Back to Journals » Diabetes, Metabolic Syndrome and Obesity » Volume 16
A Scoping Review of Trials Designed to Achieve Remission of Type 2 Diabetes with Lifestyle Intervention Alone: Implications for Sub-Saharan Africa
Authors Duhuze Karera MG, Wentzel A, Ishimwe MCS, Gatete JDD , Jagannathan R , Horlyck-Romanovsky MF, Sumner AE
Received 4 January 2023
Accepted for publication 20 February 2023
Published 9 March 2023 Volume 2023:16 Pages 677—692
DOI https://doi.org/10.2147/DMSO.S403054
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Prof. Dr. Juei-Tang Cheng
M Grace Duhuze Karera,1,2 Annemarie Wentzel,3,4 MC Sage Ishimwe,2 Jean de Dieu Gatete,1 Ram Jagannathan,5 Margrethe F Horlyck-Romanovsky,1,6 Anne E Sumner1,7
1Section on Ethnicity and Health, Diabetes, Endocrinology, and Obesity Branch, National Institute of Diabetes, Digestive and Kidney Diseases, National Institutes of Health, Bethesda, MD, USA; 2Institute of Global Health Equity Research, University of Global Health Equity, Kigali, Rwanda; 3Hypertension in Africa Research Team, North-West University, Potchefstroom, South Africa; 4South African Medical Research Council, Unit for Hypertension and Cardiovascular Disease, North-West University, Potchefstroom, South Africa; 5Department of Medicine, Emory University School of Medicine, Atlanta, GA, USA; 6Department of Health and Nutrition Sciences, Brooklyn College, City University of New York, New York, NY, USA; 7National Institute of Minority Health and Health Disparities, NIH, Bethesda, MD, USA
Correspondence: Anne E Sumner, Building 10, CRC-Rm 6940, Bethesda, MD, 20892-1612, USA, Tel +1 301-402-4240, Email [email protected]
Abstract: According to the International Diabetes Federation, sub-Saharan Africa is experiencing the highest anticipate increase in the prevalence of type 2 diabetes (T2D) in the world and has the highest percent of people living with T2D who are undiagnosed. Therefore, diagnosis and treatment need prioritization. However, pharmacological hypoglycemics are often unavailable and bariatric surgery is not an option. Therefore, the ability to induce T2D remission through lifestyle intervention alone (LSI-alone) needs assessment. This scoping review evaluated trials designed to induce T2D remission by LSI-alone. PubMed, Embase, Cochrane, and CINAHL databases were searched for trials designed to induce T2D remission through LSI-alone. Of the 928 identified, 63 duplicates were removed. With abstract review, 727 irrelevant articles were excluded. After full-text review, 112 inappropriate articles were removed. The remaining 26 articles described 16 trials. These trials were published between 1984 and 2021 and were conducted in 10 countries, none of which were in Africa. Remission rates varied across trials. Predictors of remission were 10% weight loss and higher BMI, lower A1C and shorter T2D duration at enrollment. However, LSI-alone regimens for newly diagnosed and established T2D were very different. In newly diagnosed T2D, LSI-alone were relatively low-cost and focused on exercise and dietary counseling with or without calorie restriction (~1500 kcal/d). Presumably due to differences in cost, LSI-alone trials in newly diagnosed T2D had higher enrollments and longer duration. For established T2D trials, the focus was on arduous phased dietary interventions; phase 1: low-calorie meal replacement (< 1000 kcal/day); phase 2: food re-introduction; phase 3: weight maintenance. In short, LSI-alone can induce remission in both newly diagnosed and established T2D. To demonstrate efficacy in Africa, initial trials could focus on newly diagnosed T2D. Insight gained could provide proof of concept and a foundation in Africa on which successful studies of LSI-alone in established T2D could be built.
Keywords: hypoglycemics, low-income countries, bariatric surgery, non-communicable diseases
Plain Language Summary
Lifestyle intervention (LSI) studies have expanded from prevention to remission of type 2 diabetes (T2D). While studies have shown that T2D detected early, can go into remission if treated with LSI-alone, no studies on LSI-alone have been conducted in sub-Saharan Africa. T2D prevalence is rising in sub-Saharan Africa, but medication access is limited, and bariatric surgery is not feasible. In short, T2D screening could be prioritized in sub-Saharan Africa if LSI-alone could promote remission. Furthermore, as T2D is a non-communicable disease with increased vulnerability to infectious diseases such as COVID-19 and tuberculosis, data on the ability of LSI-alone to induce T2D remission, could convince sub-Saharan African governments to invest in T2D screening. This review was conducted to demonstrate the depth and breadth of studies already conducted on T2D remission by LSI-alone. Sixteen studies were identified. Seven studies focused on newly diagnosed T2D. Nine studies were conducted in established T2D. The trials in newly diagnosed T2D required moderate calorie restriction (1200–1800 kcal/d), counseling and exercise. In established T2D, total diet replacement with low calorie liquid supplements (300–1000 kcal/d) were required. In short, LSI regimens for remission of newly diagnosed T2D are less rigorous and easier to institute than for established T2D. The initial focus in African countries could be on designing and testing protocols to achieve remission by LSI-alone in newly diagnosed T2D. Successful LSI-alone trials in newly diagnosed T2D could provide an African foundation on which successful studies of LSI-alone in established T2D could be built.
Introduction
A new frontier in Lifestyle Invention (LSI) research is emerging. LSI with its focuses on diet and exercise, is an established way to prevent or delay the onset of type 2 diabetes (T2D).1–4 The new question is: does LSI have a role in achieving T2D remission.5–7
For sub-Saharan Africa, the value in determining whether LSI can achieve T2D remission is potentially enormous. By 2045 year, the number of Africans living with T2D will increase from 24 million to 55 million.8 This represents an 129% increase in prevalence and is the highest anticipated increase in the world.8 Furthermore, 54% of individuals currently living with T2D in Africa are undiagnosed.8 In fact, Africa has the highest percent in the world of people living with T2D who are undiagnosed.8 If LSI-alone were effective treatment and could even induce T2D remission, there would be incentive for African governments to invest scarce health care resources in screening for T2D.
T2D remission trials using LSI can be divided into two categories. The most well-known category combines LSI with either hypoglycemic medication or bariatric surgery.9,10 The other category, which is less studied, but would have greater public health impact in Africa are studies of T2D remission using LSI-alone.
In many African countries, medications account for 70% of the direct cost of T2D and most often are paid for by the individual patient.11,12 Even when symptomatic, medication cost is a major disincentive to seeking care.13 Consequently, diagnosis of T2D is often delayed, setting the stage for the onset of irreversible complications and even higher costs.12,14 Furthermore, untreated, undiagnosed T2D increases susceptibility to many infectious diseases including tuberculosis and COVID-19.8,15
To develop policy about the use of LSI-alone as a therapeutic modality for T2D remission, a consensus based on numerous, high-quality studies is required.7 However, studies on whether LSI-alone will induce remission of T2D are few.
As the literature is scant and no guidelines currently exist on the use of LSI-alone to induce T2D remission, we undertook a scoping review.16
This scoping review evaluates the ability of LSI-alone to induce remission in T2D. Due to the twin challenges of rising prevalence of T2D and relative lack of data in Africa, findings are analyzed throughout this review relative to their applicability to Africa. Due to the high prevalence of undiagnosed T2D in African countries,8 a key question in the public health arena is whether newly diagnosed can be effectively treated with LSI-alone. Searches of previous reviews and meta-analyses of LSI designed to reverse T2D revealed that LSI trials were not divided into two groups: newly diagnosed, treatment-naive T2D and established T2D.6,7,17 As both enrollment criteria and the actual elements of LSI interventions may differ depending on whether T2D is newly diagnosed or established, trials in this scoping review were divided into two groups: newly diagnosed or established T2D.
Search Strategy
English language publications were searched in: PubMed (National Library of Medicine), Embase (Elsevier), the Cochrane Library (Wiley) and the Cumulative Index to Nursing and Allied Health Literature (EBSCOhost). All articles published or in press through September 16, 2021, were evaluated. The search used a combination of controlled vocabulary terms and key words specific to each database (ie, MeSH and EMTREE) (Supplement). Title/abstract, full text review, and data extraction were conducted using Covidence (Covidence.org, Melbourne, Australia), an online application which ensures a rigorous protocol and blinded review.
Inclusion criteria were: studies in adults which were controlled or observational or prospective trials, cohort studies or case–control studies. Exclusion criteria were: investigations with a bariatric surgery or pharmaceutical therapy arm, studies of either type 1 diabetes or gestational diabetes. Reviews, commentaries, position papers and guidelines were also excluded.
Article Identification and Data Extraction
The review yielded 928 publications with 63 duplicate articles removed (Figure 1). Of the 865 remaining articles, title and abstract screening led to exclusion of 727 irrelevant articles. Full text review of the remaining 138 articles led to the removal of 112 articles because they did not meet inclusion criteria. The remaining 26 articles described 16 trials. To ensure each trial would be represented by only one article, 10 articles were excluded as redundant and only the latest trial-specific publication which specifically focused on remission rate were included. Of the 16 trials, 7 trials were in newly diagnosed, treatment-naive T2D and 9 trials were in established T2D with LSI initiated after discontinuation of medications.
 |
Figure 1 Flowchart on trial inclusion. *Multiple publications from the same study. |
During the article identification phase, title/abstract and full text reviews were judged independently by two of the authors (MGDK and AES). Disagreements were resolved by a third author (MFHR). Data extraction was performed independently by two authors (MGDK and AES), compared and entered into Table 1 and Table 2.
 |
Table 1 Studies Designed to Induce Remission in Newly Diagnosed Treatment Naïve Diabetes (Ordered by Least to Most Restrictive Diet) |
 |
Table 2 Studies Designed to Induce Remission in Previously Diagnosed Diabetes After Medications Discontinued (Ordered by Year of Publication) |
Assessment of LSI Design and Success
Data from the 16 trials were divided into two tables. Table 1 includes studies in newly diagnosed T2D and Table 2 established T2D. Table 1 was subsequently divided into two sections.18–24 Section 1A lists the 4 trials with newly diagnosed T2D and no caloric restriction. Section 1B lists the 3 trials with newly diagnosed T2D and mild caloric restriction.
Table 2 includes the 9 trials identified in established T2D in which hypoglycemic medications were discontinued at the time LSI was initiated.25–33 As the design of newer trials was consistently based on the outcome of earlier trials, the studies in Table 2 are presented in chronological order, oldest to newest.
Remission Rates
To evaluate remission rates across studies, three issues needed consideration.
First, some studies reported the remission rate as one number, specifically the sum of those in the trial who converted from T2D to either prediabetes or normal glucose tolerance (NGT). Other studies reported two remission rates, one for T2D to prediabetes and one for T2D to NGT. In accordance with current guidelines, we report remission as a single number, meaning the transition from T2D to either prediabetes or NGT.7,34,35
Second, remission criteria were not uniform across studies. Some investigations used the OGTT, others used fasting plasma glucose (FPG) or glycated hemoglobin A1C (A1C) and still others used a combination of A1C and FPG. An additional challenge is that these trials were conducted from 1984 to 2021. Over this time span, ADA criteria for T2D diagnosis changed. From 1979 to 1998, T2D diagnosis required FPG≥140 mg/dL and/or 2h glucose ≥200 mg/dL.36 In 1999 the FPG threshold was lowered to ≥126 mg/dL. Furthermore, it is only since 2010 that A1C has been used as a diagnostic criterion for T2D.37 Eight of the 13 studies published since 2010 incorporated A1C into their remission criteria. Table 1 and Table 2 report remission rates by trial-specific criteria.
Third, study duration varied. The shortest trial was 5 weeks and the longest 8 years. Some studies provided both interim and end of study remission rates. For consistency, only end of study remission rates are reported.
Control Groups
Some, but not all trials, had control groups which did not receive LSI. Most trials compared the metabolic and social characteristics of remitters to non-remitters. Additionally, two studies did not provide either remission rates or control groups. Instead, they described in the intervention group how LSI influenced the physiologic control of glycemia.28,30
Results
Participant Characteristics: Country, Race/Ethnicity and Gender
The trials were published over a nearly 40-year period, between 1984 and 2021 and conducted in 10 countries. Eight (8/16) or 50% of the trials were conducted in Europe. Four of the trials, 25% (4/16) were conducted in the Americas, specifically two in the United States and two in Barbados. Four trials or 25% (4/16) were conducted in Asia (Japan and India), the Middle East (Qatar), and Oceania (Australia).
No trials were conducted in an African country. In fact, enrolment of people of African descent was described only in the two studies conducted in Barbados (24, 27). These studies were small with 10 and 25 participants, respectively. The two studies conducted in the United States did not provide race/ethnicity data and were also small with 10 participants in one study and 12 in the other (25, 36).
With the exception of the Malmo Feasibility Study which only enrolled men,20 the other studies enrolled nearly equal numbers of men and women.
Median enrolment in newly diagnosed T2D trials was 180 (range: 10 to 867). Median number of participants in the established T2D trials was 20 (range: 10 to 149) (Figure 2).
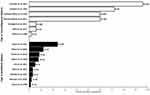 |
Figure 2 Duration and participant number in LSI-alone remission trials. White bars: trials in newly-diagnosed trials; black bars: trials in established T2D. |
Median duration of the newly diagnosed T2D trials was 5 years (range: 7 weeks to 8 years). Median duration of the established T2D trials was 5 months (range: 5 weeks to 2 years) (Figure 2).
Enrolment Criteria
In the four trials of LSI-alone in newly diagnosed T2D without calorie restriction, the only enrolment criteria specified was newly diagnosed, treatment-naive T2D. In the three trials of newly diagnosed T2D with moderate caloric restriction, participants had to have an overweight (BMI≥25) or obese BMI (BMI≥30) with one study capping BMI <40 kg/m2.22,27,38 One trial capped A1C at enrolment to ≤8% and the other at ≤ 11%.21,38
In the 9 trials with established T2D, markedly uncontrolled T2D was an exclusion criterion. For example, most studies specified that A1C had to be ≤12%.26,28,29,31–33 Prior insulin therapy was an exclusion criterion in 4 trials.26–28,33 Six studies capped T2D duration prior to enrolment to: <3, <4, <6 or <8 years.26,28–30,32,33 Most trials required an absence of end-organ damage, specifically nephropathy, heart failure and liver dysfunction.26,28,30–33
LSI-alone trials in established T2D, specified a baseline BMI of ≥25, ≥27 or ≥30 kg/m2. Four studies capped BMI at enrolment at ≤45 kg/m2.28,30,31,33
LSI-Alone Trials in Newly-Diagnosed T2D
There were 4 studies which enrolled people with newly diagnosed T2D and had no caloric restrictions (Table 1A). The earliest trial was conducted in Australia and published in 1984.23 The study enrolled 10 Aboriginal persons with T2D who were living in urban areas and willing to move for 7 weeks to a rural area and live as hunter-gatherers.23 Weight loss was ~8 kg or ~10% of baseline weight and remission was 70%. The other 3 trials had a duration of 5 to 6 years and were conducted in European countries (United Kingdom, Sweden and Spain).19,20,24 Counselling sessions were several times a year (Table 1A). Exercise was not specified but encouraged. Remission rate was 30% to 54%. Weight loss in two studies ranged from ~3% to 7% of baseline weight. In the third trial which was 5 years in duration, weight did not decline. Participants in that trial were randomized to either a Mediterranean or a low-fat diet. The 40% remission rate on both diets was attributed to the change in nutrient composition from usual diets.24
There were 3 trials with caloric restrictions in newly diagnosed T2D (Table 1B). Caloric restrictions were moderate and either 500 kcal/d less than recommended for weight maintenance or 1500 to 1800 kcal/d for men and 1200 to 1500 kcal/d for women. The counselling sessions were weekly or monthly (Table 1B). Exercise was prescribed for ~25 minutes/day.
For the 2 studies which were 6 months in duration, the T2D remission rates were 50% and 80%.22,38 For the third study, which was 8 years in duration, the end of study remission rate was 0%.21 This study was designed to compare T2D remission rates with a low-carbohydrate Mediterranean diet to a low-fat diet. At 6 years, no individuals on the low-fat diet were in remission. For the low-carbohydrate Mediterranean diet it was 8 years before all participants developed T2D. Absolute weight loss was not reported. The investigators hypothesized that the 8-year delay in T2D progression in the low-carbohydrate Mediterranean diet group versus the 6-year delay in the low-fat diet group were due to differences in diet composition.
LSI-Alone Trials in Established T2D
There were 9 LSI-alone trials in established T2D (Table 2). After hypoglycemic medication was discontinued, diet and counselling were the focus of the LSI for established T2D. All 9 trials had at the outset a total diet replacement phase provided as soups and shakes or commercially prepared liquid meals such as Cambridge Diet, Optifast, and Glucerna. These Phase 1 diets were prescribed for periods of 5 weeks to 4 months with a median duration of 2 months. The earliest LSI-alone trial in established T2D was conducted in the United States in 1986 as an inpatient study.27 It provided the lowest daily allotment of 300 kcal/d. The other 8 studies did not include hospitalizations and had calorie allotments of 450 to 1000 kcal/d. In these trials, the interaction with the research team was daily to weekly (Table 2). Five of the studies had a gradual food re-introduction phase which lasted between 2 weeks and 3 months.26,28,31–33 During this phase, contact with the research team was weekly to monthly. In 4 of the 9 trials, there was a Phase 3 with a duration of 5 to 18 months.26,31–33 To sustain weight loss, Phase 3 diets were designed to be isocaloric. Interaction with the study team during Phase 3 was generally monthly.
With one exception, physical activity was not a focus of LSI-alone trials in established T2D. In 8 of the 9 the LSI trials, maintenance of baseline activity or a moderate increase without specific instructions were recommended. However, in the trial conducted in Qatar, participants were instructed during the first two dietary phases to undertake 10,000 steps/d.32 During the weight maintenance phase, 20 minutes/d of unsupervised activity was prescribed.
Remission Rates
Fourteen of 16 studies provided end of trial remission rates (Table 1 and Table 2). Remission rates for these 14 trials combined, ranged from 0 to 100%, and were dependent on study duration. For example, the study with a duration of 5 weeks had a 100% remission rate,27 whereas the study with a duration of 8 years, had at 8 years, a 0% rate of remission.21
Metabolic Effects of LSI-Alone
The metabolic effects of LSI were described in 4 newly diagnosed T2D trials (Table 1) and 8 established T2D trials (Table 2). Parameters included and investigative tool intensity varied across studies. Some trials made metabolic assessments based on FPG and plasma insulin concentrations only and others used insulin clamps and scans. Nonetheless, the major theme across studies was that LSI-alone leads to a decrease in insulin resistance and an increase in beta-cell responsiveness. Additionally decreases in hepatic and pancreatic fat and a decline in visceral adipose tissue were observed.
Predictors of T2D Remission According to Baseline Characteristics
One newly diagnosed T2D trial and 4 established T2D trials reported on baseline factors associated with remission. Across these five studies, baseline predictors of successful remission were: shorter duration of T2D, fewer oral hypoglycemic medications at enrolment, lower baseline values of A1C and FPG, less insulin resistance and preserved beta-cell function. In addition, higher BMI and WC at baseline were associated with greater remission rates in two studies but were not a factor in a third study.25,26,33 However, these differences may be accounted for by differences in race/ethnicity. One study enrolled Asian Indians,25 another study enrolled Black Caribbeans26 and the third, Whites from the United Kingdom.33 In addition, sample size may have been a factor. The two trials which showed that a high BMI or WC at baseline were important in predicting remission had ≤25 participants, whereas the study which did not have this finding, had 149 participants.25,26,33
The relationship of age to remission rate was inconsistent. Two studies reported that younger age at enrolment predicted remission and whereas, a third study reported that older age did.25,31,33
Nonglycemic Effects of LSI-Alone
Blood pressure, renal function, physical fitness, and quality of life improved with LSI-alone in all studies which evaluated these parameters (Table 1 and Table 2).
Lipid profiles were evaluated in 4 of the newly diagnosed T2D trials. Triglyceride (TG) levels declined in 3 studies and did not change in one. In the study by Esposito et al, HDL increased on the Mediterranean diet, but decreased on the low-fat diet.21 In the study by Ades et al the cholesterol and HDL concentrations did not change but the cholesterol/HDL ratio decreased.38 In the investigation of Aboriginal people living as hunter gatherers, HDL levels declined.23
Lipid profiles were examined in 7 of the established T2D trials. As 5 of 7 studies showed a decline in TG levels and 2 of 7 showed no change, the effect on TG can be interpreted as either positive or neutral. For HDL, one study showed a decline, the other 6 studies reported no change or an increase. For total cholesterol, 2 studies reported no change and 1 study reported an increase. Two studies reported on LDL levels with one investigation reporting no change and the other an increase.
Discussion
This scoping review revealed that over nearly 40 years, 16 LSI-alone trials for diabetes remission were conducted in 10 countries. None of the trials were conducted in Africa. Overall, in LSI-alone remission trials, enrolment was generally restricted to individuals with A1C<11% and BMI ≤45 kg/m2. In established T2D, enrolment criteria also usually included: T2D duration of <6 years, no previous insulin therapy, and no end-organ damage. Whether these enrolment criteria are necessary to achieve success with LSI-alone remains to be established. However, remission rates must be considered relative to study duration. For example, the shortest trial was an established T2D study conducted for a 5-week period. The remission rate at 5 weeks was 100%.27 The longest trial enrolled individuals with newly diagnosed T2D. By 8 years, all 215 participants required hypoglycemics. Hence, the remission rate was and 0%.21
As LSI delays but does not prevent the recurrence of T2D,21 weight regain, the most prominent factor triggering relapse of T2D, must be minimized.39 Recognizing the relapse risk associated with weight gain, the DiRECT trial investigators designed partial and full meal replacement regimens if weight gain was 2kg or 4kg, respectively.39
Due to the risk of relapse, surveillance is essential. In short, if LSI is instituted as remission therapy of T2D, follow-up at 6 months intervals is necessary.7 However, if LSI-alone decreases glucose levels below diabetic thresholds for a substantial period of time, then better health and decreased costs could result.27
Benefits of Remission
The benefits of medication-free LSI can be divided into two categories, one: immediate and measurable and two: long-term and speculative. Immediate and measurable benefits include improved blood pressure, enhanced quality of life and better physical fitness (Table 1 and Table 2). The metabolic benefits include a decrease in hepatic and whole-body insulin resistance, less visceral adiposity, and improved β-cell responsiveness. In addition, in most studies, TG levels decreased, and HDL levels increased.
As a long-term benefit, if LSI alone achieves remission, medications do not need to be purchased during that time. As stated earlier, 70% of the direct cost of T2D diabetes in African countries are borne by patients.11,12 Whereas the cost of LSI counselling in newly diagnosed T2D are essentially the same as usual care and presumably less expensive than the cost that would be incurred with medication administration.19,21 In short, dietary and physical activity counselling are probably cost-effective and should be part of all T2D management programs. For example, the ADDITION-Cambridge Trial had a remission rate of 30% at 5 years with only one annual 30-minute review supplemented by three additional 10-minute sessions.19 The ADDITION-Cambridge Trial did not specify a physical activity program.
The major speculative benefit of LSI is the prevention of diabetic complications during the remission period. To the extent to which diabetes complications are caused by hyperglycemia, decreasing glycemia for an extended period of time should prevent or minimize these.21 For example, Harayama et al found in a 6-month trial of LSI in 180 Japanese individuals with obesity and newly diagnosed T2D that hyperglycemia decreased, glomerular filtration rate increased and proteinuria declined.22 Weight loss as the Pathway to Remission Weight loss at ~10% of baseline weight or ~10 kg overall appears to have been essential to achieving T2D remission in 5 of the newly diagnosed T2D trials and all 9 established T2D trials. However, for 2 newly diagnosed T2D trials, remission was triggered by diet modification without weight loss.21,24 The presumption that weight loss would be the trigger for T2D remission was the foundation on which the LSI trials were built.28,31,33 As an enrolment criterion, BMI in either the overweight or obese category was required in 3 of the newly diagnosed T2D trials and 8 of the established T2D trials. Furthermore, higher BMI and WC at baseline were predictors of remission through weight loss.25 In short, for weight loss to improve glycemia, excess weight had to be a baseline characteristic.
Weight loss as the key to T2D remission is embedded in the twin-cycle hypothesis.40 The twin cycle hypothesis was built by Roy Taylor and colleagues based on observations from three successively larger and longer trials of LSI-alone in established T2D, specifically Counterpoint (n = 11; duration = 5 months), Counterbalance (n = 30, duration = 9 months) and DiRECT (n = 149; duration = 24 months) (Table 2).28,31,33 The twin-cycle hypothesis has four components: (1) all persons with T2D have crossed a personal fat threshold and are in positive calorie balance and need to lose weight, (2) both the liver and pancreas are dysfunctional due to TG overload, (3) TG overload leads to the liver developing insulin resistance and the pancreas secreting less insulin than necessary to achieve euglycemia, (4) weight loss will reverse the TG overload in the pancreas, improve pancreatic insulin secretory capacity, reverse hepatic insulin resistance and remission will occur.40
Despite widespread acceptance of the twin-cycle hypothesis, two studies in this review found remission of newly diagnosed T2D occurred because of dietary modification rather than weight loss.21,24 Therefore, the universal applicability of the twin-cycle hypothesis needs to be reconsidered, particularly in Africa and low and middle income countries generally, where the prevalence of T2D is increasing in normal weight individuals.41
Applicability of Existing LSI Trials to T2D Remission in African Countries
There are at least two reasons why currently available LSI-alone regimens must be critically evaluated and possibly redesigned before widespread institution in African countries.
First, there is increasing awareness that the etiology of T2D in many Africans may be primarily β-cell failure rather than obesity-induced insulin resistance.41–45 There are genetic reasons for β-cell failure in Africans as well as the transgenerational effects of early life or inter-uterine undernutrition and epigenetic changes.42–44 In short, LSI programs based on insulin resistance as the major cause of T2D may be, less successful in Africans than in populations that have insulin resistance as the primary determinant of T2D. Therefore, LSI-alone regimens designed for Africa must assess the impact on T2D remission of dietary modification independent of weight loss.
Second, there is no data in established T2D on whether the low-calorie liquid diet used in Phase 1 of LSI-alone trials would be socially or culturally acceptable to Africans. This issue is independent of the cost and lack of availability in Africa of the liquid preparations used in the Phase 1 total dietary replacement period.
Altogether, designing LSI-alone intervention for the purpose of promoting T2D in African countries, might optimally begin with trials designed to specifically address newly diagnosed T2D rather than established T2D. LSI trials in newly diagnosed T2D may be easier to conduct and less expensive that LSI in established T2D. Scoping reviews preclude statistical comparisons between studies.16 Nonetheless we note that LSI-alone trials in newly diagnosed T2D appear to be longer in duration and have higher enrollments than the LSI established T2D (Figure 2). Cost and ease of trial administration may be factors.
Limitations and Strengths
This review is a valuable reference for investigators on the trials which are available on the ability of LSI-alone to promote T2D remission. By design, studies with either bariatric surgery or pharmaceutical arms were not included. Bariatric surgery is not a public health strategy and in many areas of the world medication for the treatment of T2D is not available.
Additionally, this review is the first to divide LSI trials into two groups: newly diagnosed T2D and established T2D. By doing this, it became clear that both enrollment criteria and the design of the LSI differed by T2D type. In addition, as a scoping review this study included trials with a relatively small number of participants (ie ≤25). In general, before large trials are funded, there must be smaller studies which demonstrate proof of concept and the existence of essential infrastructure. Table 1 and Table 2 were designed to direct prospective investigators to small previously successful studies which could be used as blueprints.
The main limitation of this review is that the trials designed to determine whether LSI-alone can induce T2D remission were few in number, variable in size, and conducted over nearly 40 years.
Conclusions
Due to the rise in prevalence of T2D across the African continent, investment in trials which determine the effectiveness and design of studies of LSI-alone deserve study. In short, trials of LSI-alone combined with governmental policies in every African country which promote reversal of the rapidly increasing obesogenic environment, could fundamentally slow the upward trajectory of T2D across the continent.8,46 However, this scoping review was unable to identify any publications which specifically addressed in a sub-Saharan African country whether LSI-alone can reverse T2D. However, this review did identify 16 trials which demonstrated that LSI-alone is a means by which T2D may be reversed for a period of months to years (Table 1 and Table 2) and could be used as models.
However, there are fundamental differences in the design of LSI necessary for newly diagnosed versus established T2D. Compared to LSI in established T2D, LSI for newly diagnosed T2D focuses on diet modification even without weight loss, requires less intensive follow-up, less resources and has a greater emphasis on exercise. Due to the emphasis on diet modification, LSI-alone for newly diagnosed T2D may be appropriate for Africa where a significant proportion of the population may have T2D predominantly from β-cell failure rather than obesity-related insulin resistance.47,48 In short, conduct of LSI-alone trials in Africa as a means to induce remission of newly diagnosed T2D deserves study. Insight gained from the conduct of LSI-alone trials in newly diagnosed T2D could provide proof of concept and an African foundation on which successful studies of LSI-alone in established T2D could be built.
Acknowledgments
We thank Nancy Terry, Biomedical Librarian of the National Institutes of Health Library, Bethesda, Maryland for her excellent support, insight and superb teaching.
GMDH and MCSI received support from the Institute of Global Health Equity Research of the University of Global Health Equity; GMDH, JdDG and AES received supported from the intramural program of the National Institute of Minority Health and Health Disparities; GMDH, JdDG and AES received support from the intramural program of the National Institute of Diabetes and Digestive and Kidney Diseases; AW was supported by the South African Medical Research Council, Unit for Hypertension and Cardiovascular Disease, North-West University, South Africa, RJ was supported by Department of Medicine, Emory University School of Medicine, Atlanta, GA MFH-R was supported by City University of New York, New York.
Disclosure
All authors declare no conflict of interest. All authors state that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Knowler WC, Barrett-Connor E, Fowler SE, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346(6):393–403. doi:10.1056/NEJMoa012512
2. Li G, Zhang P, Wang J, et al. Cardiovascular mortality, all-cause mortality, and diabetes incidence after lifestyle intervention for people with impaired glucose tolerance in the Da Qing Diabetes Prevention Study: a 23-year follow-up study. Lancet Diabetes Endocrinol. 2014;2(6):474–480. doi:10.1016/s2213-8587(14)70057-9
3. Lindstrom J, Ilanne-Parikka P, Peltonen M, et al. Sustained reduction in the incidence of type 2 diabetes by lifestyle intervention: follow-up of the Finnish Diabetes Prevention Study. Lancet. 2006;368(9548):1673–1679. doi:10.1016/s0140-6736(06)69701-8
4. Ramachandran A, Snehalatha C, Mary S, et al. The Indian Diabetes Prevention Programme shows that lifestyle modification and metformin prevent type 2 diabetes in Asian Indian subjects with impaired glucose tolerance (IDPP-1). Diabetologia. 2006;49(2):289–297. doi:10.1007/s00125-005-0097-z
5. Kelly J, Karlsen M, Steinke G. Type 2 Diabetes Remission and Lifestyle Medicine: a Position Statement From the American College of Lifestyle Medicine. Am J Lifestyle Med. 2020;14(4):406–419. doi:10.1177/1559827620930962
6. Rosenfeld RM, Kelly JH, Agarwal M, et al. Dietary Interventions to Treat Type 2 Diabetes in Adults with a Goal of Remission: an Expert Consensus Statement from the American College of Lifestyle Medicine. Am J Lifestyle Med. 2022;16(3):342–362. doi:10.1177/15598276221087624
7. MacKay D, Chan C, Dasgupta K. Remission of Type 2 Diabetes. Can J Diabetes. 2022;46(8):753–761. doi:10.1016/j.jcjd.2022.10.004
8. Aguirre F, Brown A. IDF Diabetes Atlas.
9. McTigue KM, Wellman R, Nauman E, et al. Comparing the 5-Year Diabetes Outcomes of Sleeve Gastrectomy and Gastric Bypass: the National Patient-Centered Clinical Research Network (PCORNet) Bariatric Study. JAMA Surg. 2020;155(5):e200087. doi:10.1001/jamasurg.2020.0087
10. Retnakaran R, Ye C, Emery A, Kramer CK, Zinman B. The metabolic effects of adding exenatide to basal insulin therapy when targeting remission in early type 2 diabetes in a randomized clinical trial. Nat Commun. 2022;13(1):6109. doi:10.1038/s41467-022-33867-9
11. Fadare J, Olamoyegun M, Gbadegesin BA. Medication adherence and direct treatment cost among diabetes patients attending a tertiary healthcare facility in Ogbomosho, Nigeria. Malawi Med J. 2015;27(2):65–70. doi:10.4314/mmj.v27i2.7
12. Quaye EA, Amporful EO, Akweongo P, Aikins MK. Analysis of the Financial Cost of Diabetes Mellitus in Four Cocoa Clinics of Ghana. Value Health Reg Issues. 2015;7:49–53. doi:10.1016/j.vhri.2015.08.005
13. Mapa-Tassou C, Katte JC, Mba Maadjhou C, Mbanya JC. Economic Impact of Diabetes in Africa. Curr Diab Rep. 2019;19(2):5. doi:10.1007/s11892-019-1124-7
14. Mutyambizi C, Pavlova M, Chola L, Hongoro C, Groot W. Cost of diabetes mellitus in Africa: a systematic review of existing literature. Global Health. 2018;14(1):3. doi:10.1186/s12992-017-0318-5
15. Al-Rifai RH, Pearson F, Critchley JA, Abu-Raddad LJ. Association between diabetes mellitus and active tuberculosis: a systematic review and meta-analysis. PLoS One. 2017;12(11):e0187967. doi:10.1371/journal.pone.0187967
16. Munn Z, Peters MDJ, Stern C, Tufanaru C, McArthur A, Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018;18(1):143. doi:10.1186/s12874-018-0611-x
17. Zhang Y, Yang Y, Huang Q, Zhang Q, Li M, Wu Y. The effectiveness of lifestyle interventions for diabetes remission on patients with type 2 diabetes mellitus: a systematic review and meta-analysis. Worldviews Evid Based Nursing. 2013;1:548. doi:10.1111/wvn.12608
18. Afulani PA, Torres JM, Sudhinaraset M, Asunka J. Transnational ties and the health of sub-Saharan African migrants: the moderating role of gender and family separation. Soc Sci Med. 2016;168:63–71. doi:10.1016/j.socscimed.2016.09.009
19. Dambha-Miller H, Day AJ, Strelitz J, Irving G, Griffin SJ. Behaviour change, weight loss and remission of Type 2 diabetes: a community-based prospective cohort study. Diabet Med. 2020;37(4):681–688. doi:10.1111/dme.14122
20. Eriksson KF, Lindgarde F. Prevention of type 2 (non-insulin-dependent) diabetes mellitus by diet and physical exercise. The 6-year Malmo feasibility study. Diabetologia. 1991;34(12):891–898. doi:10.1007/BF00400196
21. Esposito K, Maiorino MI, Petrizzo M, Bellastella G, Giugliano D. The effects of a Mediterranean diet on the need for diabetes drugs and remission of newly diagnosed type 2 diabetes: follow-up of a randomized trial. Diabetes Care. 2014;37(7):1824–1830. doi:10.2337/dc13-2899
22. Harayama TYT, Yoshioka K, Kogure A, et al. Correlation between weight loss and improvement of diabetes mellitus among obese type 2 diabetic patients. Diabetol Int. 2013;4:132–137. doi:10.1007/s13340-013-0107-1
23. O’Dea K. Marked improvement in carbohydrate and lipid metabolism in diabetic Australian aborigines after temporary reversion to traditional lifestyle. Diabetes. 1984;33(6):596–603. doi:10.2337/diab.33.6.596
24. Roncero-Ramos I, Gutierrez-Mariscal FM, Gomez-Delgado F, et al. Beta cell functionality and hepatic insulin resistance are major contributors to type 2 diabetes remission and starting pharmacological therapy: from CORDIOPREV randomized controlled trial. Transl Res. 2021;238:12–24. doi:10.1016/j.trsl.2021.07.001
25. Bhatt AA, Choudhari PK, Mahajan RR, et al. Effect of a Low-Calorie Diet on Restoration of Normoglycemia in Obese subjects with Type 2 Diabetes. Indian J Endocrinol Metab. 2017;21(5):776–780. doi:10.4103/ijem.IJEM_206_17
26. Bynoe K, Unwin N, Taylor C, et al. Inducing remission of Type 2 diabetes in the Caribbean: findings from a mixed methods feasibility study of a low-calorie liquid diet-based intervention in Barbados. Diabet Med. 2020;37(11):1816–1824. doi:10.1111/dme.14096
27. Henry RR, Wiest-Kent TA, Scheaffer L, Kolterman OG, Olefsky JM. Metabolic consequences of very-low-calorie diet therapy in obese non-insulin-dependent diabetic and nondiabetic subjects. Diabetes. 1986;35(2):155–164. doi:10.2337/diab.35.2.155
28. Lim EL, Hollingsworth KG, Aribisala BS, Chen MJ, Mathers JC, Taylor R. Reversal of type 2 diabetes: normalisation of beta cell function in association with decreased pancreas and liver triacylglycerol. Diabetologia. 2011;54(10):2506–2514. doi:10.1007/s00125-011-2204-7
29. Quimby KR, Sobers N, George C, Greaves N, Browman-Jones F, Samuels TA. Implementation of a community-based low-calorie dietary intervention for the induction of type-2 diabetes and pre-diabetes remission: a feasibility study utilising a type 2 hybrid design. Implement Sci Commun. 2021;2(1):95. doi:10.1186/s43058-021-00196-9
30. Romano L, Marchetti M, Gualtieri P, et al. Effects of a Personalized VLCKD on Body Composition and Resting Energy Expenditure in the Reversal of Diabetes to Prevent Complications. Nutrients. 2019;11(7):1526. doi:10.3390/nu11071526
31. Steven S, Hollingsworth KG, Al-Mrabeh A, et al. Very Low-Calorie Diet and 6 Months of Weight Stability in Type 2 Diabetes: pathophysiological Changes in Responders and Nonresponders. Diabetes Care. 2016;39(5):808–815. doi:10.2337/dc15-1942
32. Taheri S, Zaghloul H, Chagoury O, et al. Effect of intensive lifestyle intervention on bodyweight and glycaemia in early type 2 diabetes (DIADEM-I): an open-label, parallel-group, randomised controlled trial. Lancet Diabetes Endocrinol. 2020;8(6):477–489. doi:10.1016/s2213-8587(20)30117-0
33. Thom G, Messow CM, Leslie WS, et al. Predictors of type 2 diabetes remission in the Diabetes Remission Clinical Trial (DiRECT). Diabet Med. 2021;38(8):e14395. doi:10.1111/dme.14395
34. Buse JB, Caprio S, Cefalu WT, et al. How do we define cure of diabetes? Diabetes Care. 2009;32(11):2133–2135. doi:10.2337/dc09-9036
35. Riddle MC, Cefalu WT, Evans PH, et al. Consensus Report: definition and Interpretation of Remission in Type 2 Diabetes. Diabetes Care. 2021;44(10):2438–2444. doi:10.2337/dci21-0034
36. National Diabetes Data Group. Classification and diagnosis of diabetes mellitus and other categories of glucose intolerance. Diabetes. 1979;28(12):1039–1057. doi:10.2337/diab.28.12.1039
37. ADA. Summary of revisions for the 2010 Clinical Practice Recommendations. Diabetes Care. 2010;33:S3. doi:10.2337/dc10-S003
38. Ades PA, Savage PD, Marney AM, Harvey J, Evans KA. Remission of recently diagnosed type 2 diabetes mellitus with weight loss and exercise. J Cardiopulm Rehabil Prev. 2015;35(3):193–197. doi:10.1097/hcr.0000000000000106
39. Brosnahan N, Leslie W, McCombie L, et al. Brief formula low-energy-diet for relapse management during weight loss maintenance in the Diabetes Remission Clinical Trial (DiRECT). J Hum Nutr Diet. 2021;34(3):472–479. doi:10.1111/jhn.12839
40. Taylor R, Al-Mrabeh A, Sattar N. Understanding the mechanisms of reversal of type 2 diabetes. Lancet Diabetes Endocrinol. 2019;7(9):726–736. doi:10.1016/S2213-8587(19)30076-2
41. Dagenais GR, Gerstein HC, Zhang X, et al. Variations in Diabetes Prevalence in Low-, Middle-, and High-Income Countries: results from the Prospective Urban and Rural Epidemiology Study. Diabetes Care. 2016;39:780–787. doi:10.2337/dc15-2338
42. Adeyemo AA, Zaghloul NA, Chen G, et al. ZRANB3 is an African-specific type 2 diabetes locus associated with beta-cell mass and insulin response. Nat Commun. 2019;10(1):3195. doi:10.1038/s41467-019-10967-7
43. de Rooij SR, Roseboom TJ, Painter RC. Famines in the last 100 years: implications for diabetes. Curr Diab Rep. 2014;14(10):536. doi:10.1007/s11892-014-0536-7
44. Pembrey M, Saffery R, Bygren LO. Human transgenerational responses to early-life experience: potential impact on development, health and biomedical research. J Med Genet. 2014;51(9):563–572. doi:10.1136/jmedgenet-2014-102577
45. Utumatwishima JN, Chung ST, Bentley AR, Udahogora M, Sumner AE. Reversing the tide - diagnosis and prevention of T2DM in populations of African descent. Nat Rev Endocrinol. 2018;14(1):45–56. doi:10.1038/nrendo.2017.127
46. Obesity rising in Africa. WHO analysis finds; 2022. Available from: https://www.afro.who.int/news/obesity-rising-africa-who-analysis-finds.
47. Ishimwe MCS, Wentzel A, Shoup EM, et al. Beta-cell failure rather than insulin resistance is the major cause of abnormal glucose tolerance in Africans: insight from the Africans in America study. BMJ Open Diabetes Res Care. 2021;9(1):e002447. doi:10.1136/bmjdrc-2021-002447
48. Ladwa M, Bello O, Hakim O, et al. Ethnic differences in beta cell function occur independently of insulin sensitivity and pancreatic fat in black and white men. BMJ Open Diabetes Res Care. 2021;9(1):e002034. doi:10.1136/bmjdrc-2020-002034
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
