Back to Journals » Pediatric Health, Medicine and Therapeutics » Volume 10
A qualitative study of children’s quality of life in the context of living with cleft lip and palate
Authors Zeraatkar M , Ajami S , Nadjmi N, Faghihi SA , Golkari A
Received 4 May 2018
Accepted for publication 17 August 2018
Published 18 January 2019 Volume 2019:10 Pages 13—20
DOI https://doi.org/10.2147/PHMT.S173070
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Roosy Aulakh
Maryam Zeraatkar,1 Shabnam Ajami,2 Nasser Nadjmi,3 Seyad Aliakbar Faghihi,4 Ali Golkari1
1Oral and Dental Disease Research Center, Department of Dental Public Health, Shiraz University of Medical Sciences, Shiraz, Iran; 2Orthodontic Research Center, Department of Orthodontics, Shiraz University of Medical Sciences, Shiraz, Iran; 3Department of Cranio-Maxillofacial Surgery, Antwerp University Hospital, Antwerpen, Belgium; 4Clinical Educational Research Center, Shiraz University of Medical Sciences, Shiraz, Iran
Background and objective: Quality-of-life measures have been expanded to help in assessing the physical and psychosocial effects of oral health. Although, in the case of children undergoing oral surgery, the oro-facial status is generally measured by studies, it is essential to carry out investigations into the level of quality of life (QoL) after surgery to assess the actual effect of these surgeries on children’s lives. Hence, our study is aimed at evaluating the QoL in these children.
Methods: The study was performed using qualitative content analysis method. Eighteen caregivers of 4–6 year old children with a history of unilateral cleft lip and palate participated in in-depth interviews about the children’s experiences with different problems affecting their daily lives. The results were divided into codes, sub-categories and categories through an inductive process in which the researchers moved from the specific to the general.
Result: A number of problems were identified, particularly insufficient functional and socio-emotional well-being including, difficulty in eating and speaking, dento-facial problems, shame, anxiety, insufficient peer interaction and dissatisfaction with their own appearance.
Conclusion: The most critical problems derived from the participants’ experiences were insufficient functional and socio-emotional well-being that contributed to the reduced QoL among these children. Long term multidisciplinary interventional strategies such as psycho-social supportive programs are required to improve the QoL of these children. These interventions should be considered from the early stages of treatment, or even early stages of diagnosis.
Keywords: children, cleft lip, cleft palate, quality of life
Introduction
The World Health Organization’s definition of health as both the absence of disease and the presence of factors that promote physical, mental and social well-being has led to a broader concept of overall health, which necessarily results in quality of life (QoL).1 Given the extent of oral diseases, they are the main public health problem accounting for disability in every part of the world. The pain, suffering, impairment of functions like eating, chewing, smiling and communicating, and the reduced QoL means that the effect of oral diseases on individuals and communities is significant.2
Oro-facial clefts are one of the most widespread birth defects. In general, oro-facial clefts are classified into a cleft lip either with or without a cleft palate (CL±P) or a cleft palate only (CP).3 These defects create a high burden of disease owing to their complexity and effects on all aspects of life of both patients and their families. The prevalence of oral clefts is about 9.92 per 10,000 live births.4 In Iran, the incidence of oral cleft is reported to be about 1.0 per 1,000 live births.5
In addition to the physical defect, oro-facial clefts are associated with a large number of problems, such as speech disorder, hearing deficit, chronic ear infection (serious otitis media), dental and palatal deformities, and psychosocial problems.6 The success of medical treatment of these children is not merely defined by mending the cleft, but also extends to the maintenance or improvement of the children’s QoL after surgery,7 particularly for children with chronic health conditions and children with craniofacial abnormalities, who need long-term treatment protocols.8
Hence, evaluating the QoL has become an inseparable part of evaluating health programmes.9 QoL measures were expanded to assess the physical and psychosocial effect of oral health. Attempts were made to quantify the extent to which dental and oral disorders interfered with daily life and well-being as well as with the outcomes of clinical care like the effectiveness of treatment interventions.10 Speech and esthetic concerns appear to have been the crucial factors influencing health-related QoL after surgery in these children.8,11 Moreover, significant psychological and social burdens have been reported in relation to oro-facial clefts. Psychological adjustment tends to be challenging for children with oro-facial clefts in view of esthetic concerns, speech and hearing disabilities, and difficulty in acquiring social skills, which are essential for adjustment.11
Although the oro-facial status has been generally measured by studies, it is essential to carry out investigations into the level of QoL after surgery to measure the actual effect of these surgeries on the children’s lives. Several studies have investigated the QoL for adolescents and adults with oral clefts.12–14 However, only a few have attempted to measure the QoL of children with this condition,15 and none of these was a qualitative study for a better understanding of QoL in these children. Hence, this paper aims to clarify the influencing factors that affect QoL in these children, based on their caregivers’ experiments through a qualitative study.
Participants and methods
This qualitative study was conducted on children who were referred to the Oral Cleft Department/Research Center of Shiraz University of Medical Science, which is the most important specialized center for administration of infants and young children with cleft lip and palate (CLP) in southern Iran. Numerous patients are referred to this center for therapeutic services. As a result, this center provided the opportunity for collecting data for the aforementioned investigatory purposes.
Eighteen 4–6 year old children with a history of unilateral CLP who had undergone common methods of cleft repair surgery before the age of two were selected. The study participants were selected using the purposive sampling method. They were all under follow-up care in the above-mentioned center and had complete documentation. Their caregivers were invited to participate in this comprehensive study (Table 1). Data were obtained using semi-structured interviews. The “codes”, “sub-categories” and “categories” were explored through an inductive process, in which the researchers moved from the specific to the more general.
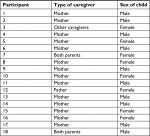  | Table 1 Participants’ characteristics |
The study was performed using the qualitative content analysis method. In the beginning, semi-structured, in-depth interviews as well as field notes were used as the strategy for data collection. The purposive sampling continued until saturation was reached, ie, no further information was obtained for the resulting concept. Each interview took an average of 45 minutes. The interview guide included a short list of general questions, eg, “What are the problems of children with oral clefts?” and “What kinds of problem did you experience during raising your child?” The questions were followed up with the participants’ experiences; for instance, they were asked to give more examples or clarify their reasons for describing the topic mentioned in the question. The interviews were recorded with the consent of the interviewees. The interviews were listened to by the principal investigator several times, and ambiguities were resolved by checking the transcript data with the participants over the phone soon after the interview. Then the meaning units and parts of data, which were directly related to the research questions, were identified. Subsequently, data analysis was performed based on Graneheim et al.16 To find similarities and differences, the preliminary codes were read several times and compared. Finally, sub-categories were developed and integrated to the categories.
Rigor
The credibility of the data was established by the triangulation strategy, which uses a specialized team combination to examine the findings. Besides semi-structured interviews, notetaking during interviews was used to ensure data credibility.17 Moreover, data dependability was assessed using both peer and member checking.18 The primary findings of the study along with the preliminary codes and categories were presented to some of the participants, and their opinion was obtained (member checking). Some parts of the data were analyzed by other colleagues who were not involved in the study (peer checking) in which the similarities with the current analysis came into view.17 In addition, the findings were repeatedly assessed and checked by supervisors (expert checking). Evidence from other studies, ideas from other researchers and documentation of the study helped to improve the confirmability.19 Finally, by providing a comprehensive description of the topics, participants, data collection and analysis procedures, and limitations of the study, we hope to have created transferability so that other researchers may clearly follow the research process taken by the researchers.17,18
Ethical approval
This study was approved by the local Ethics Committee of Shiraz University of Medical Sciences (ref. no. 95-01-03-11604) and written informed consent was taken from all participants. At the beginning of the interview, the participants acquainted themselves with the purpose of the study, method of interviewing, privacy, and confidentiality of the study. The interviews were set up individually, at a place suggested by the interviewees at an agreed time. The interviewees were allowed to leave the study at any time.
Results
In the present study, regarding QoL in the 4–6 year old children with a history of CLP, the experience and perceptions of these children’s caregivers were explored. As presented in Table 2, according to data analysis, two categories containing several sub-categories and codes were extracted, including insufficient functional well-being and insufficient socio-emotional well-being. Each category is described in more detail below.
  | Table 2 Examples of extracted codes, sub-categories and categories |
Insufficient functional wellbeing
The caregivers’ experiences indicated that the children lacked functional well-being. They have impairments in their everyday functions. This concept, which was frequently observed in our results, contained four more related sub-categories, including difficulty eating, difficulty speaking and dento-facial problems.
Difficulty eating
Based on the participants’ experiences, the first category consisted of three major codes, which refer to difficulty in incising foods with anterior teeth, difficulty in chewing hard foods with posterior teeth and regurgitating food and liquid from the nose.
From the view point of the participants, the inability to incise food with the anterior teeth is one of their major problems. In this regard, one of the participants stated: “My child does not like eating apple because he cannot bite it comfortably”
According to our participants’ experience, these patients face some difficulties in chewing hard foods using their posterior teeth. They have a tendency to consume soft and chopped foods. For instance, one of the participants stated: “I am forced to make soup for my child every day because she cannot eat hard food.”
The regurgitation of food and liquids from the nose is one unique experience in the affected children. One of the participants stated: “Due to liquid regurgitation from the nose, my child refuses to drink milk or any other liquid in a social gathering”
Difficulty speaking
Speech is one of the most problematic issues for these children. The speech problem is divided into two codes: difficulty saying certain words and hyper nasality during speech.
One of the participants expressed: “My child refuses to speak in front of others as they might not understand what he says”.
Another participant stated that: “Hyper nasality causes a continuous mocking on the part of his friends, which occurs mostly during communication”.
Dento-facial problems
From the point of view of the participants, dento-facial problems are one of the most frequent issues faced by these children and are categorized into two codes: missing teeth in the cleft area and dental crowding.
One of the participants said: “Missing two lateral incisors has had a negative effect on my child’s static beauty and she refuses to smile in any gathering.”
Another participant stated: “Dental crowding led to my child’s mocking by his peers.”
Insufficient socio-emotional well-being
Insufficient socio-emotional well-being was another major issue derived from our data. Based on the experiences and perceptions of our participants, their children lacked sufficient socio-emotional well-being in comparison to their peers. This could be described by four relevant sub-categories: shame, anxiety, insufficient peer interaction, and dissatisfaction with their own appearance.
Shame
Most of the participants agreed that apparent disfigurement is a reason for feeling ashamed. Signs are avoiding smiling or laughing with others and feeling shy or withdrawn:
One of the participants stated: “My child is always uncomfortable among her peers since she is afraid of their attitude toward her. She even resists to smile.”
Another participant said: “My daughter is always alone when we go to parties and does not speak with anyone.”
Anxiety
Anxiety one of the most common feelings among these children. They feel constant stress and pressure. This anxiety is defined as feeling worried or anxious about appearance, being worried about what other people think about them and being teased, bullied or called names by other children.
Disfiguration in facial appearance is one of the many distressing issues for these children. Even with multiple surgical revisions, they still see the differences between themselves and others. One of the participants mentioned: “Whenever my child goes to play with other children, since he is picked out by others, he becomes anxious and wants to leave immediately”.
According to the participants’ statements, what people think about children with CLP is one of their main concerns. The children feel anxious and uncomfortable since they feel it is due to their fault that they look like that. One of the participants expressed: “My daughter keeps asking me why do I look like this? What did I do to look like this?”.
As mentioned by most participants, being teased or called names by other children for the hyper nasality and inability to pronounce some words correctly or even their different facial appearance is one of the most common anxiety sources of these children. One of the participants stated: “My son is always upset and feels sad because his friends’ tease him and call him names, such as ugly boy”.
Insufficient peer interaction
Based on caregivers’ opinions, physical and facial deformity leads to lack of social interactions and thus, causes social isolation. Children suffering from this deformity have many problems in their social relations, which force them to abandon the relations. This concept is divided into some codes: being rejected by their peers and not willing to become acquainted with others.
Participants mentioned that the unwillingness of these children’s peers to accept their presence in a group leads to their being rejected by them. One of the participants said: “My son’s peers ignore him and do not permit him to play with the group.”
Based on the participants’ experience, social isolation and unwillingness to become acquainted with others is a significant problem. One of the participants expressed: “Wherever we go, my child hides himself and does not wish to talk or become acquainted with other children.”
Dissatisfaction with their own appearance
Most of the participants agree that their children are not satisfied with own appearances and mostly complain about it. They have wrong imagination about their appearances and always compare themselves with others. To some extent, this makes them depressed. This concept is divided into two codes: not willing to go to the kindergarten because of their appearance and not willing to play with peers because of their appearance.
According to the participants’ opinion, these children do not wish to go to kindergartens because of their appearance. They are ridiculed by their peers. One of the participants mentioned: “My son is afraid of being mocked and avoids going to kindergarten.”
Most of the participants believed that their children were not willing to play with their peers. Facial differences and linguistic difficulties cause them to be mocked by others; hence, they cannot develop good relationship with others. One of the participants said “Whenever my child seeks to play with his peers, his playmates escape.”
Discussion
The present study was carried out to explore QoL among young children with repaired CLP, based on their caregivers’ experiences. Results of the study revealed two main concepts including insufficient functional well-being and insufficient socio-emotional well-being. According to the study results, the first, and one of the most important problems, that affects these children’s QoL is insufficient functional well-being, which has been more explored with some related sub-categories including difficulty in eating, difficulty speaking and having dento-facial problems.
Difficulty in eating is one of their main problems. They have problems in incising fruits, such as apples and carrots, leading to dissatisfaction with the consumption of these types of fruit. Medium cooked meats are one of the essential foods which these affected children are denied due to the inability to chew comfortably. In addition, among the congenital deformities that most frequently influence the chewing function, the most prevalent is the CLP.20 Regurgitation of food and liquid from the nose was another disturbing event for a child and the caregivers, which might even induce the sense of suffocation. Some even refuse to take in liquids in front of their peers, due to fear of being mocked. Similarly, another study indicated that feeding and swallowing skills might be highly impaired in children with oral clefts. Feeding difficulty in cleft lip/palate children has been confirmed as a source of remarkable stress for parents.21
Another serious problem in these children is difficulty in speaking that could be described with hyper nasal and unintelligible voice, which invariably results in a fear of speaking and communicating. As vocal resonance is indispensible for the comprehensive rehabilitation of patients with CLP, its impairment contributes to social isolation.22 According to a study by Gkantidis et al, as reported by patients and their parents, speech problem was one of the key factors that decreased satisfaction and was correlated with the increased effect of the cleft in everyday life.23 Turner et al, also showed that most of the interviewed patients were teased about their speech problem.24 Furthermore, other studies have shown that speech and chewing difficulties, sometimes identified in cleft patients, might cause a significant cognitive sequel.22 Moreover, according to an investigation by de Buys Roessingh et al, the assessment of speech after palate surgery produced less than 50% of socially acceptable speech.25 Therefore, speech therapy is a common treatment required for CP patients. Lack of clarity in their speech might discourage them from having communication with others.
Dento-facial problems are the other problematic issue in these children. Alveolar clefts affect the number of teeth in the arch. One or more teeth might be missing in these children. These missing teeth and scars from the surgeries can result in the retardation of maxillary growth. Furthermore, due to previous surgeries and missing tooth, dental crowding is inevitable. Orthodontic treatment for these children is necessary prior to alveolar bone grafting. Another study indicated that missing teeth might influence both function and appearance.20 Similarly, Noar et al, disclosed that these patients were less satisfied with their profile, speech, and teeth.26
Insufficient socio-emotional well-being is the second major problem that affected QoL in these children. Based on the experiences of our participants, it was divided into four relevant sub-categories: shame, anxiety, insufficient peer interaction, and dissatisfaction with their own appearance.
Feeling ashamed is one of their most important problems. These children feel that they are picked out due to their different facial appearance. They also receive sympathy from others in their social interaction. Embarrassment might lead them to become uncomfortable when smiling in front of others since they feel that smiling might exaggerate their facial malformation. Furthermore, based on the participant experience, facial disfiguration leads to less interaction and feeling shy and withdrawn. Hence, they do not participate in group activities and cannot interact with others.
Feeling worried or anxious about appearance is the other problem. Disfiguration in facial appearance might even lead to interruption of social activities. It could lead to ways of avoiding situations. Being worried about what other people think about them and being teased, bullied or called names by other children are the other issues that make them anxious.
Similarly, another study revealed that, besides the functional aspect, socio-emotional factors play a key role in promoting QoL in these children.27 Several researches have reported psychological challenges among children, adolescents and young adults with oral clefts.28–30 In addition, these psychological problems could be interrelated. Anxiety and depression were reported about twice as often by subjects with CLP, as compared with controls. These psychological problems were highly related to concerns about appearance, dentition, speech, and desire for further treatment.31
According to another study, participants with CLP reported greater behavioral problems, such as being teased. Being teased was a significant predictor of poor psychological functioning amongst individuals with CLP.32 Gkantidis et al, highlighted the negative influence of the cleft on the patient’s activity and professional life during adulthood when poor esthetic results are more obvious.23 Likewise, another study found that CLP impacted emotional and social functioning.33 Another study showed that the affected adults report much more social anxiety than their unaffected siblings and controls.34 Children with oral clefts raised the rates of teacher-reported social problems, and anxious and withdrawn-depressed behavior. Also, direct observations and child representations revealed difficulties in their social relationships.35 Social-emotional deficits might become apparent in older school-age children, indicating the preschool and early elementary school years are an optimal time for preventive interventions.36 Castelnuovo-Tedesco stated that, providing hope could cause children to cope with anxieties “Children who think hopefully can imagine and embrace the goals relevant to the successful treatment of their physical problems”.37
These psychological difficulties are limited not only to children with cleft lip abnormality, but also to their parents. Research has shown that parents experience mental crisis, depending on their own previous background, while coping with present stress in raising a child with cleft lip.24
The children suffering from this deformity have many problems in their peer interaction and social relations, which force them to abandon them. Being rejected by their peers and not willing to become acquainted with others are sequels that these children faced. Similarly, according to another study, insufficient peer interaction was mainly accounted for in children with oral cleft problems.35 Evidence shows that miscommunication pertaining to the CLP are more significant during childhood.38 These disorders appear not to originate from phonological defects, but from psychological problems that might influence the entire development of an affected child.27 Additionally, another study indicated that peer interaction played a key role in maintaining psychosocial limitations. Numerous children with CLP might have less attractive facial appearance or speech than their peers. A high incidence of teasing over facial appearance was reported among those with CLP.26,32
Dissatisfaction with their own appearance is the other problem that these children faced. Similarly, according to the other studies, esthetics, and facial esthetics in particular, seem to be a crucial aspect of the individual’s general perception of life.39,40 Esthetic concerns appear to be a critical factor in influencing the health-related QoL for children with oral clefts. This factor appears to be more important as children reach adolescence (age 8–12 years) when acceptance by peers becomes more important.8 Furthermore, a negative response from outsiders, whether actual or perceived, might adversely affect the self-image.24 Certain self-report studies exhibit dissatisfaction with physical appearance in these children.32,41 Also, physical attractiveness plays a vital role in the development and maintenance of self-belief. Research indicates that preference for attractive individuals subsequently influences self-esteem, social competence, and future ratings of attractiveness.42
Moreover, being physically attractive appears to be an advantageous trait, regardless of age. It has been proven that physical attractiveness plays a significant role in social contexts like developing relationships during various stages of lifelike school, courtship, work and so forth. Social acceptance often depends on one’s physical appearance. These associations between physical beauty and social acceptability show the difficulties faced by CLP affected individuals.24 Patients should be advised to realize that other features of their personality are also significant in creating social encounters, establishing relationships, and securing employment.43
Conclusion
The present study has shed some light on the main problems influencing the QoL among children with oral clefts, even after the clefts were physically repaired. The most important problems derived from the participants’ experiences were insufficient functional well-being and insufficient socio-emotional well-being, both of which contributed to reduced QoL among these children. This study showed the importance of identifying the socio-emotional and functional outcomes in order to improve the QoL of these children. Our findings suggest that each step of the long-lasting and demanding treatment of an individual with a cleft might play a vital role in the functional and socio-emotional outcome and subsequently it might affect the everyday life of a person. Therefore, multidisciplinary interventional strategies, such as psychological aids are required to improve their diurnal life in every respect and should be considered from the early stages of treatment, or even early stages of diagnosis. And these supportive programs should be continued until a sufficient level of coping with daily conditions are achieved in later part of their lives.
Acknowledgments
This manuscript is based on MZ’s PhD thesis, registered in and financially supported by Shiraz University of Medical Sciences (# PhD 11604) and was conducted under supervision of AG and advisory of SA. The authors would like to thank all caregivers who participated in this study and spent their time to share their experiences through interviews. They have been well informed about the results of this study. The authors wish to thank Mr H Argasi at the Research Consultation Center (RCC) of Shiraz University of Medical Sciences for his invaluable assistance in editing this manuscript.
Disclosure
The authors report no conflicts of interest in this work.
References
Grad FP. The Preamble of the Constitution of the World Health Organization. Bull World Health Organ. 2002;80(12):981. | ||
Petersen PE, Bourgeois D, Ogawa H, Estupinan-Day S, Ndiaye C. The global burden of oral diseases and risks to oral health. Bull World Health Organ. 2005;83(9):661–669. | ||
Dyleski RA, Crockett DM, Seibert RW. Cleft lip and palate: evaluation and treatment of the primary deformity. In: Bailey BJ, Johnson JT, editors. Head and Neck Surgery—Otolaryngology. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2006:1317–1335. | ||
IPDTOC working group. Prevalence at birth of cleft lip with or without cleft palate: data from the International Perinatal Database of Typical Oral Clefts (IPDTOC). 2011;48(1):66–81. | ||
Khazaei S, Shirani AM, Khazaei M, Najafi F. Incidence of cleft lip and palate in Iran. A meta-analysis. Saudi Med J. 2011;32(4):390–393. | ||
Mitchell JC, Wood RJ. Management of cleft lip and palate in primary care. J Pediatr Health Care. 2000;14(1):13–19. | ||
Homer CJ, Kleinman LC, Goldman DA. Improving the quality of care for children in health systems. Health Serv Res. 1998;33(4 Pt 2):1091. | ||
Damiano PC, Tyler MC, Romitti PA, et al. Health-related quality of life among preadolescent children with oral clefts: the mother’s perspective. Pediatrics. 2007;120(2):e283–e290. | ||
Garratt AM, Ruta DA, Abdalla MI, Buckingham JK, Russell IT. The SF36 health survey questionnaire: an outcome measure suitable for routine use within the NHS? BMJ. 1993;306(6890):1440–1444. | ||
Allen PF, Mcmillan AS, Locker D. An assessment of sensitivity to change of the Oral Health Impact Profile in a clinical trial. Community Dent Oral Epidemiol. 2001;29(3):175–182. | ||
Hocevar-Boltezar I, Jarc A, Kozelj V. Ear, nose and voice problems in children with orofacial clefts. J Laryngol Otol. 2006;120(4):276–281. | ||
Marcusson A, Akerlind I, Paulin G. Quality of life in adults with repaired complete cleft lip and palate. Cleft Palate Craniofac J. 2001;38(4):379–385. | ||
Topolski TD, Edwards TC, Patrick DL. Quality of life: how do adolescents with facial differences compare with other adolescents? Cleft Palate Craniofac J. 2005;42(1):25–32. | ||
Strauss RP, Fenson C. Experiencing the “good life”: literary views of craniofacial conditions and quality of life. Cleft Palate Craniofac J. 2005;42(1):14–18. | ||
Locker D, Jokovic A, Tompson B. Health-related quality of life of children aged 11 to 14 years with orofacial conditions. Cleft Palate Craniofac J. 2005;42(3):260–266. | ||
Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today. 2004;24(2):105–112. | ||
Beck CT. Qualitative research: the evaluation of its credibility, fittingness, and auditability. West J Nurs Res. 1993;15(2):263–266. | ||
Lincoln YS. Emerging criteria for quality in qualitative and interpretive research. Qualitative Inquiry. 1995;1(3):275–289. | ||
Guba EG. Criteria for assessing the trustworthiness of naturalistic inquiries. Educational Technology Research and Development. 1981;29(2):75–91. | ||
Aizenbud D, Camasuvi S, Peled M, Brin I. Congenitally missing teeth in the Israeli cleft population. Cleft Palate Craniofac J. 2005;42(3):314–317. | ||
Miller C. Feeding issues and interventions in infants and children with clefts and craniofacial syndromes. Seminars in speech and language. Vol. 32: © Thieme Medical Publishers; 2011:115–126. | ||
Raposo-do-Amaral CE, Kuczynski E, Alonso N. Quality of life among children with cleft lips and palates: a critical review of measurement instruments. Revista Brasileira de Cirurgia Plástica. 2011;26(4):639–644. | ||
Gkantidis N, Papamanou DA, Karamolegkou M, Dorotheou D. Esthetic, functional, and everyday life assessment of individuals with cleft lip and/or palate. Biomed Res Int. 2015;2015:1–8. | ||
Turner SR, Thomas PW, Dowell T, Rumsey N, Sandy JR. Psychological outcomes amongst cleft patients and their families. Br J Plast Surg. 1997;50(1):1–9. | ||
de Buys Roessingh AS, Dolci M, Zbinden-Trichet C, Bossou R, Meyrat BJ, Hohlfeld J. Success and failure for children born with facial clefts in Africa: a 15-year follow-up. World J Surg. 2012;36(8):1963–1969. | ||
Noar JH. Questionnaire survey of attitudes and concerns of patients with cleft lip and palate and their parents. Cleft Palate Craniofac J. 1991;28(3):279–284. | ||
Rosanowski F, Eysholdt U. Phoniatric aspects in cleft lip patients. Facial Plast Surg. 2002;18(3):197–204. | ||
Hunt O, Burden D, Hepper P, Stevenson M, Johnston C. Self-reports of psychosocial functioning among children and young adults with cleft lip and palate. Cleft Palate Craniofac J. 2006;43(5):598–605. | ||
Brand S, Blechschmidt A, Müller A, et al. Psychosocial functioning and sleep patterns in children and adolescents with cleft lip and palate (CLP) compared with healthy controls. Cleft Palate Craniofac J. 2009;46(2):124–135. | ||
Kapp-Simon KA, Simon DJ, Kristovich S. Self-perception, social skills, adjustment, and inhibition in young adolescents with craniofacial anomalies. Cleft Palate Craniofac J. 1992;29(4):352–356. | ||
Ramstad T, Ottem E, Shaw WC. Psychosocial adjustment in Norwegian adults who had undergone standardised treatment of complete cleft lip and palate. II. Self-reported problems and concerns with appearance. Scand J Plast Reconstr Surg Hand Surg. 1995;29(4):329–336. | ||
Hunt O, Burden D, Hepper P, Johnston C. The psychosocial effects of cleft lip and palate: a systematic review. Eur J Orthod. 2005;27(3):274–285. | ||
Sinko K, Jagsch R, Prechtl V, Watzinger F, Hollmann K, Baumann A. Evaluation of esthetic, functional, and quality-of-life outcome in adult cleft lip and palate patients. Cleft Palate Craniofac J. 2005;42(4):355–361. | ||
Berk NW, Cooper ME, Liu YE, Marazita ML. Social anxiety in Chinese adults with oral-facial clefts. Cleft Palate Craniofac J. 2001;38(2):126–133. | ||
Murray L, Arteche A, Hill J, et al. The effect of cleft lip on socio-emotional functioning in school-aged children. J Child Psychol Psychiatry. 2010;51(1):94–103. | ||
Collett BR, Keich Cloonan Y, Speltz ML, Anderka M, Werler MM. Psychosocial functioning in children with and without orofacial clefts and their parents. Cleft Palate Craniofac J. 2012;49(4):397–405. | ||
Castelnuovo-Tedesco P. The psychological consequences of physical illness or defect and their relationship to the concept of deficit. Psychoanal Study Child. 1997;52(1):76–88. | ||
Neiman GS, Savage HE. Development of infants and toddlers with clefts from birth to three years of age. Cleft Palate Craniofac J. 1997;34(3):218–225. | ||
Jacobson A. Psychological aspects of dentofacial esthetics and orthognathic surgery. Angle Orthod. 1984;54(1):18–35. | ||
Harris DL, Carr AT. Prevalence of concern about physical appearance in the general population. Br J Plast Surg. 2001;54(3):223–226. | ||
Kapp K. Self concept of the cleft lip and or palate child. Cleft Palate J. 1979;16(2):171–176. | ||
Sarwer DB, Pruzinsky T, Cash TF, Goldwyn RM, Persing JA, Whitaker LA. Psychological Aspects of Reconstructive and Cosmetic Plastic Surgery: Clinical, Empirical, and Ethical Perspectives. Philadelphia, PA: Lippincott Williams & Wilkins; 2006. | ||
Cunningham SJ. The psychology of facial appearance. Dent Update. 1999;26(10):438–443. |
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
