Back to Journals » Clinical Ophthalmology » Volume 11
A quality of life study comparing scleral buckle and pneumatic retinopexy for the treatment of rhegmatogenous retinal detachment
Authors Gauthier AC, Adelman RA
Received 16 March 2017
Accepted for publication 1 May 2017
Published 6 June 2017 Volume 2017:11 Pages 1069—1071
DOI https://doi.org/10.2147/OPTH.S137227
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Angela C Gauthier, Ron A Adelman
Department of Ophthalmology and Visual Science, Yale School of Medicine, New Haven, CT, USA
Patients who have undergone surgical treatment for retinal detachment may have significantly impaired visual-related quality of life.1 Although there are many studies that compare the visual outcomes and anatomical success of scleral buckle and pneumatic retinopexy in treating retinal detachment, there are inadequate data contrasting quality of life measures between these two approaches.2,3 A recent Cochrane review found that patients who underwent pneumatic retinopexy may be more likely to have recurrence of detachment but less likely to have choroidal detachment or a myopic shift than those who had scleral buckle.4 They concluded that there is still a dearth of important patient-centered information such as quality of life outcomes with these procedures.4 This study aimed to compare quality of life between patients who underwent scleral buckle or pneumatic retinopexy for treatment of rhegmatogenous retinal detachment.
Introduction
Patients who have undergone surgical treatment for retinal detachment may have significantly impaired visual-related quality of life.1 Although there are many studies that compare the visual outcomes and anatomical success of scleral buckle and pneumatic retinopexy in treating retinal detachment, there are inadequate data contrasting quality of life measures between these two approaches.2,3 A recent Cochrane review found that patients who underwent pneumatic retinopexy may be more likely to have recurrence of detachment but less likely to have choroidal detachment or a myopic shift than those who had scleral buckle.4 They concluded that there is still a dearth of important patient-centered information such as quality of life outcomes with these procedures.4 This study aimed to compare quality of life between patients who underwent scleral buckle or pneumatic retinopexy for treatment of rhegmatogenous retinal detachment.
Methods
Patients who underwent either scleral buckle or pneumatic retinopexy for rhegmatogenous retinal detachment at the Yale Eye Center between January 1993 and December 2013 were identified. A modified version of the National Eye Institute Visual Function Questionnaire-25 (VFQ-25) was administered by mail or phone interview to patients within 8 years after their surgery.5 For data received from respondents, results were calculated by subgroup analysis of the VFQ-25, independent two-tailed t-test, and a chi-squared test.
The study was reviewed and approved by the Yale University Institutional Review Board, which found that written informed consent could be waived because the research presented no more than minimal risk of harm to subjects. All subjects were provided an information sheet or given verbal information that described the risks and benefits of the study, and the decision to participate in the survey was considered consent.
Results
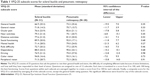
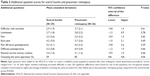
Fifty-nine patients participated in the survey, including 31 scleral buckle patients and 28 pneumatic retinopexy patients. There was no difference in VFQ-25 composite scores between scleral buckle (78.9±19.0) and pneumatic retinopexy (81.1±19.0) patients (P=0.64). Both groups scored similarly in general health, general vision, ocular pain, near activities, distance activities, social functioning, mental health, role difficulties, dependency, driving, color vision, and peripheral vision (Table 1). Also, there were no significant differences found for any of the additional postoperational questions (Table 2). There was a trend toward a higher percentage (85%) of pneumatic retinopexy patients preferring to have the same procedure in their fellow eye compared to scleral buckle patients (59%, P=0.06).
Discussion
These findings suggest that patients who had scleral buckle or pneumatic retinopexy treatment have a similar postoperative quality of life. Indeed, primary and overall surgical success rates appear to be similar in the two treatments.6,7 In addition, studies have generally found comparable final visual acuity outcomes in patients with uncomplicated rhegmatogenous retinal detachment.2
Although this effect did not reach statistical significance due to small sample size, it is interesting that a much lower proportion of scleral buckle patients than pneumatic retinopexy patients may choose to repeat the procedure, although both groups now enjoy similar levels of quality of life. Pneumatic retinopexy is a newer, quicker, less expensive, and less invasive procedure than scleral buckle.8,9 Perhaps the differences in likelihood to reelect the procedure are due to factors not assessed in this survey. In addition, it is possible that there exist postoperative pain and recovery differences between the groups, but they simply did not reach statistical significance due to sample size. If pneumatic retinopexy patients experienced an easier recovery than patients in the scleral buckle group, it may explain why they are more likely to choose the procedure again.
A few limitations of this study can be identified. For example, patients completed surveys at variable times up to 8 years following their surgeries given the study’s retrospective design. In addition, we excluded patients who underwent reoperation for subsequent retinal detachment, as our primary endpoint focused on those patients who underwent one of two single procedures. The sample size of 59 patients is relatively small because many patients with uncomplicated rhegmatogenous retinal detachment undergo vitrectomy or a combination of procedures. Future work involving a larger patient cohort, randomization to scleral buckle or pneumatic retinopexy in a prospective fashion, and multi-institutional collaboration may further elucidate quality of life measures depending on the specific surgical approach. We also suggest administering the VFQ-25 both pre- and postoperatively to better compare patients’ baseline with follow-up opinions on their vision quality of life.
Conclusion
Patients who had scleral buckle or pneumatic retinopexy had a similar postoperative quality of life, although scleral buckle is more invasive. However, there was a trend toward a higher percentage of patients preferring to have the same procedure on their fellow eye in the pneumatic retinopexy group than the scleral buckle group, suggesting that quality of life is not the only factor that determines patient preferences.
Acknowledgments
We would like to acknowledge Modjtaba Amirahmadi, MD, for his help with data collection. This project was supported by Leir Foundation, Newman’s Own Foundation, Research to Prevent Blindness, and Grant Number T35HL007649 from the National Heart, Lung and Blood Institute. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Heart, Lung, and Blood Institute or the National Institutes of Health.
Author contributions
All authors contributed toward data analysis, drafting and critically revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
Smretschnig E, Falkner-Radler CI, Binder S, et al. Vision-related quality of life and visual function after retinal detachment surgery. Retina. 2016;36(5):967–973. | ||
Saw SM, Gazzard G, Wagle AM, Lim J, Au Eong KG. An evidence-based analysis of surgical interventions for uncomplicated rhegmatogenous retinal detachment. Acta Ophthalmol Scand. 2006;84(5):606–612. | ||
Adelman RA, Parnes AJ, Ducournau D. Strategy for the management of uncomplicated retinal detachments: the European vitreo-retinal society retinal detachment study report 1. Ophthalmology. 2013;120(9):1804–1808. | ||
Hatef E, Sena DF, Fallano KA, Crews J, Do DV. Pneumatic retinopexy versus scleral buckle for repairing simple rhegmatogenous retinal detachments. Cochrane Database Syst Rev. 2015;(5):CD008350. | ||
Mangione CM, Lee PP, Gutierrez PR, Spritzer K, Berry S, Hays RD. Development of the 25-item National Eye Institute Visual Function Questionnaire. Arch Ophthalmol. 2001;119(7):1050–1058. | ||
Ellakwa AF. Long term results of pneumatic retinopexy. Clin Ophthalmol. 2012;6:55–59. | ||
Schwartz SG, Kuhl DP, McPherson AR, Holz ER, Mieler WF. Twenty-year follow-up for scleral buckling. Arch Ophthalmol. 2002;120(3):325–329. | ||
Goldman DR, Shah CP, Heier JS. Expanded criteria for pneumatic retinopexy and potential cost savings. Ophthalmology. 2014;121(1):318–326. | ||
Holz ER, Mieler WF. View 3: the case for pneumatic retinopexy. Br J Ophthalmol. 2003;87(6):787–789. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.