Back to Journals » Drug Design, Development and Therapy » Volume 17
A Novel Opioid-Sparing Analgesia Following Thoracoscopic Surgery: A Non-Inferiority Trial
Authors Sun JJ, Xiang XB, Xu GH, Cheng XQ
Received 30 January 2023
Accepted for publication 19 May 2023
Published 6 June 2023 Volume 2023:17 Pages 1641—1650
DOI https://doi.org/10.2147/DDDT.S405990
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Tin Wui Wong
Jing-jing Sun,1,* Xiao-bing Xiang,2,* Guang-hong Xu,1 Xin-qi Cheng1
1Department of Anesthesiology, The First Affiliated Hospital of Anhui Medical University, Hefei, People’s Republic of China; 2Department of Anesthesiology, The Cancer Hospital of the University of Chinese Academy of Sciences (Zhejiang Cancer Hospital), Hefei, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Xin-qi Cheng; Guang-hong Xu, Department of Anesthesiology, The First Affiliated Hospital of Anhui Medical University, 218 Jixi Road, Hefei, Anhui, 230022, People’s Republic of China, Tel +86-0551-62922344, Fax +86 0551 62923704, Email [email protected]; [email protected]
Purpose: This randomized, non-inferiority study aimed to observe the feasibility of opioid-sparing analgesia based on modified intercostal nerve block (MINB) following thoracoscopic surgery.
Patients and Methods: 60 patients scheduled for single-port thoracoscopic lobectomy were randomized to the intervention group or control group. After MINB was performed in both groups at the end of the surgery, the intervention group received patient controlled-intravenous analgesia (PCIA) of dexmedetomidine 0.05 μg/kg/h for 72 h after surgery, and the control group received conventional PCIA of sufentanil 3 μg/kg for 72 h. The primary outcome was a visual analog scale (VAS) on coughing 24 h after surgery. Secondary outcomes included the time to first analgesic request, pressing times of PCIA, time to first flatus, and hospital stay.
Results: There was no difference in the cough-VAS at 24 h (median [interquartile range]) between the intervention group [3 (2– 4)] and control group [3 (2– 4), P = 0.36]. The median difference (95% CI) in the cough-VAS at 24 h was [0 (0 to 1), P = 0.36]. There was no significant difference in the time to first analgesic request, pressing times of PCIA, and hospital stay between groups (P > 0.05). A significant decrease in time to first flatus was observed in the intervention group (P < 0.01).
Conclusion: Opioid-sparing analgesia provided safe and analogous postoperative analgesia with a shortened time to first flatus, compared with sufentanil-based analgesia in thoracoscopic surgery. This might be a novel method recommended for thoracoscopic surgery.
Keywords: opioid-sparing, intercostal nerve block, dexmedetomidine, sufentanil, opioid consumption, thoracoscopic surgery
Graphical Abstract:
Plain Language Summary
Opioids are no stranger to the public. Opioids have strong analgesic properties, and can greatly reduce pain after surgery. Currently, opioids and other drugs combined with nerve block are often used in analgesia after thoracic surgery. However, opioids can prolong the time to first flatus, bowel movements, and even hospital stay time after surgery. So, we aimed to find a new method of pain control that would have the same analgesic effects as the previous method (opioid-based analgesia) and dramatically reduce opioid use. Dexmedetomidine and nonsteroidal anti-inflammatory drugs (NSAIDs), as non-opioid analgesics, have good postoperative analgesic effect and reduce opioid consumption. Based on the above, we proposed a novel analgesia strategy that combined with nerve block and dexmedetomidine, as well as NSAIDs. Then, we designed and conducted experiments related to patients undergoing thoracoscopic surgery comparing two analgesic strategies. The results show that the novel analgesia strategy provided safe and analogous postoperative analgesia and shortened the time to first flatus. Therefore, we believe the novel analgesia strategy that combined with nerve block and dexmedetomidine, as well as NSAIDs, may be an effective alternative for thoracoscopic surgery.
Introduction
Spurred by concerns about undesirable side effects1 following opioid-based analgesia, strategies for opioid-sparing analgesia are now recommended for single-port video-assisted thoracoscopic surgery (VATS). Multimodal analgesia based on regional techniques can be used to markedly reduce perioperative opioid consumption.2 However, little is known about its potentially facilitating enhanced recovery effect. Recently, our preliminary observation found that multimodal analgesia based on modified intercostal nerve block (MINB)3 was a novel method to achieve an opioid-sparing effect perioperatively in a minimally invasive lobectomy. It would be interesting to investigate whether multimodal strategies based on MINB could potentially facilitate enhanced recovery.
Dexmedetomidine (DEX) and NSAIDs were recommended for postoperative analgesia to reduce opioid consumption.4,5 The whole-course application of DEX combined with ketorolac6 has been demonstrated to provide adequate and safe postoperative intravenous patient-controlled analgesia (PCIA) following thoracoscopic surgery. Based on the above, a novel opioid-sparing analgesia that combined with MINB and dexmedetomidine, as well as NSAIDs, was proposed.
Aim
This randomized, controlled and non-inferiority trial would evaluate the feasibility of a new opioid-sparing protocol after VATS, which was compared to the conventional opioid-based analgesia model.
Methods
Design and Participants
This prospective trial was approved by the institutional review board of the First Affiliated Hospital of Anhui Medical University (approval No. PJ2020-01-27) and written informed consent was obtained from the participants. The trial was carried out in accordance with the Declaration of Helsinki. We successfully registered at http://www.chictr.org.cn (ChiCTR2000031906) on 14 April 2020. Patients with American Society of Anesthesiologists (ASA) physical status classes I–III, aged 18–70 years and scheduled for single-port VATS between April 15, 2020 and March 31, 2021 were enrolled. The exclusion criteria were as follows: any difficulty with communication, any contraindications to regional techniques (allergy to local anesthetics, infection around the site of the block, and coagulation disorder), history of an opioid use disorder, heart rate < 50 beats/minute or II–III atrioventricular block, previous history of a gastrointestinal ulcer or platelet abnormality, allergy to the study drugs, and refusal to participate in the study. Those who were transferred to thoracotomy and discontinued the use of analgesia pumps for various reasons were subsequently excluded from the study.
Randomization and Masking
All recruited patients based on computer-generated random assignment were randomly assigned (1:1) to the intervention group (a combination of MINB and PCIA of dexmedetomidine 0.05 µg/kg/h for 72 h postoperatively) and the control group (a combination of MINB and PCIA of sufentanil 3 µg/kg for 72 h postoperatively). Patients and observers were blinded to the treatment allocation.
Anesthesia Management
After entering the operating room, routine monitoring was performed: invasive arterial blood pressure, electrocardiogram (ECG), and pulse oxygen saturation. The depth of sedation was monitored by a SedLine monitor (Masimo Inc, Irvine, CA, USA). Anesthesia was induced with etomidate 0.3 mg/kg, sufentanil 0.3–0.5 µg/kg, and cisatracurium 0.2–0.3 mg/kg. Then, the surgeon started the operation. General anesthesia was maintained with propofol 3–6 mg/kg/h by state index of 25–50 and remifentanil 0.2–0.5 μg/kg/min. Patients were placed with a 28 or 32 thoracic drainage tube during the operation and they were managed by one chest drain connected to a digital chest drainage system. Followed by PCIA, all patients received MINB with 5 mL 0.35% ropivacaine at the end of the operation. Intravenous tropisetron 5 mg was administered to prevent postoperative nausea and vomiting. Then, the patients were transferred to the post-anesthesia care unit (PACU).
Modified Intercostal Nerve Block
Near the incision site where a chest drainage tube was inserted, the ultrasound transducer (S-Nerve; SonoSite Iberica S.L., Madrid, Spain) was placed perpendicular to the long axis of the upper rib (posterior axillary line level). As the previous protocol by our study,3 the 21G needle was inserted which targeted the lateral border of the upper rib in a caudal-to-cephalic direction along the long axis of the transducer. Then 5 mL of 0.35% ropivacaine combined with 0.025% dexamethasone was injected when the needle reached this special landmark, which facilitated the drug’s diffusion up, down, and back, between the anterior serratus muscle and the coastal space (S. Figure 1).
Postoperative Patient-Controlled Analgesia
The intervention group: PCIA protocols were DEX 0.05 µg/kg/h for 72 h diluted in 150 mL normal saline, a background infusion rate of 2 mL/h, and a 2 mL bolus with a lockout interval of 15 min. PCIA bolus dose was administered for visual analog scale (VAS) > 3 or on patient request.
The control group: PCIA protocols were sufentanil 3 µg/kg for 72 h diluted in 150 mL normal saline. PCIA parameter settings remained the same (2 mL bolus, a lockout time with 15 min, and 2 mL/h baseline infusion). PCIA bolus dose was also administered for VAS > 3 or on patient request.
As part of the multimodal analgesia, flurbiprofen 50 mg (twice daily) was administered intravenously for 72 h in two groups. Also, the patient would be administered a rescue analgesic of tramadol 100 mg 6 hourly if it was ineffective to press twice continuously.
Outcome
The primary outcome focused on a non-inferiority comparison of VAS score during coughing at 24 h after surgery. Secondary outcomes included the time to first analgesic request, PCIA pressing times, postoperative sufentanil consumption, time to first flatus, tramadol consumption, opioid-related effects, hospital stay, and the incidence of postoperative complications systematically.
The same research staff who were unaware of the assignment of the study group assessed the VAS scores at rest and coughing, and other outcomes systematically. Postoperative opioid consumption was calculated from the total background dose plus the bolus dose if required during 24 h, 48 h, and 72 h after surgery. The patient and relatives were instructed on how to use the analgesic pump. The device of the patient-controlled analgesia pumps could automatically record the exact time to press the pump and the total pressing times. Rescue tramadol consumption was defined as the total tramadol dose during 24 h, 48 h, and 72 h after surgery.
Sample Size
The primary objective was to evaluate whether dexmedetomidine-based opioid-sparing analgesia was non-inferior to the sufentanil-based approach in terms of VAS score during coughing at 24 h after surgery in VATS patients. According to our preliminary study conducted with ten patients (five in each group), the expected mean VAS score was 3.7 ± 0.4 in the intervention group and 3.2 ± 1.0 in the control group. Based on available study,7,8 a non-inferiority margin of 1 was set as a clinically relevant difference in change of VAS score. Thus, the non-inferiority was established when the upper boundary of the 95% CI for the mean difference was lower than 1. Using a power of 80% of the non-inferiority test, a significance level (alpha) of 0.05, and a mean margin in VAS score of 1, we calculated that a sample of 60 patients (1:1 allocation ratio) would be needed. Considering a supposed dropout rate of 15%, we planned to include 70 patients, 35 in each group.
Data Analysis
Statistical analysis was performed using PASS 15.0. The Kolmogorov–Smirnov test was used to check for normal distribution of data. The normally distributed data were analyzed using Student´s t-test. Nonparametric and non-normally distributed data were analyzed using the Mann–Whitney U-test. Mean ± standard deviation was estimated for age, and body mass index. The median (interquartile range) was estimated for VAS, PCIA pressing times, the time to first analgesic request, and sufentanil consumption. A nonparametric test was used to analyze PCIA pressing times, sufentanil consumption, time to first flatus, and postoperative hospital stay by the Mann–Whitney U-test. The 95% CI of the median difference was calculated with the Hodges–Lehmann test for the time to first rescue analgesic request. A chi-square test was applied for postoperative adverse events and complications. It was considered statistically significant when P < 0.05.
Results
A patient flow diagram is shown in Figure 1. 70 patients who met the inclusion criteria were allocated into two groups randomly. However, 10 patients were subsequently excluded: 5 patients changed to open thoracic surgery and 5 patients refused PCIA. Finally, a total of 60 patients (n=30 in the intervention group and n=30 in the control group) were analyzed.
 |
Figure 1 Flow diagram. |
Baseline characteristics were similar between groups (Table 1). There was no difference in VAS scores on coughing at 24 h between the intervention group and the control group (P >0.05, Table 2), with a median difference (95% CI) of [0 (0 to 1), P = 0.36] (Figure 2). The low boundary of the 95% confidence interval was > –1, therefore, non-inferiority was established.
 |
Table 1 Demographic Data and Surgical Characteristics |
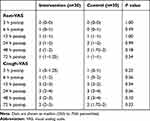 |
Table 2 VAS Scores |
Table 3 shows postoperative opioid consumption. There was no difference in the time to first analgesic request and the total number of PCIA activations. A marked decrease in sufentanil consumption was observed in the intervention group compared with the control group. The sufentanil consumption 3 days postoperatively was [0 (0–0)] µg in the intervention group vs [187.5 (150–210)] µg in the control group, with a median difference [187.5 (159.0 to 204.0), P = 0.00]. No rescue analgesia was used in each group.
 |
Table 3 Postoperative Opioid Consumption |
A significant difference in time to first flatus was observed in the intervention group [20.0 (15.9–22.3) vs 26.3 (22–33.0), P = 0.00]. In addition, there was no case of constipation in the intervention group, and five cases in the control group (0/30 vs 5/30, P = 0.02). In summary, the total adverse effects in the intervention group was lower than in the control group (2/30 vs 11/30, P = 0.00). However, postoperative length of stay was not significantly shortened in the intervention group (P = 0.07) (Table 4).
 |
Table 4 Postoperative Complications, Adverse Events and Outcome |
Discussion
This prospective study firstly demonstrated this novel opioid-sparing analgesia approach was not inferior to opioid-based analgesia protocol, with a reduction in time to first flatus.
Postoperative analgesia after thoracic surgery is a real challenge that requires reducing opioids perioperatively. The pleural drain is the main cause of pain after VATS. As an important component of multimodal analgesia, posterior intercostal nerve blockade9 with bupivacaine may be as effective as thoracic epidural analgesia in terms of postoperative pain originating from the pleural drain. In our study, we simplified the conventional approach of intercostal nerve blockade to one more superficial MINB and further optimized this to single-point injection. Combined with dexamethasone, the analgesic effect of MINB was prolonged and resulted in fewer opioids requirement. Single-shot intercostal nerves have not been widely used because of the short duration of action of local anesthetics; however, the availability of non-opioid analgesics, such as DEX10 and NSAIDs,11 offers the potential prolonged and supplemental analgesia effect. Therefore, we implemented a combination of MINB and non-opioid analgesic adjuvants to achieve a potential opioid-sparing effect. Compared to the traditional intercostal block-based approach,6 this novel opioid-sparing strategy prolonged the time to first request of analgesia, with lower PCIA pressing times and rescue analgesia, which may benefit from the opioid-sparing effect of MINB by extending 24 h after surgery.
Since visceral pain is innervated by the vagal and phrenic nerves, MINB does not affect visceral pain.12 DEX and NSAIDs, as non-opioid analgesics, are helpful to manage somatic pain.13 Anti-nociceptive effects of DEX to blunt increased MAP and HR have been confirmed especially.14 Animal studies have shown that dexmedetomidine can inhibit acute inflammatory visceral pain through NF-κB activation15 and chronic inflammatory visceral pain through the HDAC2 pathway and MEK/ERK/CREB pathway, suppressing visceral hypersensitivity.16,17 Thus, a clinical trial demonstrated that DEX ameliorated visceral pain after abdominal surgery in patients via a dose-dependent inhibitory on C-fibers and Aα-fibers.18 Also, our preliminary study3 showed an intra-operative opioid-sparing effect extending 48 h after surgery after MINB and intra-operative DEX infusion might be an alternative method to blunt visceral stress effectively in patients undergoing thoracoscopic lobectomy. This current study focused on the postoperative opioid-sparing effect and further demonstrated the feasibility of postoperative opioid-free analgesia. Another study6 showed that DEX 0.1 µg/kg/h added to PCIA without opioids provided adequate and safe postoperative analgesia, with no bradycardia, hypotension, or respiratory depression. According to our preliminary observation, we found that DEX 0.1 µg/kg/h may cause dizziness and drowsiness in patients, and a low dose of DEX 0.05 µg/kg/h was chosen in this study. DEX 0.05 µg/kg/h of PCIA is safe and feasible, with no side effect in postoperative sedatives. However, the optimal dose of DEX still warrants further investigation.
Importantly, high compliance with non-opioid enhanced recovery protocols significantly reduces opioid requirements and leads to improved outcomes.5 Although this opioid-sparing strategy minimized postoperative opioid requirements, there was no significant difference in the incidence of postoperative nausea and vomiting between groups. This similar outcome was consistent with recent evidence19,20 that opioid-free balanced anesthesia did not decrease the incidence of postoperative nausea and vomiting for noncardiac surgery. However, a remarkable decrease in time to first flatus was observed in this prospective study, and non-opioid requirements resulted in enhanced bowel recovery. Unfortunately, patients managed with the opioid-sparing approach had not appeared to be shorter in hospitalization. Indeed, whether implementation of an opioid-sparing protocol may enhance postoperative recovery is uncertain.21 A recent study22 showed that an enhanced recovery pathway has no benefit on postoperative hospital stay, morbidity, mortality, and readmission rates. Another retrospective study23 found an implementation of a multimodal analgesic pathway based on incisional nerve block could effectively reduce perioperative opioid consumption and length of stay. Nevertheless, the outcome of a novel opioid-sparing analgesic strategy for thoracoscopic surgery needs further study.
Limitation
This study has several limitations. Firstly, to avoid dizziness and drowsiness side effects, a safer dose of DEX 0.05 µg/kg/h was chosen. Tan et al's study24 showed DEX combined with sufentanil was effective for postoperative PCIA in patients undergoing VATS when the ED50 and ED95 are 0.0346 μg/kg/h and 0.0459 μg/kg/h, respectively. The optimal dose of DEX may require further exploration. Secondly, we did not collect the data on opioid consumption after discharge, and it may be the novel opioid-sparing effect in the long term. Lastly, this is a single-center study with a small sample size, so a large-scale randomized controlled trial would be needed to confirm the potential benefit.
Conclusion
Dexmedetomidine-based analgesia in combination with MINB was non-inferior to conventional sufentanil-based analgesia in providing analgesia after single-port thoracoscopic lobectomy, with a faster exhaust time. We believe that dexmedetomidine-based analgesia in combination with a multimodal analgesic regimen may be an effective alternative for thoracoscopic surgery.
Abbreviations
VATS, Single-port video-assisted thoracoscopic surgery; DEX, Dexmedetomidine; PCIA, Postoperative patient-controlled intravenous analgesia; NSIAD, Nonsteroidal anti-inflammatory drug; ASA, American Society of Anesthesiologists; MINB, Modified intercostal nerve block; ECG, Electrocardiogram; HR, Heart rate; MAP, Mean arterial pressure; PACU, Post-anesthesia care unit; VAS, Visual analogue scale; ERAS, Enhanced recovery after surgery; ED50, Median effective dose; ED95, 95% effective dose.
Data Sharing Statement
The raw data used in this study are available from the corresponding author ([email protected]) upon reasonable request.
Ethical Approval and Patient Consent
This prospective trial was approved by our institutional review board (approval No. PJ2020-01-27) on 9 January 2020 and conducted after written informed consent. All procedures were performed according to the Declaration of Helsinki.
Acknowledgments
The authors thank all the members of the Thoracic Surgery Department for their support.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by the National Nature Science Foundation of China (Grant No. 81870837) and Natural Science Foundation of Universities of Anhui Province (No.kj2021A0278).
Disclosure
The authors declare that they have no conflict of interest.
References
1. Cata JP, Keerty V, Keerty D, et al. A retrospective analysis of the effect of intraoperative opioid dose on cancer recurrence after non-small cell lung cancer resection. Cancer Med. 2014;3(4):900–908. doi:10.1002/cam4.236
2. Kumar K, Kirksey MA, Duong S, Wu CL. A review of opioid-sparing modalities in perioperative pain management: methods to decrease opioid use postoperatively. Anesth Analg. 2017;125(5):1749–1760. doi:10.1213/ane.0000000000002497
3. Cheng XQ, Cheng J, Zhou YN, et al. Anti-nociceptive effects of dexmedetomidine infusion plus modified intercostal nerve block during single-port thoracoscopic lobectomy: a double-blind, randomized controlled trial. Pain Physician. 2021;24(5):E565–E572.
4. Peng K, Zhang J, Meng XW, Liu HY, Ji FH. Optimization of postoperative intravenous patient-controlled analgesia with opioid-dexmedetomidine combinations: an updated meta-analysis with trial sequential analysis of randomized controlled trials. Pain Physician. 2017;20(7):569–596.
5. Wick EC, Grant MC, Wu CL. Postoperative multimodal analgesia pain management with nonopioid analgesics and techniques: a review. JAMA Surg. 2017;152(7):691–697. doi:10.1001/jamasurg.2017.0898
6. Miao Z, Wu P, Wang J, et al. Whole-course application of dexmedetomidine combined with ketorolac in nonnarcotic postoperative analgesia for patients with lung cancer undergoing thoracoscopic surgery: a randomized control trial. Pain Physician. 2020;23(2):E185–E193.
7. Park SY, Park JS, Choi GS, Kim HJ, Moon S, Yeo J. Comparison of analgesic efficacy of laparoscope-assisted and ultrasound-guided transversus abdominis plane block after laparoscopic colorectal operation: a randomized, single-blind, non-inferiority trial. J Am Coll Surg. 2017;225(3):403–410. doi:10.1016/j.jamcollsurg.2017.05.017
8. Hausken J, Fretland ÅA, Edwin B, et al. Intravenous patient-controlled analgesia versus thoracic epidural analgesia after open liver surgery: a prospective, randomized, controlled, noninferiority trial. Ann Surg. 2019;270(2):193–199. doi:10.1097/sla.0000000000003209
9. Rice DC, Cata JP, Mena GE, Rodriguez-Restrepo A, Correa AM, Mehran RJ. Posterior intercostal nerve block with liposomal bupivacaine: an alternative to thoracic epidural analgesia. Ann Thorac Surg. 2015;99(6):1953–1960. doi:10.1016/j.athoracsur.2015.02.074
10. Kang R, Jeong JS, Yoo JC, et al. Effective dose of intravenous dexmedetomidine to prolong the analgesic duration of interscalene brachial plexus block: a single-center, prospective, double-blind, randomized controlled trial. Reg Anesth Pain Med. 2018;43(5):488–495. doi:10.1097/AAP.0000000000000773
11. Thagaard KS, Jensen HH, Raeder J. Analgesic and antiemetic effect of ketorolac vs. betamethasone or dexamethasone after ambulatory surgery. Acta Anaesthesiol Scand. 2007;51(3):271–277. doi:10.1111/j.1399-6576.2006.01240.x
12. Novak-Jankovic V, Markovic-Bozic J. Regional anaesthesia in thoracic and abdominal surgery. Acta Clin Croat. 2019;58(Suppl 1):96–100. doi:10.20471/acc.2019.58.s1.14
13. Kim KH, Seo HJ, Abdi S, Huh B. All about pain pharmacology: what pain physicians should know. Korean J Pain. 2020;33(2):108–120. doi:10.3344/kjp.2020.33.2.108
14. Kakkar A, Tyagi A, Nabi N, Sethi AK, Verma UC. Comparison of clonidine and dexmedetomidine for attenuation of laryngoscopy and intubation response - A randomized controlled trial. J Clin Anesth. 2016;33:283–288. doi:10.1016/j.jclinane.2016.04.026
15. Lan J, Zheng J, Feng J, Peng W. Nrf2 mediates the antinociceptive activity of dexmedetomidine in an acute inflammatory visceral pain rat model by activating the NF-κB sensor. Cell Biochem Funct. 2020;38(1):97–105. doi:10.1002/cbf.3456
16. Liang M, Shao A, Tang X, Feng M, Wang J, Qiu Y. MiR-34a affects dexmedetomidine-inhibited chronic inflammatory visceral pain by targeting to HDAC2. BMC Anesthesiol. 2019;19(1):131. doi:10.1186/s12871-019-0801-z
17. Sun L, Zhou J, Sun C. MicroRNA-211-5p enhances analgesic effect of dexmedetomidine on inflammatory visceral pain in rats by suppressing ERK signaling. J Mol Neurosci. 2019;68(1):19–28. doi:10.1007/s12031-019-01278-z
18. Jiang Z, Zhou G, Song Q, Bao C, Wang H, Chen Z. Effect of intravenous oxycodone in combination with different doses of dexmedetomidine on sleep quality and visceral pain in patients after abdominal surgery: a randomized study. Clin J Pain. 2018;34(12):1126–1132. doi:10.1097/ajp.0000000000000645
19. Beloeil H, Garot M, Lebuffe G, et al. Balanced opioid-free anesthesia with dexmedetomidine versus balanced anesthesia with remifentanil for major or intermediate noncardiac surgery. Anesthesiology. 2021;134(4):541–551. doi:10.1097/aln.0000000000003725
20. Massoth C, Schwellenbach J, Saadat-Gilani K, et al. Impact of opioid-free anaesthesia on postoperative nausea, vomiting and pain after gynaecological laparoscopy - A randomised controlled trial. J Clin Anesth. 2021;75:110437. doi:10.1016/j.jclinane.2021.110437
21. Frauenknecht J, Kirkham KR, Jacot-Guillarmod A, Albrecht E. Analgesic impact of intra-operative opioids vs. opioid-free anaesthesia: a systematic review and meta-analysis. Anaesthesia. 2019;74(5):651–662. doi:10.1111/anae.14582
22. Brunelli A, Thomas C, Dinesh P, Lumb A. Enhanced recovery pathway versus standard care in patients undergoing video-assisted thoracoscopic lobectomy. J Thorac Cardiovasc Surg. 2017;154(6):2084–2090. doi:10.1016/j.jtcvs.2017.06.037
23. Rice D, Rodriguez-Restrepo A, Mena G, et al. Matched pairs comparison of an enhanced recovery pathway versus conventional management on opioid exposure and pain control in patients undergoing lung surgery. Ann Surg. 2021;274(6):1099–1106. doi:10.1097/SLA.0000000000003587
24. Tan XL, Chen YY, Hu B, et al. 右美托咪定复合舒芬太尼用于胸腔镜术后静脉镇痛的量效关系 [Dose-response relationship of dexmedetomidine combined with sufentail for postoperative intravenous analgesia in video-assisted thoracoscopic surgery]. Zhongguo Yi Xue Ke Xue Yuan Xue Bao. 2019;41(3):373–378. Chinese. doi:10.3881/j.issn.1000-503X.10881
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.