory problems up”. It has a 3-point scale: 1, “never use”; 2, “occasionally use”; and 3, “often use”.
Data analyses
Descriptive statistics including frequency distribution (N) and mean scores (M) were used to report the baseline demographic and clinical characteristics of the participants. Group mean value (M) and standard deviation (SD) or count (N) and percentage (%) were used to report the GDS and other outcome assessment scores. The baseline demographic and clinical characteristics between the treatment and control group were compared using chi-squared (χ2) tests for categorical variables, and nonparametric Mann–Whitney U-tests were used for ordinal or interval scale variables due to the small sample size involved in this study. When analyzing the significant change of repeated measures of GDS and other outcome assessment scores for both the treatment and control groups, the nonparametric Wilcoxon signed-rank tests were performed. For all analyses, two-tailed P-values of <0.05 indicated statistical significance. All data were analyzed using SPSS version 21.0 (IBM Corporation, Armonk, NY, USA).
Results
A total of 46 participants were recruited; however, seven of them did not meet the inclusion criteria and were excluded. Thirty-nine subjects were randomly assigned to a treatment group or a control group. Among them, 20 subjects entered the treatment group, while 19 subjects entered the control group. Figure 1 illustrates the recruitment procedure. After the study was completed, 36 subjects (92.3%) remained and finished all the assessments.
  | Figure 1 Recruitment procedure. |
Characteristics of the research sample
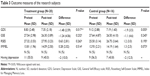
Table 2 details the demographic data and baseline measures of all participants. The mean age of the participants was 80.3 years. Just over one-half of them (56.4%; number [n]=22) were male. One-third (33.3%; n=13) did not receive any education, about one-third (30.8%; n=12) reached primary school, while 17.9% (n=7) reached the secondary school level. Over one-half of them were married (57.9%; n=22); about one-third (36.8%; n=14) were widowed, separated, or divorced; while 5.3% (n=2) were single. The majority of them (84.6%; n=33) lived with their family members; 7.7% (n=3) lived with a domestic helper, and another 7.7% (n=3) lived alone. Two-thirds of them (66.7%; n=26) received a diagnosis of dementia, while one-third (33.3%; n=13) were diagnosed as having probable dementia, as assessed by the HKLLT. Their mean MMSE score was 22.0 (SD =3.2). Over one-half (54.1%; n=13) of the participants suffered from dementia <1 year, about one-third (37.5%; n=9) suffered for 1–2 years, while the rest (8.4%; n=2) suffered for 3 years or more.
Depressive symptoms
At baseline, just over one-half (59.0%; n=23) of the participants manifested depressive symptoms as assessed by the Chinese GDS (ie, GDS ≥8). The respondents regarded their self-esteem as average, with a mean RSES score of 26.13 (SD =3.85, ranging from 16.00–37.50). The treatment and control groups did not show any significance on any of the demographic variables or on the baseline measures. Please refer to Table 2 for the data analysis.
Treatment outcomes
Table 3 summarizes the outcome measures of the participants. The results showed that support group participants exhibited a significant reduction in their depressive mood, as the mean GDS score reduced from 8.83 (SD =2.48) to 7.35 (SD =2.18) (Wilcoxon signed-rank test; P=0.017, P<0.05). However, the treatment group did not show any significant change in self-esteem, self-efficacy, and coping skills. On the other hand, the control group did not show any significant changes in the GDS score or on the other outcome assessment scores.
Discussion
This present single blind, randomized controlled study provides evidence to support the efficacy and effectiveness of a structured and time-limited support group for Chinese persons with mild dementia. Also, this present study shows that the support group is effective in reducing participants’ depressive mood.
Several established models of support groups for persons with mild dementia have been developed in Western countries. An early support group model for persons with mild dementia and their caregivers has been developed in the US.18,19 This support group model is structured with eight sessions focusing on coping with memory problems, daily living, self-esteem, relationships, as well as health, legal, and financial concerns. The Memory Club is another support group model for a person with mild dementia and their care partners that was developed in the US.20,21 This support group is structured with ten sessions and is aimed at empowering participants to problem solve and plan for the future. Circle of Care, based in Toronto, ON, Canada, is an eight-session support group for persons with mild dementia without the participation of family caregivers.23 It is structured and allows participants to share in different topics including: causation of dementia; coping with memory problems; loss; grief; and daily living skills. Unlike previous support group models, the Alzheimer’s Café in the Netherlands has been carried out to provide a relaxed café-like environment for persons with mild dementia and their family caregivers, so as to facilitate social interactions and sharing among participants.22 Participation is open-ended, allowing for ongoing participation. In fact, all of these support group models have been found to be effective in recent research studies for participants.19,21,24
All of these previously named support group models developed in Western countries share common group elements of enhancing the participants’ coping skills with memory problems, daily living skills, problem-solving skills, and better planning for the future. However, as discussed earlier, Chinese persons with mild dementia in Hong Kong have somewhat different concerns regarding their cognitive decline.25 Chinese persons with mild dementia expressed fears with being labeled as mentally ill, losing face and status within the family, experiencing guilty feelings of becoming dependent and being a family burden, and having feelings of helplessness. Thus, it is important for the support group to help participants to promote the acceptance of illness, handle role adjustment, develop a positive lifestyle, let go of responsibilities without feeling guilty, and improve their relationship with family caregivers. Moreover, Chinese elderly individuals were afraid of sharing their difficulties with family members, as family members tended to limit the activities that participants could continue to perform, and they valued the opportunity to share with others facing similar problems.25 Thus, it is important for the support group to allow participants to share in different topics without the presence of family caregivers. Also, it is important for the support group to facilitate emotional support among the participants who share similar difficulties that are encountered in daily living. By receiving emotional support from others, participants can reduce their loneliness, helplessness, and hopelessness, which are typical symptoms of depression. These previously named elements may contribute to the support group’s benefit in reducing participants’ depressive mood.
In this study, the Chinese GDS was used to assess the depressive symptoms of participants; a cut-off point ≥8 was indicative of clinical depression for Chinese participants.29 In fact, this cut-off point (GDS ≥8) has been widely used in local large-scale prevalence studies of depression among older people in Hong Kong.38,39 However, different cut-off points for the Chinese GDS have been suggested in the literature, including GDS ≥4,40 GDS ≥5,41 GDS ≥8,38,39 and GDS ≥10.33 Most of these studies included a sample without a diagnosis of dementia. Only one study33 has been performed to validate the use of the GDS for screening depression among Chinese persons with dementia living in Singapore. A cut-off point of a GDS score ≥10 has been suggested,33 which is close to the cut-off point adopted in the present study. Interestingly, a higher GDS cut-off point has also been suggested for Chinese persons with moderate to severe dementia.33 Thus, more research studies are needed to establish an optimal cut-off point for the Chinese GDS for a Chinese person with mild dementia. Nevertheless, the research results of this present study (ie, the significant reduction of the GDS score among support group participants) remain unchanged, even when adopting a different cut-off point for the Chinese GDS.
Conclusion
In a recent review on various nonpharmacological interventions for persons with mild dementia, support groups have been recommended as an effective intervention by experts.4 This present randomized controlled study provides evidence to support the efficacy and effectiveness of the structured and time-limited support group for Chinese persons with mild dementia. In particular, the present study shows that support groups can reduce depressive symptoms among participants.
Several methodological limitations of this randomized control study require attention. First, the generalizability of the research results are limited by the small sample size. In the future, it would be better to conduct a larger scale randomized controlled study to further validate the effectiveness and benefits of the support group model for Chinese persons with mild dementia. Second, promoting an acceptance of illness, handling role adjustment, developing a positive lifestyle, letting go of responsibilities without feeling guilty, improving relationship with family caregivers, and facilitating emotional support among participants are thought to be essential elements of this support group. However, no standardized tools have been adopted to assess these elements in this study. So, it is better to conduct further research studies to identify the essential elements of a support group for Chinese persons with mild dementia.
Acknowledgment
This study was generously sponsored by the Social Science Faculty of Hong Kong Baptist University.
Disclosure
The authors report no conflicts of interest in this work.
References
Lam LC, Tam CW, Lui VW, et al. Prevalence of very mild and mild dementia in community-dwelling older Chinese people in Hong Kong. Int Psychogeriatr. 2008;20(1):135–148. | ||
The Hong Kong Council of Social Service. Elderly Service in Hong Kong. Hong Kong: The Hong Kong Council of Social Service; 2007. | ||
Hogan DB, Bailey P, Black S, et al. Diagnosis and treatment of dementia: 5. Nonpharmacologic and pharmacologic therapy for mild to moderate dementia. CMAJ. 2008;179(10):1019–1026. | ||
Burgener S, Beattie E, Bossen A, Buckwalter K, Buettner L, Fick D, et al. Consensus Report: Review of Scientific Evidence Addressing Prevalence, Documented Needs, and Interdisciplinary Research: Persons in Mild Alzheimer’s Dementia. Chicago, IL: Alzheimer’s Association; 2007. | ||
Li Y, Meyer JS, Thornby J. Depressive symptoms among cognitively normal versus cognitively impaired elderly subjects. Int J Geriatr Psychiatry. 2001;16(5):455–461. | ||
Fritze F, Ehrt U, Sønnesyn H, et al. Depression in mild dementia: associations with diagnosis, APOE genotype and clinical features. Int J Geriatr Psychiatry. 2011;26(10):1054–1061. | ||
Hurt C, Bhattacharyya S, Burns A, et al. Patient and caregiver perspectives of quality of life in dementia. An investigation of the relationship to behavioural and psychological symptoms in dementia. Dement Geriatr Cogn Disord. 2008;26(2):138–146. | ||
Starkstein SE, Jorge R, Mizrahi R, Robinson RG. The construct of minor and major depression in Alzheimer’s disease. Am J Psychiatry. 2005;162(11):2086–2093. | ||
Dorenlot P, Harboun M, Bige V, Henrard JC, Ankri J. Major depression as a risk factor for early institutionalization of dementia patients living in the community. Int J Geriatr Psychiatry. 2005;20(5):471–478. | ||
Rosness TA, Ulstein I, Engedal K. Stress affects carers before patient’s first visit to a memory clinic. Int J Geriatr Psychiatry. 2009;24(10):1143–1150. | ||
Bergdahl E, Allard P, Gustafson Y. Depression among the very old with dementia. Int Psychogeriatr. 2011;23(5):756–763. | ||
Lee HB, Lyketsos CG. Depression in Alzheimer’s disease: heterogeneity and related issues. Biol Psychiatry. 2003;54(3):353–362. | ||
Phinney A. Toward understanding subjective experiences of dementia. In: Downs M, Bowers B, editors. Excellence in Dementia Care: Research Into Practice., Berkshire, UK: McGraw-Hill Education, Open University Press; 2008:35–51. | ||
Waite A, Bebbington P, Skelton-Robinson M, Orrell M. Life events, depression and social support in dementia. Br J Clin Psychol. 2004;43(Pt 3):313–324. | ||
Lyketsos CG, Lee HB. Diagnosis and treatment of depression in Alzheimer’s disease. A practical update for the clinician. Dement Geriatr Cogn Disord. 2004;17(1–2):55–64. | ||
Rosness TA, Barca ML, Engedal K. Occurrence of depression and its correlates in early onset dementia patients. Int J Geriatr Psychiatry. 2010;25(7):704–711. | ||
Logsdon RG, Pike KC, McCurry SM, et al. Early stage memory loss support groups: outcomes from a randomized controlled clinical trial. J Gerontol B Psychol Sci Soc Sci. 2010;65(6):691–697. | ||
Yale R. Developing Support Groups for Individuals with Early-Stage Alzheimer’s Disease: Planning, Implementation, and Evaluation. Baltimore, MD: Health Professions Press; 1995. | ||
Snyder L, Bower D, Arneson S, Shepherd S, Quayhagen M. Coping with Alzheimer’s Disease and Related Disorders: An Educational Support Group for Mild Individuals and Their Families. San Diego, CA: UCSD Alzheimer’s Disease Research Center; 1994. | ||
Gaugler JE, Gallagher-Winker K, Kehrberg K, et al. The Memory Club: Providing support to persons with early-stage dementia and their care partners. Am J Alzheimers Dis Other Demen. 2011;26(3):218–226. | ||
Zarit SH, Femia EE, Watson J, Rice-Oeschger L, Kakos B. Memory Club: a group intervention for people with early-stage dementia and their care partners. Gerontologist. 2004;44(2):262–269. | ||
Morrissey MV. Rethinking the benefits of an adapted version of ‘Alzheimer Café’ for individuals with Alzheimer’s and their partners. Int J Psychiatr Nurs Res. 2006;12(1):1393–1401. | ||
Goldsilver PM, Gruneir MR. Early stage dementia group: an innovative model of support for individuals in the early stages of dementia. Am J Alzheimers Dis Other Demen. 2001;16(2):109–114. | ||
Snyder L, Jenkins C, Joosten L. Effectiveness of support groups for people with mild to moderate Alzheimer’s disease: an evaluative survey. Am J Alzheimers Dis Other Demen. 2007;22(1):14–19. | ||
Mok E, Lai CK, Wong FL, Wan P. Living with early-stage dementia: the perspective of older Chinese people. J Adv Nurs. 2007;59(6):591–600. | ||
Lam CS, Tsang HWH, Corrigan PW, et al. Chinese lay theory and mental illness stigma: implications for research and practices. J Rehabil. 2010;76(1):35–40. | ||
Chan A, Kwok I. Hong Kong List Learning Test (HKLLT): Manual and Preliminary Norms. Hong Kong: Chinese University of Hong Kong; 1999. | ||
Chiu HF, Lee HC, Chung WS, Kwong PK. Reliability and validity of the Cantonese version of mini-mental state examination – a preliminary study. Journal of Hong Kong College of Psychiatry. 1994;4(2):25–28. | ||
Chiu HF, Lee HC, Wing YK, Kwong PK, Leung CM, Chung DW. Reliability, validity and structure of the Chinese Geriatric Depression Scale in a Hong Kong context: a preliminary report. Singapore Med J. 1994;35(5):477–480. | ||
Sheehan B. Assessment scales in dementia. Ther Adv Neurol Disord. 2012;5(6):349–358. | ||
Lach HW, Chang YP, Edwards D. Can older adults with dementia accurately report depression using brief forms? Reliability and validity of the Geriatric Depression Scale. J Gerontol Nurs. 2010;36(5):30–37. | ||
Lucas-Carrasco R. Spanish version of the Geriatric Depression Scale: reliability and validity in persons with mild-moderate dementia. Int Psychogeriatr. 2012;24(8):1284–1290. | ||
Lam CK, Lim PP, Low BL, Ng LL, Chiam PC, Sahadevan S. Depression in dementia: a comparative and validation study of four brief scales in the elderly Chinese. Int J Geriatr Psychiatry. 2004;19(5):422–428. | ||
Sheikh JI, Yesavage JA. 1986. Geriatric Depression Scale (GDS): Recent evidence and development of a shorter version. Clin Gerontol. 1986;5(1–2):165–173. | ||
Leung SO, Wong PM. Validity and reliability of Chinese Rosenberg Self-Esteem Scale. New Horizons in Education. 2008;56(1):62–69. | ||
Schwarzer R, Bäβler J, Kwiatek P, Schröder K, Zhang JX. The assessment of optimistic self-beliefs: comparison of the German, Spanish, and Chinese versions of the General Self-Efficacy Scale. Applied Psychology: An International Review. 1997;46(1):69–88. | ||
Keady J, Nolan M. IMMEL: assessing coping responses in the early stage of dementia. Br J Nurs. 1995;4(6):309–314. | ||
Woo J, Ho SC, Lau J, et al. The prevalence of depressive symptoms and predisposing factors in an elderly Chinese population. Acta Psychiatr Scand. 1994;89(1):8–13. | ||
Chi I, Yip PS, Chiu HF, et al. Prevalence of depression and its correlates in Hong Kong’s Chinese older adults. Am J Geriatr Psychiatry. 2005;13(5):409–416. | ||
Lim PP, Ng LL, Chiam PC, Ong PS, Ngui FT, Sahadevan S. Validation and comparison of three brief depression scales in an elderly Chinese population. Int J Geriatr Psychiatry. 2000;15(9):824–830. | ||
Lai DW, Fung TS, Yuen CT. The factor structure of a Chinese version of the Geriatric Depression Scale. Int J Psychiatry Med. 2005;35(2):137–148. |
 © 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.