Back to Journals » Diabetes, Metabolic Syndrome and Obesity » Volume 15
A Retrospective Evaluation of Pregnancy Outcomes Following Bariatric Surgery: A Single-Center Experience
Authors Wang X, Liu J , He A, Dong Z, Chen X, Yu S, Gao L, Wang H, Chen W , Hu R, Jiang S, Wang J, Chen Y, Wang C, Yang W , Li R
Received 31 August 2022
Accepted for publication 10 November 2022
Published 25 November 2022 Volume 2022:15 Pages 3669—3678
DOI https://doi.org/10.2147/DMSO.S386773
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Konstantinos Tziomalos
Xiufang Wang,1,* Jia Liu,1,* Andong He,1 Zhiyong Dong,2– 4 Xiaomei Chen,2– 4 Shuqing Yu,2– 4 Lilian Gao,2– 4 Huaxi Wang,2– 4 Wenhui Chen,2– 4 Ruixiang Hu,2– 4 Shuwen Jiang,2– 4 Jianxue Wang,2– 4 Yuan Chen,2– 4 Cunchuan Wang,2– 4 Wah Yang,2– 4 Ruiman Li1
1Department of Obstetrics and Gynecology, The First Affiliated Hospital of Jinan University, Guangzhou, People’s Republic of China; 2Department of Metabolic and Bariatric Surgery, The First Affiliated Hospital of Jinan University, Guangzhou, People’s Republic of China; 3Jinan University Institute of Obesity and Metabolic Disorders, Guangzhou, People’s Republic of China; 4Guangdong-Hong Kong-Macao Joint University Laboratory of Metabolic and Molecular Medicine, Guangzhou, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Ruiman Li, Department of Obstetrics and Gynecology, The First Affiliated Hospital of Jinan University, No. 613, Huangpu Avenue West, Guangzhou, People’s Republic of China, Email [email protected] Wah Yang, Department of Metabolic and Bariatric Surgery, The First Affiliated Hospital of Jinan University, No. 613, Huangpu Avenue West, Guangzhou, People’s Republic of China, Email [email protected]; [email protected]
Background: Bariatric and metabolic surgery (BMS) is an effective treatment for obesity and its complications, but its effect on pregnancy outcomes is inconclusive. The present study aimed to investigate women’s pregnancy status and outcomes as well as the impact of pregnancy intervals after BMS.
Methods: The menstrual cycle and fertility status of women who underwent BMS in our centre between July 2010 and January 2021 were retrospectively analyzed and followed up until one-year post-delivery. The pregnancy outcomes after BMS were observed, including changes in weight, pregnancy interval, pregnancy complications, weight and health status of the newborn (premature birth, admission to neonatology, or deformity).
Results: We identified 31 women who were successfully conceived after BMS. There were statistical differences in weight and menstrual status before and post-operation (P < 0.05), and 77.97% of them had remission or recovery of obesity-related comorbidities. Eighteen patients delivered successfully after BMS, but there were still 12 cases of spontaneous abortion and 1 case of induced abortion. The abortion rate in pregnancy intervals less than 2 years was higher than those ≥ 2 years (P = 0.045). Of the women who delivered successfully, 5 had pregnancy-specific complications, including gestational diabetes mellitus and hypertensive disorder of pregnancy. However, the growth and development of the newborn are normal since the birth follow-up.
Conclusion: The present results suggest that the abortion rate in pregnancy intervals less than 2 years was higher than those ≥ 2 years. It is recommended that postoperative patients avoid pregnancy until their weight is stable to reduce the risk of adverse pregnancy outcomes.
Keywords: pregnancy, bariatric surgery, metabolic surgery, obesity
Introduction
Recently, the prevalence of obesity is increasing worldwide. More than one-third of adults are overweight or in severe obesity in China, and the overweight and obesity rates of Chinese women of reproductive age are 25.4% and 9.2%, respectively. However, the prevalence of severe obesity in China remains unclear.1–5 A variety of diseases caused by obesity have become a worldwide public health problem.6–9 Obesity can not only increase the risk of a series of noninfectious chronic diseases but also lead to many pregnancy complications and adverse pregnancy outcomes, such as miscarriage, premature delivery, hypertensive disorder complicating pregnancy, gestational diabetes mellitus, fetal abnormalities, postpartum haemorrhage, thrombosis and puerperal infection.10,11 Therefore, it is important for pregnant women to control the weight.
Many patients with severe obesity have received bariatric and metabolic surgery (BMS), including women of childbearing age.12–14 In China, the number of BMS in 2020 is 12,837, but the number of BMS performed in women of childbearing age is unclear.15 BMS for women of childbearing age also poses clinical challenges for subsequent pregnancies, requiring multidisciplinary collaboration for rigorous prenatal management. Bariatric and metabolic surgery for pregnancy has been reported to reduce the incidence of preeclampsia, gestational diabetes, and large for gestational age infants. Still, it may increase the risk of fetal growth restriction, preterm birth, neonatal intensive care unit hospitalization, and increased perinatal mortality.16,17 Short pregnancy intervals may also increase the risk of maternal morbidity and mortality.18 However, some studies have shown that pregnancy after BMS is not associated with adverse perinatal outcomes.19,20 There were also no significant differences in pregnancy complications and neonatal outcomes between women who conceived within the first 12 months of surgery and those who conceived later.21 Thus, the effect of BMS for women’s pregnancy outcomes could not be fully determined.
The existing evidence mainly comes from the population of western developed countries, which is not fully applicable to the Chinese population, and further research and discussion are needed. Therefore, in the present study, we reviewed the pregnancy and delivery outcomes of women undergoing BMS in our center, aiming to evaluate the impact of BMS on pregnancy.
Materials and Methods
Patients
Participants who were age ≥ 20 and underwent spontaneous and singleton pregnancy after BMS in the First Affiliated Hospital of Jinan University from July 2010 to January 2021 were included. Retrospective analysis of pregnancy outcomes and pregnancy complications after BMS was performed using the prospective managed database in our center. The follow-up of these patients after surgery and their relevant clinical information were obtained through the electronic medical record, questionnaire surveys, and telephone interviews. Information on BMS and 6 months after this surgery was obtained from the electronic medical record, and information on postoperative pregnancy was obtained from the questionnaire surveys and telephone interviews. WeChat, questionnaire star, and telephone were used for survey and interview. All patients met the criteria for BMS according to the Chinese Surgical Guidelines for Obesity and Type 2 Diabetes (2019) by the Chinese Society for Metabolic and Bariatric Surgery (CSMBS).22 Since the nature of the present study is retrospective and there were no interventions that may affect the patient’s interests as well as the included patients were not recontacted specifically for the study, it was orally approved by the Scientific and Ethics Review Committees of the First Affiliated Hospital of Jinan University and the informed consent and approval number for the study had been waived. Notably, the guidelines of the Declaration of Helsinki were followed, and all patient data was de-identified to achieve the confidentiality.
Surgical Procedures
Standard laparoscopic sleeve gastrectomy (LSG) and laparoscopic Roux-en-Y gastric bypass (LRYGB) were performed by a single surgeon and managed by the same surgical team. The surgical techniques were described previously.23
Clinical Parameters
Clinical data of the patients included preoperative weight, preoperative body mass index (BMI), types of surgeries, postoperative weight change and BMI, the interval from surgery to pregnancy, weight gain during pregnancy, post-delivery weight, postpartum one-year weight and BMI, miscarriage events, complications of pregnancy (including gestational diabetes mellitus, preeclampsia, intrahepatic cholestasis of pregnancy, etc.), and adverse birth outcomes (including preterm birth, stillbirth, small for gestational age, and birth defects). Notably, Questionnaire stars was used to directly ask patients whether their menstrual cycle was regular. For pregnant women with a pre-pregnancy BMI < 18.5, the weight-gain range should be 12.5–18.0 kg; for pregnant women with a pre-pregnancy BMI of 18.5–24.9, the weight-gain range should be 11.5–16.0 kg; for women with a pre-pregnancy BMI of 25.0–29.9, the weight-gain range should be 7.0~11.5 kg; For pregnant women with a pre-pregnancy BMI over 30.0, the weight gain should range from 5.0 to 9.0 kg. Below or above the abovementioned weight-gain range is defined as inadequate or excessive weight gain. For the convenience of statistics, cases with two or more births are included in the statistics with the first child.
Statistical Analysis
SPSS 23.0 statistical software was used to process and analyze the measured data. The missing data were replaced by the median of other non-zero data. Fisher’s exact test was used for comparing the counting data (total number of cases < 40). Student’s t-test (obeyed normal distribution) or nonparametric (did not obey normal distribution) test was used for comparing the measuring data. Friedman test was used for comparing preoperative and postoperative data, which did not follow a normal distribution. The test level was α = 0.05.
Results
Basic Characteristics of the Patients
Forty women of childbearing age who underwent BMS in our center were conceived spontaneously without receiving ovulation stimulation therapy or other medical treatment. Among them, four women who were unwilling to be followed up (consent rate: 90.0%, attrition rate: 10.0%), four women who were still pregnant, and one woman who was less than one year postpartum were excluded, 31 women were finally eligible for inclusion. The characteristics of these patients are shown in Table 1.
 |
Table 1 Changes in Weight and BMI Before BMS, During Pregnancy After BMS, and After Delivery |
Changes in Weight and BMI
Compared with pre-operation, the weight and BMI of the patients after the operation were significantly lower than before, and the mean difference at each observation time point was statistically significant (P < 0.05). For those who delivered after operation (n = 18), 9, 7, and 2 gained excessive, adequate, and inadequate weight during gestation, respectively. The BMI at conception was 25.67 (22.44, 31.60) kg/m2, of which 72.2% (n = 13) women had a BMI < 30 kg/m2; however, there were three patients had a BMI higher than 35 kg/m2. The weight post-delivery at one year was 70.50 (60.00–87.00) kg. The BMI was 27.17 (23.91, 30.02) kg/m2, of which only 22.2% (n = 4) recovered to the original weight (the lowest weight at the time of pregnancy was detected) within one year post delivery, and 77.8% (n = 14) still did not recover to the original weight within one year post delivery. More details are shown in Table 1 and Figure 1.
Menstrual Changes Pre- and Post-BMS
Seventeen patients had menstrual disorders before surgery, with an overall menstrual disorder rate of 54.84%, while 11 patients had normal menstruation after BMS, with a 64.71% improvement rate. After the operation, the total menstrual disorder rate was 19.35%, significantly lower than before. The difference in menstrual changes before BMS was statistically significant (P = 0.000), as shown in Table 2. In addition, we found that three patients with irregular menstruation had polycystic Ovary Syndrome (PCOS) before BMS and two of them normalized menstrual function postoperatively.
 |
Table 2 Menstrual Changes Before and Post Operation |
Comorbidities and Complications Pre- and Post-BMS
In our cohort, 96.77% of patients undergoing BMS had one or more obesity-related diseases before surgery, including dyslipidemia, uric acid abnormality, diabetes, sleep apnea syndrome and hypertension. Most of these comorbidities were relieved or even cured after the operation (77.97%) at the follow-up point in December, 2021. However, two patients with diabetes were still under control with drugs, and two patients with thyroid diseases continued to receive medical treatment. In addition, two patients developed symptoms of anaemia after the operation, and one patient developed dumping syndrome after the operation, as detailed in Table 3.
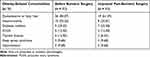 |
Table 3 Obesity-Related Comorbidities Before and Post-Operation |
Complications of Pregnancy and Pregnancy Outcomes
Twenty-two patients had never had a pregnancy before surgery, and nine had been conceived spontaneously. Eighteen cases were successfully delivered, but 12 cases still had a spontaneous abortion, and one patient had induced abortion due to a personal request. We compared the pregnancy outcomes with pregnancy intervals less than 2 years (n = 10) and ≥2 years (n = 20) and found that the abortion rate of pregnant women with pregnancy intervals less than 2 years was higher (P = 0.045), as detailed in Table 4. Table 5 shows the pregnancy characteristics of pregnant women who delivered successfully after BMS. Among them, five patients (27.78%) had pregnancy-specific complications, including gestational diabetes mellitus and hypertensive disorder of pregnancy. None of the patients had complications related to delivery. The growth and development of the newborn are normal since the birth follow-up.
 |
Table 4 Comparison of Results Based on Pregnancy Intervals in All Case |
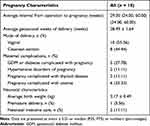 |
Table 5 Pregnancy Characteristics of Pregnant Women Who Delivered Successfully After Bariatric Surgery |
Comparison of Results Based on Pregnancy Intervals
In our postoperative successful delivery cohort, we compared the results of pregnancy between ≤ 24 months after BMS (A1) and > 24 months of pregnancy (A2). Among them, 50% (n = 9) of patients became pregnant less than 24 months after weight loss, and 50% (n = 9) became pregnant more than 24 months after the operation. In group A1, 33.3% underwent LSG, and 66.7% underwent LRYGB. In A2, 55.6% underwent LSG, and 44.4% underwent LRYGB. The study showed no significant difference in pregnancy weight, pregnancy weight gain, late pregnancy weight, postpartum weight, one-year postpartum weight, newborn birth weight, gestational age, delivery mode, and pregnancy complications between the two groups (P > 0.05). See Table 6 for details.
 |
Table 6 Comparison of Results Based on Pregnancy Intervals in Those with Successful Postoperative Delivery |
Comparison of Results Based on BMI at Conception
In our cohort of successful postoperative deliveries, we compared the differences between patients with BMI < 30 kg/m2 (B1) and BMI ≥ 30kg/m2 (B2) at conception. In B1, 7 (53.8%) patients had LSG and 6 (46.2%) had LRYGB. In B2, 1 (20%) had LSG and 4 (80%) had LRYGB. The study showed differences in weight in the third trimester of pregnancy, weight post-delivery, and weight in the first-year post-delivery between the two groups. At the same time, there were no significant differences in weight gain during pregnancy, birth weight of newborn, gestational age, mode of delivery, and complications of pregnancy (P > 0.05), indicating that BMI increased weight during pregnancy and pregnancy safety were the same at different times of conception. See Table 7 for details.
 |
Table 7 Comparison of Results Based on BMI at Conception |
Discussion
The present study aimed to observe women’s pregnancy status and outcomes after BMS. Our results indicate that pregnancy after BMS seems to exhibit certain risk. And it is recommended that postoperative patients avoid pregnancy until their weight is stable to reduce the risk of adverse pregnancy outcomes.
The incidence of overweight and obesity is increasing rapidly worldwide, and BMS is still the most effective way to treat severe obesity and its related complications.24 Studies have shown that BMS can contribute to dramatic weight loss, sustained at least 4 years after surgery, as well as help to achieve glycemic control in obese patients with uncontrolled type 2 diabetes.25,26 In the present study, patients’ average weight and BMI decreased by 25% within six months after the operation. The body weight of 72.2% of patients returned to normal at conception (BMI < 30 kg/m2). Thus, BMS has a significant effect on weight loss and can highlight the impact of surgery within a short period after the operation, which is consistent with the conclusions of previous studies.27
Additionally, BMS can also improve the symptoms of menstrual disorders in obese patients of childbearing age and improve women’s fertility. A study showed that 38.6% of women had menstrual dysfunction before the operation, and about 35.4% of patients returned to normal menstruation after BMS.28 In the present study, among the women with menstrual disorders before the operation, about 65% of the patients had regular menstruation recovery after an operation. However, there are still some patients whose menstruation has not recovered after the operation. The relationship between bariatric surgery and menstrual disorders remains to be further explored, and patients after BMS should continue to strengthen lifestyle management since menstruation may be affected by various factors.29
Studies have shown that more than half of the patients undergoing BMS are women of childbearing age, most of whom have reproductive needs.30 Overall, BMS helps to reduce the incidence of preeclampsia, gestational diabetes, and large for gestational age infants but increases the risk of small for gestational age infants (SGA).16,31,32 Gastric bypass is associated with a higher risk of SGA than other procedures, which may be related to malabsorption of nutrients during postoperative pregnancy.33 In particular, with rapid weight loss during the first 1–2 years after surgery, pregnancy has a higher risk of nutrient deficiency, leading to increased rates of fetal malnutrition and obstetric complications.18 Therefore, most scholars recommend delaying pregnancy after BMS for at least one year,34–37 but the evidence supporting this recommendation is insufficient. In addition, several studies have shown no association between interval time and adverse pregnancy or neonatal outcome and delaying pregnancy time does not appear to have any greater benefit.21,38–40 The present study compared pregnancy results two years after surgery with pregnancy after two years. We also found that the incidence of pregnancy complications and the newborn’s birth weight were not statistically significant between the two groups. However, we observed spontaneous abortion in up to 38% of pregnancies in the study cohort. The time interval from surgery to pregnancy was shorter in these patients than in live births after surgery. We further found that the abortion rate of pregnant women with pregnancy intervals less than 2 years was higher compared with those with pregnancy intervals ≥2 years. A previous study indicated that abortion occurred more often after RYGB (OR=9.81, 95% CI: 1.12–85.71),33 but other studies observed no change in abortion rate (38.7% vs 56.5%, P = 0.256).41 Therefore, the relationship between BMS and abortion was inconsistent, which needs more evidence.
In addition, during the follow-up, we found that anemia during pregnancy is a common problem. After BMS, changes in intestinal anatomy, poor absorption of trace elements, and increased nutritional requirements during pregnancy make pregnant women more prone to anemia. A recent systematic review also confirmed an increased risk of anemia and decreased ferritin levels in pregnancy after BMS.42 However, there is a close correlation between pregnancy anemia and adverse pregnancy outcomes.43 Therefore, the guidelines also recommend that nutritional supplementation be optimized 3 to 6 months before conception, and iron, ferritin, and transferrin levels should be regularly monitored to prevent and treat anemia during pregnancy.34,44
The present study had some limitations, such as this was a retrospective and single-institution study which may limit the generalizability of study results, and a relatively small sample size, resulting in insufficient statistical power. Additionally, the potential confounding variables could not be controlled. But to the best of our knowledge, this is the first study on pregnancy after BMS in the Chinese population, which may provide preliminary evidence for the effect of BMS for pregnancy. It added evidence for pregnancy safety after BMS in specific populations in China under the “one-child policy”. With the policy that has become more open in the past few years that people can have more than one child, future multicenter research can be conducted to clarify further the impact of BMS on pregnancy outcomes in female patients and their offspring.
Conclusions
The present study showed that BMS substantially impact weight control and management in women with obesity and can significantly improve most obesity-related comorbidities. The abortion rate in pregnancy intervals less than 2 years was higher than those ≥2 years. In addition, it is necessary to strengthen the intake of nutrients during postoperative pregnancy. For example, increasing iron supplements can reduce gestational anemia. Therefore, postoperative trace element supplements and monitoring are also essential.
Ethical Approval
The present study was performed based on the retrospective data, which was orally approved by the Scientific and Ethics Review Committees of the First Affiliated Hospital of Jinan University. Notably, the Scientific and Ethics Review Committees had waived informed consent and approval number for the study as the nature of the present study is retrospective.
Acknowledgment
The authors would like to thank all the staff in the Department of Obstetrics and Gynecology, and the Department of Metabolic and Bariatric Surgery for their help and assistance in the study.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Jia WP, Wang C, Jiang S, Pan JM. Characteristics of obesity and its related disorders in China. Biomed Environ Sci. 2010;23(1):4–11. doi:10.1016/S0895-3988(10)60025-6
2. Wang Y, Su C, Ouyang YF, et al. Secular trends in sedentary behaviors and associations with weight indicators among Chinese reproductive-age women from 2004 to 2015: findings from the China Health and Nutrition Survey. Int J Obes. 2020;44(11):2267–2278. doi:10.1038/s41366-020-00684-3
3. Wang Y, Wang L, Qu W. New national data show alarming increase in obesity and noncommunicable chronic diseases in China. Eur J Clin Nutr. 2017;71(1):149–150. doi:10.1038/ejcn.2016.171
4. Health Management Branch of Chinese Medical Association CNBoCNS, Medical Nutrition Industry Branch of National Health Industry Enterprise Management Association, Editorial Board of Chinese Journal of Health Management. Expert consensus on weight management process of overweight or obese people (2021). Chin J Health Manage. 2021;15(04):317–322. in Chinese.
5. Nutrition and Metabolic Management Branch of China Association for the Promotion of International Exchanges in Healthcare CNBoCNS, Diabetes Branch of Chinese Medical Association, Parenteral and Enteral Nutrition Branch of Chinese Medical Association, Nutrition Physician Professional Committee of Chinese Medical Doctor Association. Guidelines for medical nutritional treatment of overweight/obesity in China (2021). Chin J Front Med Sci. 2021;13(11):1–55. in Chinese.
6. Guidelines QC. Obesity and pregnancy (including post bariatric surgery). Guideline No MN2114-V6-R26 Queensland Health. 2021.
7. Bray GA, Heisel WE, Afshin A, et al. The science of obesity management: an endocrine society scientific statement. Endocr Rev. 2018;39(2):79–132. doi:10.1210/er.2017-00253
8. Schetz M, De Jong A, Deane AM, et al. Obesity in the critically ill: a narrative review. Intensive Care Med. 2019;45(6):757–769. doi:10.1007/s00134-019-05594-1
9. Finucane MM, Stevens GA, Cowan MJ, et al. National, regional, and global trends in body-mass index since 1980: systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 9.1 million participants. Lancet. 2011;377(9765):557–567. doi:10.1016/S0140-6736(10)62037-5
10. Wolfe BM, Kvach E, Eckel RH. Treatment of obesity: weight loss and bariatric surgery. Circ Res. 2016;118(11):1844–1855. doi:10.1161/CIRCRESAHA.116.307591
11. Ma RCW, Schmidt MI, Tam WH, McIntyre HD, Catalano PM. Clinical management of pregnancy in the obese mother: before conception, during pregnancy, and post partum. Lancet Diabetes Endocrinol. 2016;4(12):1037–1049. doi:10.1016/S2213-8587(16)30278-9
12. Angrisani L, Santonicola A, Iovino P, Formisano G, Buchwald H, Scopinaro N. Bariatric surgery worldwide 2013. Obes Surg. 2015;25(10):1822–1832. doi:10.1007/s11695-015-1657-z
13. Alatishe A, Ammori BJ, New JP, Syed AA. Bariatric surgery in women of childbearing age. QJM. 2013;106(8):717–720. doi:10.1093/qjmed/hct081
14. Yang W, Zhu S, Cheng Z, et al. Laparoscopic Roux-en-Y gastric bypass for excess weight and diabetes: a multicenter retrospective cohort study in China. Mini-Invasive Surg. 2021;5:11.
15. Group COaMSRC. Obesity and metabolic surgery database in China: 2020 annual report. Chin J Obes Metab Dis. 2021;7(1):1–7.
16. Akhter Z, Rankin J, Ceulemans D, et al. Pregnancy after bariatric surgery and adverse perinatal outcomes: a systematic review and meta-analysis. PLoS Med. 2019;16(8):e1002866. doi:10.1371/journal.pmed.1002866
17. Badreldin N, Kuller J, Rhee E, Brown L, Laifer S. Pregnancy management after bariatric surgery. Obstet Gynecol Surv. 2016;71(6):361–368. doi:10.1097/OGX.0000000000000322
18. Parent B, Martopullo I, Weiss NS, Khandelwal S, Fay EE, Rowhani-Rahbar A. Bariatric surgery in women of childbearing age, timing between an operation and birth, and associated perinatal complications. JAMA Surg. 2017;152(2):128–135. doi:10.1001/jamasurg.2016.3621
19. Sheiner E, Levy A, Silverberg D, et al. Pregnancy after bariatric surgery is not associated with adverse perinatal outcome. Am J Obstet Gynecol. 2004;190(5):1335–1340. doi:10.1016/j.ajog.2003.11.004
20. Abodeely A, Roye GD, Harrington DT, Cioffi WG. Pregnancy outcomes after bariatric surgery: maternal, fetal, and infant implications. Surg Obes Relat Dis. 2008;4(3):464–471. doi:10.1016/j.soard.2007.08.018
21. Malakauskiene L, Nadisauskiene RJ, Ramasauskaite D, Bartuseviciene E, Ramoniene G, Maleckiene L. Is it necessary to postpone pregnancy after bariatric surgery: a national cohort study. J Obstet Gynaecol. 2020;40(5):614–618. doi:10.1080/01443615.2019.1634024
22. Yang W, Wang C. Metabolic surgery needs stronger endorsement in Asian T2DM patients with low BMI. Obes Surg. 2022;32(1):212–213. doi:10.1007/s11695-021-05636-y
23. Hu S, Huang B, Loi K, et al. Patients with Prader-Willi Syndrome (PWS) underwent bariatric surgery benefit more from high-intensity home care. Obes Surg. 2022;32(5):1631–1640. doi:10.1007/s11695-022-05999-w
24. Rozier MD, Ghaferi AA, Rose A, Simon NJ, Birkmeyer N, Prosser LA. Patient preferences for bariatric surgery: findings from a survey using discrete choice experiment methodology. JAMA Surg. 2019;154(1):e184375. doi:10.1001/jamasurg.2018.4375
25. Douglas IJ, Bhaskaran K, Batterham RL, Smeeth L. Bariatric surgery in the United Kingdom: a cohort study of weight loss and clinical outcomes in routine clinical care. PLoS Med. 2015;12(12):e1001925. doi:10.1371/journal.pmed.1001925
26. Schauer PR, Kashyap SR, Wolski K, et al. Bariatric surgery versus intensive medical therapy in obese patients with diabetes. N Engl J Med. 2012;366(17):1567–1576. doi:10.1056/NEJMoa1200225
27. Courcoulas AP, Christian NJ, Belle SH, et al. Weight change and health outcomes at 3 years after bariatric surgery among individuals with severe obesity. JAMA. 2013;310(22):2416–2425. doi:10.1001/jama.2013.280928
28. Rozanska-Waledziak A, Bartnik P, Kacperczyk-Bartnik J, Czajkowski K, Waledziak M. The impact of bariatric surgery on menstrual abnormalities-a cross-sectional study. Obes Surg. 2020;30(11):4505–4509. doi:10.1007/s11695-020-04840-6
29. Vyver E, Steinegger C, Katzman DK. Eating disorders and menstrual dysfunction in adolescents. Ann N Y Acad Sci. 2008;1135:253–264. doi:10.1196/annals.1429.013
30. Edison E, Whyte M, van Vlymen J, et al. Bariatric surgery in obese women of reproductive age improves conditions that underlie fertility and pregnancy outcomes: retrospective cohort study of UK National Bariatric Surgery Registry (NBSR). Obes Surg. 2016;26(12):2837–2842. doi:10.1007/s11695-016-2202-4
31. Johansson K, Cnattingius S, Naslund I, et al. Outcomes of pregnancy after bariatric surgery. N Engl J Med. 2015;372(9):814–824. doi:10.1056/NEJMoa1405789
32. Getahun D, Fassett MJ, Jacobsen SJ, et al. Perinatal outcomes after bariatric surgery. Am J Obstet Gynecol. 2022;226(1):121e1–e16 . doi:10.1016/j.ajog.2021.06.087
33. Goldman RH, Missmer SA, Robinson MK, Farland LV, Ginsburg ES. Reproductive outcomes differ following roux-en-y gastric bypass and adjustable gastric band compared with those of an obese non-surgical group. Obes Surg. 2016;26(11):2581–2589. doi:10.1007/s11695-016-2158-4
34. Shawe J, Ceulemans D, Akhter Z, et al. Pregnancy after bariatric surgery: consensus recommendations for periconception, antenatal and postnatal care. Obes Rev. 2019;20(11):1507–1522. doi:10.1111/obr.12927
35. Heber D, Greenway FL, Kaplan LM, et al. Endocrine and nutritional management of the post-bariatric surgery patient: an Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab. 2010;95(11):4823–4843. doi:10.1210/jc.2009-2128
36. Busetto L, Dicker D, Azran C, et al. Practical recommendations of the obesity management task force of the European Association for the study of obesity for the post-bariatric surgery medical management. Obes Facts. 2017;10(6):597–632. doi:10.1159/000481825
37. American College of Obstetricians and Gynecologists. ACOG practice bulletin no. 105: bariatric surgery and pregnancy. Obstet Gynecol. 2009;113(6):1405–1413. doi:10.1097/AOG.0b013e3181ac0544
38. Sancak S, Celer O, Cirak E, et al. Timing of gestation after Laparoscopic Sleeve Gastrectomy (LSG): does it influence obstetrical and neonatal outcomes of pregnancies? Obes Surg. 2019;29(8):2629–2630. doi:10.1007/s11695-019-03959-5
39. Mahmoudieh M, Keleidari B, Shahabi S, et al. Pregnancy less than 1 year after the bariatric surgery: is it really safe? Obes Surg. 2021;31(5):2211–2218. doi:10.1007/s11695-021-05260-w
40. Sheiner E, Edri A, Balaban E, Levi I, Aricha-Tamir B. Pregnancy outcome of patients who conceive during or after the first year following bariatric surgery. Am J Obstet Gynecol. 2011;204(1):50 e1–6. doi:10.1016/j.ajog.2010.08.027
41. Grzegorczyk-Martin V, Freour T, De Bantel Finet A, et al. IVF outcomes in patients with a history of bariatric surgery: a multicenter retrospective cohort study. Hum Reprod. 2020;35(12):2755–2762. doi:10.1093/humrep/deaa208
42. Rottenstreich A, Elazary R, Goldenshluger A, Pikarsky AJ, Elchalal U, Ben-Porat T. Maternal nutritional status and related pregnancy outcomes following bariatric surgery: a systematic review. Surg Obes Relat Dis. 2019;15(2):324–332. doi:10.1016/j.soard.2018.11.018
43. Lin L, Wei Y, Zhu W, et al. Prevalence, risk factors and associated adverse pregnancy outcomes of anaemia in Chinese pregnant women: a multicentre retrospective study. BMC Pregnancy Childbirth. 2018;18(1):111. doi:10.1186/s12884-018-1739-8
44. Yang W, Abbott S, Borg CM, et al. Global variations in preoperative practices concerning patients seeking primary bariatric and metabolic surgery (PACT Study): a survey of 634 bariatric healthcare professionals. Int J Obes. 2022;46(7):1341–1350. doi:10.1038/s41366-022-01119-x
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

