Back to Journals » Therapeutics and Clinical Risk Management » Volume 13
A rare case of lung carcinoma acquires multidrug-resistant Klebsiella pneumoniae pneumonia radiologically mimicking metastasis caused by nivolumab therapy-associated neutropenia
Authors Liu C, Ding L, Zhu Y, Chen C
Received 23 June 2017
Accepted for publication 11 August 2017
Published 12 October 2017 Volume 2017:13 Pages 1375—1377
DOI https://doi.org/10.2147/TCRM.S144681
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Deyun Wang
Chao Liu,* Ling Ding,* Ye-han Zhu, Cheng Chen
Respiratory Department, The First Affiliated Hospital of Soochow University, Suzhou, People’s Republic of China
*These authors contributed equally to this work
Abstract: Nosocomial infections by Klebsiella pneumoniae, especially those due to multidrug-resistant strains, are being increasingly detected. In this report, we present the case of a 63-year-old man with lung squamous carcinoma who received nivolumab therapy due to failure of first-line chemotherapy. This report also demonstrates an association of nivolumab therapy and neutropenia, and supports the use of a combination of tigecycline and meropenem in managing hospitalization-acquired pneumonia caused by multidrug-resistant K. pneumoniae. It also implicates that a further evaluation is required in lung cancer patients with a suspected metastatic or recurrent carcinoma, and an antibiotic therapy is valuable in ruling out a potential lung infection since a risk of hospitalization-acquired pneumonia may exist.
Keywords: hospitalization-acquired pneumonia, nivolumab, neutropenia, lung carcinoma, multidrug-resistant Klebsiella pneumoniae
Introduction
Multidrug-resistant Klebsiella pneumoniae (MDR-Kp) affecting lung tissue or bloodstream is a life-threatening disease, especially for patients with poor immunity. Its early recognition and treatment is one of the most important factors for improving patient survival.1 The dearth of effective treatment against MDR-Kp infections, and neutropenia and other immunological defects observed in patients with malignancies are the two major obstacles that make the outcome even worse.
Nivolumab is the first PD-1 inhibitor approved for use in patients with unresectable melanoma and lung cancer. It has been found that nivolumab therapy is associated with development of certain adverse events such as all-grade endocrine, cutaneous, hepatic and gastrointestinal toxicities, which are commonly described as immune-related adverse events (irAEs).2,3 In this report, we present a rare case of lung squamous carcinoma, which developed MDR-Kp pneumonia caused by nivolumab therapy-associated neutropenia.
Case
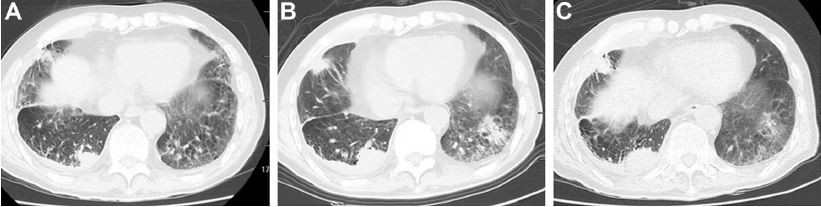
A 63-year-old man with lung squamous carcinoma and right pleural metastasis received nivolumab therapy due to failure of the first-line chemotherapy.4,5 Clinically, it was found that the primary lesion achieved rapid and partial remission, but the secondary fibrosis became more complicated after nivolumab treatment. After administering methylprednisolone, the radiological findings showed carcinoma regression.6 Three weeks after starting the nivolumab treatment, the patient was noticed having serious neutropenia (0.43×1012/L), and newly developed fever as well as purulent sputum. Although neutropenia was completely cured by using G-CSF, infection by MDR-Kp was reported by microbiological culture assay. The strain is resistant to β-lactams, sulfonamides and quinolones. In addition, occurrence of a new lesion in the lower lobe of the left lung suspected to be carcinoma metastasis was revealed by chest CT. At that point, an antibiotic therapy was decided to be administered and adjusted according to the susceptibility of MDR-Kp. Following treatment with tigecycline and meropenem for <2 weeks, the lesion in the lower lobe of the left lung was well controlled (Figures 1 and 2). The patient’s legally authorized representative provided written informed consent for the patient’s information and images to be included in this report. This case report was approved by the Ethics and Review Committee of the First Affiliated Hospital of Soochow University.
  | Figure 1 Overview of the clinical manifestation, monitoring and therapy from starting nivolumab administration (D0). |
Discussion
Infection is a common complication of chemotherapy in patients with malignancies. A number of novel targeted cancer therapies have been shown to decrease the risk of neutropenia; however, if a neutropenia-associated infection occurs, it will lead to a high rate of morbidity and mortality, prolonged length of hospitalization and significant economic losses. Here, we described a case of delayed hematological toxicity caused by nivolumab and its potential association with the hospitalization-acquired MDR-Kp pneumonia. However, it is unclear how nivolumab could cause delayed neutropenia, as it is generally not considered a cytotoxic chemotherapeutic agent causing neutropenia.
K. pneumoniae is one of the most important pathogens present in hospitals, and the multidrug-resistant strain is particularly concerning. Unresolved neutropenia, septic shock and failure of monotherapy are independent predictors of death.7 Another treatment-related factor that could affect the outcome is the time of initiation of the effective antimicrobial treatment. This report illustrates a possible association of neutropenia and MDR-Kp infection. The susceptibility of the neutropenic cancer patient reported here to MDR-Kp may partly be due to the long-term therapy with immunosuppressive methylprednisolone administered for his secondary pulmonary fibrosis.
In fact, the patient received an empirical antimicrobial therapy when neutropenia was noticed. However, the delayed initiation of active treatment targeting MDR-Kp did affect the association between neutropenia and MDR-Kp infection. The efficacy of monotherapy with an aminoglycoside, colistin or tigecycline against MDR-Kp infections has been questioned by several studies, and particularly among patients in septic shock and in those with severe underlying diseases. Moreover, it has also been shown that aminoglycosides and polymyxins, when administered as single agents, are ineffective against Gram-negative infections in patients with a neutrophil count <100 cells/mm3.8–10 Unlike monotherapy, combination therapy has been found to be more effective and associated with a lower mortality rate. The MDR-Kp infection in the patient reported here was successfully managed with a combination of carbapenem and tigecycline.
Further evaluation is required in patients with a suspected metastatic and recurrent carcinoma, and an antibiotic therapy is valuable in these patients since a risk of hospitalization-acquired pneumonia may exist. The findings of this report may assist physicians in making treatment decisions for neutropenic cancer patients found to have abnormality in their chest images to reduce the risk of misdiagnosing infectious lesions as tumor metastasis.11
Taken together, in addition to irAEs, neutropenia might continue to be an issue in patients with malignancies receiving immune checkpoint inhibitor therapy. This case report supports the use of combination of tigecycline and meropenem in managing hospitalization-acquired pneumonia caused by MDR-Kp.
Acknowledgment
The authors thank Professor Jim Xiang (Cancer Research Unit, Saskatchewan Cancer Agency, University of Saskatchewan, Saskatoon, SK, Canada) for providing constructive criticism and helpful suggestions for improving this manuscript. This work was supported by the Project of National Natural Science Foundation of China (81672280), Key Laboratory of Suzhou City (SZS201617), Clinical Medical Center of Suzhou (SZZX201502), Jiangsu Province’s Key Discipline of Medicine (ZDXKB2016007) and Medical Youth of Jiangsu Province (QNRC2016748).
Disclosure
The authors report no conflicts of interest in this work.
References
Tumbarello M, Trecarichi EM, De Rosa FG, et al; ISGRI-SITA (Italian Study Group on Resistant Infections of the Società Italiana Terapia Antinfettiva). Infections caused by KPC-producing Klebsiella pneumoniae: differences in therapy and mortality in a multicentre study. J Antimicrob Chemother. 2015;70(7):2133–2143. | ||
Lian ZZ, Sun YF, Chen C. Partial remission of hepatic metastatic lesion but complicated with secondary and refractory fever lead by nivolumab in a patient with lung adenocarcinoma presenting gefitinib acquired resistance. Chin Med J (Engl). 2016;129(7):879–880. | ||
Freeman-Keller M, Kim Y, Cronin H, Richards A, Gibney G, Weber JS. Nivolumab in resected and unresectable metastatic melanoma: characteristics of immune-related adverse events and association with outcomes. Clin Cancer Res. 2016;22(4):886–894. | ||
Gettinger SN, Horn L, Gandhi L, et al. Overall survival and long-term safety of Nivolumab (anti-programmed death 1 antibody, BMS-936558, ONO-4538) in patients with previously treated advanced non-small-cell lung cancer. J Clin Oncol. 2015;33(18):2004–2012. | ||
Brahmer J, Reckamp KL, Baas P, et al. Nivolumab versus docetaxel in advanced squamous-cell non-small-cell lung cancer. N Engl J Med. 2015;373(2):123–135. | ||
Ding L, Zhu Y, Chen C. Rapid and partial remission of primary lesion but complicated by secondary fibrosis after treatment with nivolumab in a lung squamous carcinoma. Ther Adv Respir Dis. 2017;11(2):129–132. | ||
Tofas P, Skiada A, Angelopoulou M, et al. Carbapenemase-producing Klebsiella pneumoniae bloodstream infections in neutropenic patients with haematological malignancies or aplastic anaemia: analysis of 50 cases. Int J Antimicrob Agents. 2016;47(4):335–339. | ||
Tumbarello M, Viale P, Viscoli C, et al. Predictors of mortality in bloodstream infections caused by Klebsiella pneumoniae carbapenemase-producing K. pneumoniae: importance of combination therapy. Clin Infect Dis. 2012;55(7):943–950. | ||
Daikos GL, Tsaousi S, Tzouvelekis LS, et al. Carbapenemase-producing Klebsiella pneumoniae bloodstream infections: lowering mortality by antibiotic combination schemes and the role of carbapenems. Antimicrob Agents Chemother. 2014;58(4):2322–2328. | ||
Tzouvelekis LS, Markogiannakis A, Piperaki E, Souli M, Daikos GL. Treating infections caused by carbapenemase-producing Enterobacteriaceae. Clin Microbiol Infect. 2014;20(9):862–872. | ||
Chen C, Zhu YH, Qian HY, Huang JA. Pulmonary tuberculosis with false-positive 18F-fluorodeoxyglucose positron emission tomography mimicking recurrent lung cancer: a case report. Exp Ther Med. 2015;9(1):159–161. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.