Back to Journals » Patient Preference and Adherence » Volume 12
A qualitative study among breast cancer patients on chemotherapy: experiences and side-effects
Authors Nies YH , Mhd Ali A, Abdullah N, Islahudin F, Mohamed Shah N
Received 19 March 2018
Accepted for publication 16 June 2018
Published 28 September 2018 Volume 2018:12 Pages 1955—1964
DOI https://doi.org/10.2147/PPA.S168638
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Johnny Chen
Yong Hui Nies,1 Adliah Mhd Ali,1 Norlia Abdullah,2 Farida Islahudin,1 Noraida Mohamed Shah1
1Faculty of Pharmacy, Universiti Kebangsaan Malaysia, Kuala Lumpur, Malaysia; 2Department of Surgery, Universiti Kebangsaan Malaysia Medical Centre, Kuala Lumpur, Malaysia
Purpose: The objective of this study was to explore the experiences and side-effects of breast cancer patients on chemotherapy in Malaysia.
Participants and methods: Purposive sampling of 36 breast cancer patients who have completed chemotherapy and agreed to participate in semi-structured in-depth interviews. A constant comparative method and thematic analysis were used to analyze the interviews.
Results: Data were categorized into six main themes: know nothing of chemotherapy; fear of chemotherapy; patients’ beliefs in alternative treatments; symptom management; staying healthy after chemotherapy; and concerns of patients after chemotherapy.
Conclusion: Despite complaints about the bad experiences of their chemotherapy-induced side-effects, these patients still managed to complete the entire course of chemotherapy. Moreover, there is a need for a clinical pharmacy service in the oncology clinic setting in Malaysia in order to provide relevant information to help patients understand the chemotherapy received.
Keywords: breast cancer, chemotherapy, clinical pharmacy service, Malaysia, semi-structured interview
Introduction
Cancer is the main cause of death in both developed and developing countries. This problem is anticipated to grow globally because of the aging population, particularly in developing nations. Nowadays, unhealthy lifestyles such as smoking, unhealthy diet, sedentary behavior, as well as reproductive changes have exacerbated cancer risks. Therefore, breast cancer is still a worldwide issue, with an estimated 1.7 million new cases diagnosed annually. According to the Global Cancer Statistics, around 60% of deaths from cancer in developing countries were caused by breast cancer.1 In Malaysia, it is estimated that one in every 19 women is at risk for breast cancer, compared to one in every eight women in Europe and the US.2
Treatment for breast cancer comprises chemotherapy, hormonal therapy, targeted therapy, and palliative care.3 According to Corner and Bailey,4 the administration of chemotherapeutic drugs may cause numerous immediate side-effects to patients (eg, hypotension, facial and bodily flushing, and abnormal taste and smell) in the short-term (eg, nausea, vomiting, gastrointestinal disturbances, stomatitis) and long-term (eg, fatigue, alopecia, renal toxicity, sexual dysfunction). It would also influence food intake, by prompting several gastrointestinal symptoms such as nausea, vomiting, anorexia, abdominal pain, diarrhea, fever, stomatitis, and mucositis.5 Patients may restrict their food intake to minimize gastrointestinal symptoms, which may subsequently lead to nutrition deficiency.6 However, the type of chemotherapy used, dosage, as well as the treatment duration and frequency, would influence the seriousness of the side-effects experienced, which will eventually decrease the quality-of-life.
Most studies conducted focused on social support, body image, quality-of-life, and psychological reactions of patients with breast cancer.7 Due to the known various side-effects brought by chemotherapy, patients may have concerns and worries prior to receiving the treatment. Qualitative studies are carried out to explore the perceptions and sentiments of patients with breast cancer on chemotherapy, which allow researchers and healthcare providers to achieve a better understanding of patients’ feelings and unreported experiences. According to Beaver et al,8 in-depth qualitative interviews were conducted to explore the experiences of 20 women who had completed their neo-adjuvant chemotherapy for breast cancer in the North West of England. Besides that, Speck et al9 have also conducted semi-structured interviews on 25 patients to examine the experience and coping strategies for taste alteration in female breast cancer patients treated with docetaxel or paclitaxel in the US. Moreover, Kwok et al10 have also carried out interviews on 17 patients to explore the experiences, dietary information, and support needs of women who gain weight during chemotherapy treatment in Melbourne, Australia. Therefore, the semi-structured interview method was used in this study to explore the experiences and side-effects felt by patients with breast cancer after receiving chemotherapy.
Participants and methods
Study design and setting
In this study, a semi-structured interview method was used to determine patients’ personal experiences and the side-effects they felt undergoing chemotherapy. This design was chosen to comprehend the situation among Malaysian patients from patients’ personal experiences, besides capturing new insights and cultivating a deeper understanding of a particular phenomenon which would help the researchers in obtaining data on patients’ experiences that could not be captured through a quantitative study.11 The study was approved by the Research Ethics Committee of Universiti Kebangsaan Malaysia (Ref No: UKM PPI/111/8/JEP-2017–695), and it was carried out on patients from two tertiary care hospitals in Malaysia as well as the National Cancer Society Malaysia.
Participants
The patients were chosen from the three main ethnic groups in Malaysia, particularly the Malay, Chinese, and Indian. The purposive sampling method was employed to identify patients who fulfilled the criteria of the study in order to explore the voices of the patients within the study context.12 Breast cancer patients, regardless of the stage of their disease, who have completed their chemotherapy prior to the interview, were approached when they attended the clinic for a follow-up visit. The researcher recruited patients to participate in this study right after their consultation with the doctors. The purpose of this study was briefly explained to the patients. Written informed consent forms were distributed and collected from these patients upon their agreement to participate in the interview. The permission to audio-record the interview was also obtained from the patients prior to the interview.
Study tool
A semi-structured interview topic guide was utilized as a layout to investigate and probe further on issues with regard to the objectives of the study. The interview topic guide was developed based on the Ottawa Decision Support Framework (ODSF)13 and an extensive literature review, but patients were also allowed to raise any issues of concern. The main topics covered in the interview consist of: views on chemotherapy, experiences on chemotherapy, side-effects of chemotherapy, as well as the use of complementary and alternative medicines. The first draft of the interview topic guide was discussed among the researchers, and the modified interview topic guide was pre-tested by carrying out pilot interviews to ensure it was understandable and useful in retrieving the required information.
Interview
Interviews were conducted from October 2016 to January 2017. A list of topic guides was applied during the semi-structured interview in order to help the interviewer direct the conversation toward the topics and issues relevant to our research questions. However, patients did have the freedom to express their views in their own terms. The interviews were conducted until data reached saturation, where there was no new information contributed during the interview and no new codes could be produced.14 Glaser et al15 suggested the concept of saturation for accomplishing an appropriate sample size in qualitative studies. However, there were some other guidelines which recommended the sample size to range from 20 to 50.16,17 Each interview typically lasted between 15 and 30 minutes and was audio-recorded and transcribed verbatim for analysis.
Data analysis
The QSR NVivo® 11 software program was used to analyze the data. All transcribed data were analyzed using the constant comparative method with thematic analysis. A theme tends to depict the different highlights of an element over the dataset. A subtheme is categorized under the theme which has a similar concept with its parent theme, yet focuses on one remarkable concrete element. Basically, there is a four-phase process to develop a theme which includes initialization, construction, rectification, and finalization.18 The initialization phase involves reading the whole transcripts of patients, so that the researchers are able to understand the general information and also the main issues on the phenomenon under study. This phase involves creating codes and extracting relevant data throughout the entire dataset to identify important data corresponding to the research question. The construction phase involves sorting out codes and categorizing them into different clusters of codes relevant to the research question. Each cluster is given a label which covers similar codes. This phase involves combining the codes which have a similar concept to each other for development of potential themes. The rectification phase involves checking of the potential themes by the researchers through a discussion to ensure all the themes are convincing and answering the research question. The refinement of themes involves the themes being split, combined, or discarded. The finalization phase involves a comprehensive analysis of what the themes contribute to understanding the data, by focussing on each theme. This envelops a “story line” that gives a comprehensive view on the study phenomenon. At the end, discussion and finalization of an appropriate informative name for each theme was carried out and agreed by all researchers.18
Results
Patients’ characteristics
A total of 36 patients aged between 34–71 years with breast cancer who had completed chemotherapy participated in the study. The ethnic distribution consisted of 66.7% Malays; 25% Chinese; and 8.3% Indians. The majority of the patients (44.4%) had Stage II breast cancer. The breast cancer patients are described in Table 1. The most common chemotherapy-induced side-effects encountered in this study were hair loss (66.7%), cracked lip/dry mouth (61.1%), and vomiting (58.3%). The symptoms experienced after chemotherapy are summarized in Table 2.
  | Table 1 Description of the breast cancer patients from qualitative interview |
  | Table 2 Systematic symptoms/signs during chemotherapy (not exclusive) |
Key themes
During the analysis, six themes were identified: know nothing of chemotherapy; fear of chemotherapy; patients’ belief in alternative treatments; symptom management; staying healthy after chemotherapy; and concerns of patients after chemotherapy. The number of patients who expressed a given theme and subtheme are shown in Tables 3 and 4, respectively.
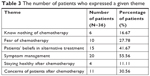  | Table 3 The number of patients who expressed a given theme |
  | Table 4 The number of patients who expressed a given subtheme |
Theme 1: Know nothing of chemotherapy
Lack of prior knowledge about chemotherapy
A few patients reported that they did not understand much about chemotherapy. They did not know how chemotherapy is administered and the feeling when chemotherapy is administered. However, they hoped that the treatment could cure their cancer.
I have never received it beforehand. So, during the first time, I just knew what chemotherapy is as I always heard of it but I didn’t have any idea about it. (IV003, Malay, 50 years, Stage IV)
I didn’t know anything before about chemotherapy … Many of them thought that they would feel the pain while receiving the chemotherapy … because we (patients’ family) do not have any idea about chemotherapy. (IV007, Malay, 51 years, Stage III)
As the doctor said it is used to shrink the tumor … I felt sorry lah because I didn’t really understand … it’s our body, so we (I) didn’t know what it does to our body then. I just prayed and hoped that the tumor could be decreased in size. (IV036, Malay, 34 years, Stage III)
Theme 2: Fear of chemotherapy
The consequences after receiving chemotherapy
The majority of the patients reported that they were worried about the side-effects of chemotherapy, so they needed courage to face the treatment. Moreover, some of them had even heard that chemotherapy could be fatal, causing them to be afraid of chemotherapy.
We (patients’ family) struggled to receive it at first since we (patients’ family) have heard a lot about the side-effects such as some people would not be able to stand [side-effects] after chemotherapy, so I was worried. (IV004, Chinese, 62 years, Stage I)
I cried lah because I was worried. People said that most of the patients will die after getting cancer, so I cried because I was afraid. (IV012, Malay, 68 years, Stage II)
Of course, I afraid because everyone said that the chemotherapy is like killing yourself slowly. That’s what people said lah, because of those drugs. (IV016, Malay, 37 years, Stage IV)
I was afraid of it because I had not undergone it before. Since I have heard from others about the side-effects, it’s so scary when you knew that you’re going to feel it later. (IV018, Chinese, 51 years, Stage III)
Fear of hospitalization
Despite advances in medical technology, some patients still fear hospital treatments. This has led them to try alternative medicines as they did not want to be admitted to the hospital.
The fear of handling the disease in the hospital causes us to try alternative treatments before heading to the hospital as the last option for survival. (IV002, Malay, 60 years, Stage III)
Theme 3: Patients’ beliefs in alternative treatments
Concurrent use of complementary and alternative medicines with chemotherapy
A few patients reported using complementary medicines in addition to chemotherapy. This included the use of fruits and tea, together with chemotherapy. They claimed that they felt better after consuming them and had fewer side-effects from chemotherapy.
I have been eating the “XX” brand, especially for cancer … It provides energy and strength … So, I tried it out, and it really made me feel energized. And this shows that XX works for my body. I used to eat it during the time I received the chemotherapy, and that’s why I suffered less from the side-effects because I felt energized when taking XX. (IV001, Malay, 47 years, Stage IV)
Arr … I did drink the warm lemon water … I just googled [the information] myself … I felt a bit fresh … I felt fresh when drinking the lemon water because of the flavor, so I could feel less pain in my body. (IV015, Malay, 34 years, Stage III)
I did drink the butterfly tea because they said it’s good. After the chemotherapy, I could feel a little bit of pain inside my body, but after I drank it, I felt good and didn’t feel the pain like before. Even until now, I feel fresh and healthy … Maybe it suits my body. At least I feel okay until now. (IV017, Malay, 49 years, Stage II)
Patients’ perception towards the impact of complementary and alternative medicines on cancer.
There were patients who claimed tumor shrinkage after using alternative medicines given by friends before any conventional treatment was started.
I just ate the sour sop. They said it is for cancer. When I ate the sour sop, the doctor in hospital X measured the size of my cancer, and it was 9 cm. Then I went to hospital Y, and when the doctor measured it, it was 7 cm, even though I hadn’t started the chemotherapy. So, the sour sop is okay lah … (IV010, Malay, 46 years, Stage IV)
… her tumour was 6 cm, and the doctor insisted on an operation, but she kept having the “YY” for around 1 month. After that, she went back for her check up again, and it turned out to be 3 cm. Though the doctor wanted to operate at first, she held it back for about 1 month. In the end, the doctor couldn’t find the tumor anymore as it was getting smaller and smaller and it was broken into smaller pieces, she really drank a lot of YY. (IV028, Malay, 38 years, Stage III)
Another patient reported that there was a center offering ozone treatment that claimed “to destroy foreign microbes for treatment of various diseases.” The patient claimed that it was useful for “body detoxification.”
I did the ozone [treatment] to clean up and bring more oxygen into my body. All that … I think that I feel fresher, better. I think for the cancer, it should undergo alternative ozone because I can see myself my blood is black in color … after chemotherapy … it’s full of … what is it called? The dirty chemical all that, isn’t it? So, it’s black color. When I put ozone, I can see the blood changed color … (IV024, Malay, 55 years, Stage II)
Theme 4: Symptom management
Quarantined themselves and tolerated the side-effects passively
The emotional status of a few patients was impaired. They were in awful temperament when experiencing the side-effects and discomfort. One of the patients reported that she quarantined herself in the room in order to prevent herself from hurting others. Meanwhile, some of them tolerated the discomfort passively.
I informed every one of my family members, and all my children. Erm … I like to be independent, so leave me alone, and I stayed in one room, and I didn’t want to have any visitors so that, I could handle my emotions alone, and nobody would get hurt. (IV002, Malay, 60 years, Stage III)
I didn’t have any choice, I just went through it day by day. I’m always thinking when will it end? (IV016, Malay, 37 years, Stage IV)
Solutions to counter appetite problems
Most of the patients reported that they experienced significant impairment in their daily life. The side-effects from chemotherapy had affected their quality-of-life. One of the most common problems encountered by them was having no appetite to eat, because everything felt tasteless, and they also feel nauseous. The patients thought that ample nutrition is necessary to survive chemotherapy.
But I just ate even though it felt tasteless … (IV005, Malay, 56 years, Stage III)
Force to eat (laughing). If not, I would not have any energy later. (IV007, Malay, 51 years, Stage III)
I have to eat anyhow even though it means pouring some water into the rice, as long as I have it in order to make me feel full. (IV012, Malay, 68 years, Stage II)
I still forced myself to eat even though the food was vomited out after eating; as long as I ate something … (IV014, Chinese, 52 years, Stage III)
Lifestyle adjustments
The patients expressed that being active by doing household chores distracted them from thinking about the disease. They would also psychologically think of themselves as healthy individuals rather than cancer patients.
Since we (I) felt that we (I) were (was) sick, we (I) kept lying down, and this would make us (me) sicker if we (I) kept laying down. So, I tried to make myself active by doing some household chores. We (I) couldn’t keep laying down like that. (IV017, Malay, 49 years, Stage II)
Encountering the impact of chemotherapy positively
A few patients were actively coping with the side-effects during this transitional period in their life to reduce the degree of suffering. They knew that they would encounter the side-effects after the chemotherapy, so they tried certain things in order to counteract them.
I did drink a lot of water as I didn’t want to have any stomach ulcer or gastritis, so I took good care of myself. I drank the water, and I finished drinking one jar of water in just five intakes (laughing). I didn’t want the pain at all … I ate the medicine. But they just gave the medicine for 3 days, so I would feel the pain after that. They did give the medicine, but there were a lot of medicines that I had to eat. (IV028, Malay, 38 years, Stage III)
I think positively lah … like … when I was feeling pain and all that. I would … if I didn’t eat, look lethargic … and that’s not good for me. (IV036, Malay, 34 years, Stage III)
Theme 5: Staying healthy after chemotherapy
Avoid the crowd to prevent infection
A few patients actively engaged in self-care by deliberately staying away from crowds, because they were informed that their immune system had been weakened after chemotherapy. The patients also noticed that they fell sick easily when people around them were unwell. Therefore, they preferred to stay at home to prevent themselves from getting any infections.
I took all the doctor’s advice that I should avoid those who are sick, especially those with cough and flu, since I didn’t have my antibody. I noticed that I fell sick easily with cough and flu when my grandchildren were sick as we (patients’ family) were living in the same house. So, I would abstain from kissing and touching my grandchildren. (IV002, Malay, 60 years, Stage III)
Since I started chemotherapy, I had to prevent myself from being attacked by bacteria. So, I quarantined myself and avoided socializing with others when I was receiving my chemotherapy. That was the way I took care of myself by staying home … (IV003, Malay, 50 years, Stage IV)
Although my side-effects were not serious, we needed to take good care [of ourselves] by staying at home so that I won’t be affected by the crowd outside. (IV008, Malay, 47 years, Stage II)
Theme 6: Concerns of patients after chemotherapy
Worrying about the possibility of recurrence in future
The patients were found to be worried about their future health due to the possibility of cancer recurrence. They felt that cancer recurrence was quite common, even in those who had completed their treatment. Therefore, they understood that cancer may recur despite the chemotherapy received.
Of course yes. I think every patient will worry about it because it is not guaranteed that you will fully recover. Even the doctor would not be able predict when the cancer will come back again. (IV018, Chinese, 51 years, Stage III)
Yup … nowadays recurrence is so common, so many people got it. That’s why it is so scary. If it recurred, one has to do again the chemo, radio … (IV019, Indian, 59 years, Stage III)
Yes, since I have heard from my friends that it [cancer] could recur. (IV020, Malay, 65 years, Stage II)
Discussion
Currently, chemotherapy remains a vital part of the treatment for breast cancer patients with both early and advanced cancer stages. There are many chemotherapy regimens available for patients with breast cancer nowadays; however, every single regimen differs in terms of its constituent agents, route of administration, frequency, effectiveness, and side-effects.19 Due to the increasing importance of patients’ quality-of-life, it is essential for doctors to understand patients’ unreported experiences while they are on chemotherapy, as incidences of chemotherapy-induced side-effects are actually higher than what have been reported.20 The use of chemotherapy has influenced each patient in different ways and at different degrees. Some patients reported experiencing severe side-effects; however, there were also those who reported minimal side-effects from chemotherapy.21 The present study found that the majority of the patients interviewed were psychologically distressed due to the side-effects, and only a few patients managed to cope with the side-effects experienced. Nonetheless, all patients completed the entire course of treatment, as they were encouraged to complete the entire course of chemotherapy recommended despite the side-effects experienced. They could inform their oncologists and discuss how to deal with those unwanted side-effects to prevent them from withdrawing chemotherapy midway.21
In this study, patients’ comprehension of chemotherapy was rather limited; hence, there is room for improvement to meet the particular needs of this population. Moreover, many patients expressed their fear towards chemotherapy regardless of their disease stage. This study also found that some patients may not like to seek treatment at hospitals due to the fear of hospitalization. Lim et al22 reported that the loneliness of not having family members around them when they are admitted is one of the reasons for resisting treatment at the hospital. In addition, patients’ perceptions of chemotherapy-induced side-effects could also make them feel uneasy, since they had heard others describing the negative side-effects which had indirectly traumatized them.
A number of government hospitals in Malaysia have clinical pharmacists at oncology wards or clinics. However, in one of our hospital settings there is no clinical pharmacist stationed at the oncology clinics. Therefore, oncologists have to explain about chemotherapy during patient consultation, which may not be comprehensive, due to the short consultation period in a busy clinic. The presence of oncology clinical pharmacy services is crucial, as clinical pharmacists could support patient management by providing specific medication information, drug-use review, counseling, as well as the management of treatment-related side-effects.23 Crespo and Tyszka24 reported that the provision of clinical pharmacy services in ambulatory chemotherapy units is able to improve patients’ understanding of the medication taken, enhance patients’ satisfaction, and improve self-management of treatment-related side-effects.
It is also essential to educate patients with accurate information in order to let them understand all the misunderstandings (such as chemotherapy could cause death) as described by patients in the present study. Therefore, provision of adequate information on chemotherapy prior to its administration, including its side-effects and self-care strategies, are necessary in order to manage treatment-related concerns as well as physical and psychosocial outcomes.25 Studies have shown that information given to patients allows them to comprehend their diagnoses and promotes participation of patients in treatment decision-making.8,26 Information provided also allows patients to have a feeling of control over their circumstances, while at the same time alleviating tension, changing their mind-set, and improving their ability to cope with the situation better in the future.27 An open discussion may help to prevent unwanted strain between physicians and patients before making treatment decisions, and this could also build a better physician–patient relationship in the long run.
Hair loss, cracked lips/dry mouth, and vomiting were the top three side-effects experienced by patients receiving chemotherapy in the present study. This is similar to the study by Chan and Ismail,28 where more than half of the patients experienced hair loss after chemotherapy. Despite the fact that their hair will grow again after the completion of chemotherapy, many patients still feel distressed, as they think that it represents a sign of cancer patient on chemotherapy. In addition, chemotherapy-induced vomiting has been ranked as one of the most distressing side-effects according to several studies.29–31 Unsurprisingly, the majority of the patients in this study reported that vomiting was one of the most worrisome side-effects because it had drastically influenced their eating appetite.
In this study, there were about 40% of patients who believed in complementary and alternative medicines (CAM). There were two patients under theme 1 (know nothing of chemotherapy) exploring CAM, meanwhile there were six patients under theme 2 (fear of chemotherapy) seeking CAM while on chemotherapy. The utilization of CAM has turned out to be progressively well known, especially among patients with cancer.32,33 CAM use has been reported to be prevalent among patients with breast cancer in Malaysia who have a higher education level,34 higher household income, advanced cancer, as well as lower chemotherapy schedule compliance according to Chui et al.35 However, education and income level of patients were not determined in this study.
In this study, there were two censored brand names (which appear in the first and second subthemes under theme 3), which have been differentiated as brand XX and YY. Both brands are different kinds of herbal supplements used by patients in this study. They claimed that the supplements were useful to provide relief from chemotherapy-induced side-effects. Studies have reported that cancer patients would seek CAM to lessen unbearable side-effects, strengthen their immune system, as well as improve physical and spiritual well-being.36,37 In the present study, there was a patient who reported feeling better with less chemotherapy-induced side-effects after receiving ozone therapy from a center outside the hospital. However, there is not enough evidence in the literature to support its use for cancer patients. The majority of patients with breast cancer tend to use CAM without informing their physicians. Patients should inform their physicians and seek proper guidance on the advantages and disadvantages of CAM, because its usage is not usually addressed in clinical consultations.38,39 The present study reported that patients claimed that CAM had improved their health and lessened the side-effects of chemotherapy. Previous studies have also reported that CAM with a diet rich in fruits and vegetables and low in fat has shown a significant improvement in the overall quality-of-life and better ability to cope with their disease among patients with gynecologic and breast malignancies.40,41
Some patients were mindful of their health while receiving chemotherapy, as they knew that their immune system had weakened. Therefore, they kept themselves away from the crowd by staying at home to avoid falling sick, which may intensify the severity of the side-effects experienced. In this study, the majority of the patients with advanced cancer stages thought their future as being uncertain because they did not know whether their cancer would return in the future. Beatty et al40 also revealed that patients with breast cancer suffered from the feeling of ongoing fear of recurrence due to the possibility of dying, even though they have completed their treatment. The fear of recurrence is exclusively related to the possibility of death and also the acceptance of receiving chemotherapy again in the future. A few regional slangs such as “lah” appeared in the context of the patients’ interview. “Lah” is a slang used mainly by people of South-East Asia (mainly in Malaysia and Singapore) to complement sentences in a social conversation. It is a final “word” indicating an imperative, reassurance, or emphasis.
There are few limitations in the present study. Patients who were willing to participate in this study were more open to express their feelings and experiences while on chemotherapy. Those who refused may have other views on the side-effects experienced from the administration of chemotherapy. Similarly, those who are skeptical or fearful of chemotherapy and discontinued chemotherapy earlier were not available for interview. These patients may have different views on chemotherapy compared to patients who completed chemotherapy. Nonetheless, the qualitative semi-structured interviews conducted were able to capture various patients’ experiences and side-effects related to the use of chemotherapy for breast cancer.
Conclusion
Most patients experienced side-effects from chemotherapy; however, they completed the entire course of chemotherapy successfully. Findings from the present study have also shed light on information and support needed by patients with breast cancer before receiving chemotherapy. It is important to provide more detailed information to patients about chemotherapy, along with potential side-effects prior to its commencement. Therefore, patients are better informed and understand the treatment that they are about to receive and are able to address any misconceptions about chemotherapy. Besides that, clinical pharmacists would be in an ideal position to counsel patients on the administration of chemotherapy, expected side-effects, and its management.
Acknowledgments
We would like to thank all the participants, staff nurses, and administrative personnel of the participating hospitals and the National Cancer Society Malaysia for assisting in the study. We would also like to thank Universiti Kebangsaan Malaysia for funding this research (grant code: KOMUNITI-2014-009).
Disclosure
The authors report no conflicts of interest in this work.
References
Torre LA, Bray F, Siegel RL, et al. Global cancer statistics, 2012. CA Cancer J Clin. 2015;65(2):87–108. | ||
Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61(2):69–90. | ||
Phua CE, Tang WH, Yusof MM, et al. Risk of Treatment Related Death and Febrile Neutropaenia with First Line Palliative Chemotherapy for De Novo Metastatic Breast Cancer in Clinical Practice in a Middle Resource Country. Asian Pacific Journal of Cancer Prevention. 2015;15(23):10263–10266. | ||
Corner J, Bailey CD. Cancer nursing: care in context. 2nd ed. Oxford: John Wiley & Sons; 2009. | ||
Capra S, Ferguson M, Ried K. Cancer: impact of nutrition intervention outcome – nutrition issues for patients. Nutrition. 2001;17(9):769–772. | ||
Lua PL, Salihah NZ, Mazlan N. Nutritional status and health-related quality of life of breast cancer patients on chemotherapy. Malays J Nutr. 2012;18(2):173–184. | ||
Sammarco A, Konecny LM. Quality of life, social support, and uncertainty among Latina and Caucasian breast cancer survivors: a comparative study. Oncol Nurs Forum. 2010;37(1):93–99. | ||
Beaver K, Williamson S, Briggs J. Exploring patient experiences of neo-adjuvant chemotherapy for breast cancer. Eur J Oncol Nurs. 2016;20:77–86. | ||
Speck RM, Demichele A, Farrar JT, et al. Taste alteration in breast cancer patients treated with taxane chemotherapy: experience, effect, and coping strategies. Support Care Cancer. 2013;21(2):549–555. | ||
Kwok A, Palermo C, Boltong A. Dietary experiences and support needs of women who gain weight following chemotherapy for breast cancer. Support Care Cancer. 2015;23(6):1561–1568. | ||
Sutton J, Austin Z. Qualitative Research: Data Collection, Analysis, and Management. Can J Hosp Pharm. 2015;68(3):226–231. | ||
Pathmawathi S, Beng TS, Li LM, et al. Satisfaction with and Perception of Pain Management among Palliative Patients with Breakthrough Pain: A Qualitative Study. Pain Manag Nurs. 2015;16(4):552–560. | ||
Légaré F, O’Connor AM, Graham ID, et al. Primary health care professionals’ views on barriers and facilitators to the implementation of the Ottawa Decision Support Framework in practice. Patient Educ Couns. 2006;63(3):380–390. | ||
Guest G, Bunce A, Johnson L. How many interviews are enough? An experiment with data saturation and variability. Field methods. 2006;18(1):59–82. | ||
Glaser BG, Strauss AL, Strutzel E. The Discovery of Grounded Theory; Strategies for Qualitative Research. Nurs Res. 1968;17(4):364. | ||
Creswell JW. Quality inquiry and research design: Choosing among five traditions. California: Thousand Oaks; 1998. | ||
Morse JM. Designing funded qualitative research. Handbook of qualitative research. 2nd ed Denizin NK, Lincoln YS, editors. California: Thousand Oaks; 1994. | ||
Vaismoradi M, Jones J, Turunen H, Snelgrove S. Theme development in qualitative content analysis and thematic analysis. J Nurs Educ Pract. 2016;6(5):100. | ||
Beusterien K, Grinspan J, Kuchuk I, et al. Use of conjoint analysis to assess breast cancer patient preferences for chemotherapy side effects. Oncologist. 2014;19(2):127–134. | ||
Maryann N. Center for Medical Consumers. Breast Cancer Chemotherapy: Adverse Effects Higher Than Reported in Clinical Trials. HEALTHFACTS. 2006;4. Available from: http://www.encognitive.com/files/Breast%20Cancer%20Chemotherapy--Adverse%20side%20effects.pdf. Accessed February 22, 2018. | ||
Lai XB, Ching SSY, Wong FKY. A qualitative exploration of the experiences of patients with breast cancer receiving outpatient-based chemotherapy. J Adv Nurs. 2017;73(10):2339–2350. | ||
Lim JN, Potrata B, Simonella L, et al. Barriers to early presentation of self-discovered breast cancer in Singapore and Malaysia: a qualitative multicentre study. BMJ Open. 2015;5(12):e009863. | ||
Leveque D, Delpeuch A, Gourieux B. New anticancer agents: role of clinical pharmacy services. Anticancer Res. 2014;34(4):1573–1578. | ||
Crespo A, Tyszka M. Evaluating the patient-perceived impact of clinical pharmacy services and proactive follow-up care in an ambulatory chemotherapy unit. J Oncol Pharm Pract. 2017;23(4):243–248. | ||
Aranda S, Jefford M, Yates P, et al. Impact of a novel nurse-led prechemotherapy education intervention (ChemoEd) on patient distress, symptom burden, and treatment-related information and support needs: results from a randomised, controlled trial. Ann Oncol. 2012;23(1):222–231. | ||
McWilliam CL, Brown JB, Stewart M. Breast cancer patients’ experiences of patient-doctor communication: a working relationship. Patient Educ Couns. 2000;39(2–3):191–204. | ||
Henman MJ, Butow PN, Brown RF, Boyle F, Tattersall MH. Lay constructions of decision-making in cancer. Psychooncology. 2002;11(4):295–306. | ||
Chan HK, Ismail S. Side effects of chemotherapy among cancer patients in a Malaysian General Hospital: experiences, perceptions and informational needs from clinical pharmacists. Asian Pac J Cancer Prev. 2014;15(13):5305–5309. | ||
Schnell FM. Chemotherapy-induced nausea and vomiting: the importance of acute antiemetic control. Oncologist. 2003;8(2):187–198. | ||
Sun CC, Bodurka DC, Weaver CB, et al. Rankings and symptom assessments of side effects from chemotherapy: insights from experienced patients with ovarian cancer. Support Care Cancer. 2005;13(4):219–227. | ||
Farrell C, Brearley SG, Pilling M, Molassiotis A. The impact of chemotherapy-related nausea on patients’ nutritional status, psychological distress and quality of life. Support Care Cancer. 2013;21(1):59–66. | ||
Ernst E, Cassileth BR. The prevalence of complementary/alternative medicine in cancer: a systematic review. Cancer. 1998;83(4):777–782. | ||
Molassiotis A, Fernadez-Ortega P, Pud D, et al. Use of complementary and alternative medicine in cancer patients: a European survey. Ann Oncol. 2005;16(4):655–663. | ||
Üstündağ S, Demir Zencirci A, Zencirci AD. Complementary and alternative medicine use among cancer patients and determination of affecting factors: a questionnaire study. Holist Nurs Pract. 2015;29(6):357–369. | ||
Chui PL, Abdullah KL, Wong LP, Taib NA. Prayer-for-health and complementary alternative medicine use among Malaysian breast cancer patients during chemotherapy. BMC Complement Altern Med. 2014;14(1):425. | ||
Hlubocky FJ, Ratain MJ, Wen M, Daugherty CK. Complementary and alternative medicine among advanced cancer patients enrolled on phase I trials: a study of prognosis, quality of life, and preferences for decision making. J Clin Oncol. 2007;25(5):548–554. | ||
Nazik E, Nazik H, Api M, Kale A, Aksu M. Complementary and alternative medicine use by gynecologic oncology patients in Turkey. Asian Pac J Cancer Prev. 2012;13(1):21–25. | ||
Tautz E, Momm F, Hasenburg A, Guethlin C. Use of complementary and alternative medicine in breast cancer patients and their experiences: a cross-sectional study. Eur J Cancer. 2012;48(17):3133–3139. | ||
Pirri C. Complementary and alternative medicine used by patients with cancer: evidence for efficacy and safety. Perspectives On Complementary And Alternative Medicines. I Olver, M Robotin, editors. London: Imperial College Press; 2012:31–87. | ||
Beatty L, Oxlad M, Koczwara B, Wade TD. The psychosocial concerns and needs of women recently diagnosed with breast cancer: a qualitative study of patient, nurse and volunteer perspectives. Health Expect. 2008;11(4):331–342. | ||
Fasching PA, Thiel F, Nicolaisen-Murmann K, et al. Association of complementary methods with quality of life and life satisfaction in patients with gynecologic and breast malignancies. Support Care Cancer. 2007;15(11):1277–1284. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
