Back to Journals » Journal of Hepatocellular Carcinoma » Volume 10
A Novel Neutrophil-to-Lymphocyte Ratio and Sarcopenia Based TACE-Predict Model of Hepatocellular Carcinoma Patients
Authors Wang S, Zhang X, Chen Q, Jin ZC, Lu J, Guo J
Received 21 February 2023
Accepted for publication 12 April 2023
Published 20 April 2023 Volume 2023:10 Pages 659—671
DOI https://doi.org/10.2147/JHC.S407646
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 5
Editor who approved publication: Dr David Gerber
Shangyuan Wang, Xuanpu Zhang, Qi Chen, Zhi-Cheng Jin, Jian Lu, Jinhe Guo
Center of Interventional Radiology & Vascular Surgery, Department of Radiology, Zhongda Hospital, Medical School, Southeast University, Nanjing, 210009, People’s Republic of China
Correspondence: Jian Lu; Jinhe Guo, Center of Interventional Radiology & Vascular Surgery, Department of Radiology, Zhongda Hospital, Southeast University, 87 Dingjiaqiao Road, Nanjing, 210009, People’s Republic of China, Tel +86-25-83262230 ; +86-25-83272121, Email [email protected]; [email protected]
Purpose: Transarterial chemoembolization (TACE) was commonly applied in hepatocellular carcinoma (HCC) patients across BCLC A-C stages with heterogeneous outcomes in real-world practice. We aimed to develop a neutrophil-to-lymphocyte ratio (NLR) and sarcopenia-based prognostic nomogram to estimate the prognosis of HCC patients after TACE treatment.
Patients and Methods: Between June 2013 and December 2019, a total of 364 HCC patients who underwent TACE were included and randomly assigned to the training (n=255) and the validation cohort (n=109). Sarcopenia was diagnosed based on the third lumbar vertebra skeletal muscle mass index (L3-SMI). The multivariate Cox proportional risk model was used to generate a nomogram.
Results: NLR ≥ 4.0, sarcopenia, alpha-fetoprotein (AFP) ≥ 200 ng/mL, albumin-bilirubin (ALBI) grade 2 or 3, number of lesions (≥ 2), and maximum size of the lesion (≥ 5 cm) were independent predictors for overall survival (OS) (P < 0.05). The calibration curve shows that the predicted results agree well with the observed results. The time-dependent areas under the receiver-operating characteristic curves for OS at 1, 2, and 3 years predicted by the nomogram were 0.818/0.827, 0.742/0.823, and 0.748/0.836 in both training and validation cohorts. Nomogram can divide patients into low-, medium- and high-risk groups based on predictor factors. The C-indexes of the nomogram for OS were 0.782/0.728 in the training and validation cohorts, outperforming other currently available models.
Conclusion: A novel nomogram based on NLR and sarcopenia may be useful to predict the prognosis of HCC patients who underwent TACE across BCLC A-C stage patients.
Keywords: hepatocellular carcinoma, transarterial chemoembolization, neutrophil-to-lymphocyte ratio, sarcopenia, albumin-bilirubin, nomogram
Introduction
Hepatocellular carcinoma (HCC) is the sixth most common cancer and the third leading cause of cancer-related death in 2020 worldwide.1,2 According to the recommendation of the Barcelona Clinical Liver Cancer (BCLC) staging system, transarterial chemoembolization (TACE) is the first choice for the treatment of intermediate-stage HCC.3 The BRIDGE study based on real-world data found that the first treatment of HCC patients across all stages was most frequently transarterial chemoembolization in North America, Europe, China, and South Korea4. Meanwhile, because the nature of HCC is highly heterogeneous, not all HCC patients can benefit from TACE. Therefore, predictor tools of overall survival (OS) can be helpful in clinical decision-making.4,5 So far, various prognostic models have been developed to predict survival after TACE, including the HAP score,6 ALBI-TAE score,7 and six-and-twelve score.8 These models were based on routinely available parameters, including tumor factors (tumor number and maximum size), alpha-fetoprotein (AFP) level, and bilirubin. However, most of these models were built to predict prognosis after TACE in BCLC A or B stage patients, while BCLC-C stage patients were excluded.
Recently, increasing evidence showed that systemic inflammation plays a vital role in tumor progression and the long-term prognosis of patients with established cancers.9 The neutrophil-to-lymphocyte ratio (NLR) is a readily available systemic inflammatory marker associated with cancer progression. High NLR has been proven to be related to poor prognosis of cancer, including hepatocellular carcinoma.10–12 Systemic inflammation can also accelerate metabolism and make patients’ nutritional status worse.13 As a reflection of nutritional status, sarcopenia is a progressive and generalized skeletal muscle disorder characterized by accelerated loss of muscle mass and function. It is a common syndrome in aging patients with chronic disorders. Sarcopenia increases the risk of falls and fractures, causes an impaired ability to perform activities of daily living, and leads to a lower quality of life, even death.14,15 Patients with chronic diseases showed higher prevalence rates of sarcopenia: 29.7% in cardioVascular disease, 24% in chronic obstructive pulmonary disease, and 48.1% in liver cirrhosis.16 In recent years, sarcopenia has been considered an independent prognostic factor for the outcome of HCC patients who accepted TACE or hepatectomy.17–19
As far as we know, no previous study has explored the influence of both NLR and sarcopenia on the outcome of HCC patients undergoing TACE. We aimed to develop a novel prognostic model based on NLR and sarcopenia to predict the prognosis of BCLC A-C HCC patients after TACE in real-world practice and compared the prognostic utility of the new model with those of conventional models.
Materials and Methods
Study Design
Electronic data of patients with HCC treated by TACE from June 2013 to December 2019 at the authors’ Hospital was queried and analyzed. All patients were diagnosed as HCC by diagnostic criteria20 and treated with a conventional TACE regimen. Relevant data were collected, including demographic data (age, sex, history of hepatitis B, hepatitis C), cirrhosis (diagnosed through histopathologic examination or a combination of clinical, laboratory, and imaging findings),21 and portal hypertension, laboratory data (alanine aminotransferase ALT, aspartate aminotransferase AST, total bilirubin TBIL, serum albumin ALB, neutrophil count, lymphocyte count), tumor characteristics (tumor number, tumor size), tumor biomarkers (alpha-fetoprotein AFP, carcinoembryonic antigen CEA, carbohydrate antigen 19–9 CA 19–9), liver function grade (Child-Pugh class, ALBI grade) and abdominal CT imaging data. The inclusion criteria included 1) TACE as the first recorded treatment; 2) Child-Pugh class A or B grade; 3) blood sample and abdominal CT examination were performed within 7 days before TACE treatment. Patients were excluded based on the following criteria: 1) complicated with primary tumors of other organs; 2) with systemic inflammatory reaction; 3) incomplete clinical data. The protocol conformed to the ethical guidelines of the 1975 Declaration of Helsinki. Each patient gave written informed consent prior to treatment.
TACE Procedure
Femoral artery puncture was performed by the Seldinger technique. After the puncture, the catheter was selected into the blood supply branch of the liver tumor under fluoroscopic guidance. Angiographic images were analyzed to confirm the location, size, number of lesions, and all the tumor-feeding arteries. According to tumor volume, liver function, and tumor condition, the appropriate amount of ethiodized oil (Lipiodol Ultra-Fluide; Guerbet, Roissy, France) and doxorubicin (Adriamycin; Shenzhen Main Luck Pharmaceuticals Inc, Shenzhen, China) were perfused. Then, 300–500 μm Gelfoam particles (Hangzhou ALICON Pharm SCI&TEC CO. LTD) were injected to embolize the tumor-feeding artery until the arterial blood flow slowed. After embolization, confirmatory angiography was performed to embolize the tumor-related blood supply artery to achieve the de-vascularization effect of the target tumor.22 After first TACE treatment, patients were followed every 6–8 weeks with measurement of serum AFP, liver function, CT or MRI. In cases of viable tumors or intrahepatic recurrences, subsequent TACE was arranged if general condition acceptable All TACE procedures were performed by doctors with at least 10 years of experience.
Assessment of Sarcopenia and NLR
The third lumbar vertebra skeletal muscle mass index (L3-SMI) was used to evaluate sarcopenia.15 Based on preoperative abdominal CT image data, all skeletal muscle area in the third lumbar vertebral plane was sketched by Image J software (National Institutes of Health, Maryland), and the L3-SMI was obtained according to the formula. L3-SMI calculation formula: L3-SMI = all skeletal muscle area in L3 vertebral plane/height cm2/m2. Images and calculated L3-SMI were assessed by an expert radiologist with over 15 years of experience in CT scanning and image postprocessing. NLR was defined as the ratio derived from the division of the neutrophil count by the lymphocyte count. The optimal cutoff levels for L3-SMI and NLR were calculated by the X-tile software (Yale University, New Haven, CT). In this study, sarcopenia was defined as follows: for male, an L3-SMI less than 49 cm2/m2; for female, an L3-SMI less than 36 cm2/m2 The optimal cutoff value for the NLR was 4.0.
Statistical Analysis
All patients were randomly divided into training and validation cohorts according to the ratio of 7:3 through R package “caret“. Quantitative variables were presented as median with interquartile range (IQR) and classified variables were expressed as frequency or percentage of events. The chi-square test was used to compare category variables among groups, and Student’s t-test or non-parametric Mann–Whitney U-test was used to compare continuous variables. Overall survival was defined as the time between surgery and death from any cause or until the last follow-up. Survival curves were estimated by the Kaplan–Meier method and compared by Log rank test. Cox regression analysis was used to analyze the related factors affecting prognosis. Based on the Cox regression analysis, variables with 2-sided P <0.05 were included in the construction of the prognosis nomogram. The receiver operating characteristic (ROC) curves were used to assess the diagnostic performance of the nomogram. Calibration curves were constructed to compare predicted and observed survival rates. The R package “rms” was used to construct and validate the prognostic nomogram. The 1-year, 2-year, and 3-year OS nomogram calibration curves were used to evaluate the consistency between predicted and observed survival rates. Harrell’s consistency index (C-index) was used to compare with prognostic models, including the HAP score, ALBI-TAE score, and six-and-twelve score6–8 in both training and validation cohorts. This study used SPSS 26.0 (SPSS Inc., Chicago, IL) and R ver. 4.2.1 (R Foundation for Statistical Computing, Vienna, Austria) to analyze and process the data.
Results
Baseline Characteristic
A total of 364 patients were enrolled and randomly divided into the training cohort (n=255) and validation cohort (n=109). Patients received a total of 1062 TACE sessions. The median age of patients was 58 years old, and 82.4% of patients were male. HBV infection was the most common cause of HCC (67.9%) and multiple tumors in 199 patients (54.7%). BCLC stage A in 84 cases (23.1%), stage B in 193 cases (53.0%), and stage C in 87 cases (23.9%). There was no significant difference between the two sets (P > 0.05) except in tumor number and BCLC staging (Table 1).
 |
Table 1 Baseline Characteristics |
Overall Survival
As of the final follow-up date (December 31, 2021), the median OS of total patients was 11.6 months (IQR 6.8–24.2). Among them, the median OS of patients at BCLC-A, B, and C stage were 19.2 months (IQR 11.1–35.2), 11.6 months (IQR 6.4–24.4), and 8.5 months (IQR 5.2–13.6), respectively. In the training and validation cohort, the median OS was 11.4 months (IQR 6.6–24.5) versus 12.0 months (IQR 7.6–23.5). A total of 242 (94.9%) of 255 participants in the training cohort and 104 (95.4%) of 109 in the validation cohort were demised. The 1-year, 2-year, and 3-year OS rates were 47.8%, 25.5%, and 11.4% in the training cohort and 50.5%, 23.9%, and 15.6% in the validation cohort, respectively. There was no significant difference in overall survival time between the two groups (P=0.572). There was a significant difference in the OS between patients with or without sarcopenia. In the training cohort, the median survival time was 16.2 months (IQR 8.2–29.1) versus 9.4 months (IQR 6.1–16.6). For patients in the validation cohort, the median OS was 14.9 months (IQR 0.8–2.2) versus 10.6 months (IQR 5.4–16.1).
Prognostic Factors of OS
In order to identify the main influencing factors of OS after TACE, the clinical characteristic factors collected in this study were analyzed by univariate analysis and multivariate analysis (Table 2). According to the results of Cox regression analysis, sarcopenia, preoperative AFP level ≥200 ng/mL, NLR≥4.0, ALBI grade, maximum tumor size (≥5cm), and tumor number (≥2) (P<0.05) were selected to be the independent risk factors for OS. Kaplan–Meier curve of these independent risk factors in the training cohort (Figure 1).
 |
Table 2 Univariate and Multivariate Analyses of Prognostic Factors for OS |
 |
Figure 1 Kaplan–Meier curves of risk group stratification for OS in the training cohort (A–F). |
Construction, Validation and Comparison of the Nomogram
The six variables obtained from the Cox regression analysis were used to construct the nomograms for OS. In both the training and validation cohorts, nomogram was used by adding points determined on the predictor point scale. Each subtype in the variable was assigned a score. The probability of the result can be calculated by drawing a vertical line on the total score to obtain the estimated 1-year, 2-year, and 3-year survival rates were plotted (Figure 2).
 |
Figure 2 Nomogram used to predict the 1-year, 2-year and 3-year survival rate of hepatocellular carcinoma patients. |
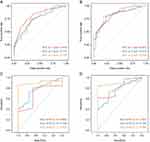
The application of the predictive model to the training cohort showed that the time-dependent areas under receiver operating characteristic curve (AUROC) values were 0.818 (95% CI 0.763–0.902), 0.742 (95% CI 0.693–0.795), and 0.748 (95% CI 0.718–0.806) at 1-year, 2-year, and 3-year, and in validation cohorts were 0.827 (95% CI 0.749–0.889), 0.823 (95% CI 0.755–0.874), and 0.836 (95% CI 0.790–0.898) (Figure 3A and B). In both the training and validation cohort, the AUROC values were 0.685 (95% CI 0.378–0.992)/0.803 (95% CI 0.619–0.88), 0.769 (95% CI 0.623–0.915)/0.769 (95% CI 0.623–0.915), and 0.909 (95% CI 0.823–0.995)/0.889 (95% CI 0.803–0.987) on BCLC-A, -B, and -C stage patients (Figure 3C and D). In addition, the calibration curves of 1-year, 2-year, and 3-year OS probabilities show that the prediction efficiency of the nomogram is in good agreement with the actual observation results in both the training and validation cohort (Figure 4). In the training and validation cohort, Harrell’s OS predictive C-index was 0.782 (95% CI 0.664–0.899) and 0.728 (95% CI 0.496–0.960), higher than single variable (Supplementary Table 1 and Supplementary Figure 1), which were also higher than those of other models, including hepatoma arterial-embolization prognostic (HAP) score, ALBI-TAE score and six-and-twelve score (Table 3).
 |
Table 3 Comparison of Nomogram and Other Prognostic Systems |
Risk Stratification
Based on the nomogram, patients were divided into the low-risk, medium-risk, and high-risk groups (n=79, n=115, n=61) according to the prediction probability of OS, which provided a reasonable basis for the prognosis classification of OS patients in the training cohort. For the low-, medium-, and high-risk groups in the training cohort, the median survival time was 28.4 months (IQR 23.8–33.0), 15.9 months (IQR 13.3–18.5), and 8.2 months (95% CI 6.0–10.4), respectively. The patients in the validation cohort were also divided into three groups (n=33, n=51, and n=25). For each group, the median survival time was 31.0 months (IQR CI 24.2–37.7), 14.6 months (IQR 11.7–17.5), and 7.5 months (IQR 5.8–9.3) months, respectively. In the training cohort and the validation cohort, the survival curves of the three stratifications were significantly different (log-rank P < 0.0001) (Figure 5). Besides, for the three groups in the training cohort, the median NLR was 2.1 (IQR 1.3–3.1), 3.4 (IQR 2.2–5.1), and 6.4 (IQR 4.1–9.6), and for the different group of patients in the validation cohort, the median NLR was 1.3 (IQR 0.8–2.2), 4.1 (IQR 2.4–6.8), and 6.9 (IQR 4.1–11.5), respectively.
 |
Figure 5 Kaplan-Meier OS curves for subgroups of patients. Patients were stratified by the nomogram in the training cohort (A) and validation cohort (B). |
Discussion
In real-world practice, TACE is applied across all BCLC stages of HCC.23 However, due to the high heterogeneity of HCC, the prognosis of patients who underwent TACE was quite different. Therefore, individualized models were needed to be developed to screen patients suitable for TACE. In this study, a novel prognostic model was built based on NLR, sarcopenia, AFP level, ALBI grade, tumor number, and maximum tumor size. The model incorporated NLR and sarcopenia simultaneously, both of which have been proven by previous studies to be important predictors of HCC. The novel nomogram shows good predictive performance after validation and comparison.
In both training and validation cohorts, data of patients with BCLC A-C stages were collected and put into the nomogram for evaluation. The AUROC values showed that the nomogram has good performance among all BCLC A-C stage patients. The median OS of 11.5 months in the current cohort was shorter than that of 19–38 months reported by Llovet et al.24 Probably because more advanced patients were included in the current study, with nearly 24% BCLC-C stage patients (Table 1). In fact, not only patients with BCLC A or BCLC B, but also those with BCLC-C stage received TACE treatment in the real-world practice. The study population in the current study seemed more representative than that of other studies. Based on these characteristics, this nomogram may be more suitable across BCLC-stage HCC patients.
Inflammation is a well-known inducing factor of tumors and drives tumor growth, development, and metastasis.25 About 90% of HCC progression is due to the induction of potential chronic liver inflammation and fibrosis. Chronic inflammation caused by hepatitis B or hepatitis C virus infection is key to HCC susceptibility.1 NLR was selected to assess the inflammatory immune status of the body, which can be easily obtained in the clinical record system. High NLR has been proven to be associated with poor prognosis of various solid tumors.11 In a prospective study, Johnson et al found that high NLR is an independent risk factor for HCC patients’ outcomes.26 In this study, a multivariate analysis showed that NLR is an independent predictor for HCC patients. As the current nomogram could stratify patients into the three strata, for the different groups in the training cohort, the median NLR was 2.1, 3.4, and 6.4, respectively, and for the different group of patients in the validation cohort, the median NLR was 1.3, 4.1, and 6.9, respectively. Low NLR has proven to be a significant prognostic factor for better survival.
The systemic inflammatory response of tumors profoundly influences the host’s metabolism and nutritional status.13 Inflammatory cytokines have been shown to promote muscle atrophy, eventually stimulating protein breakdown and inhibiting muscle synthesis. Studies have shown that higher inflammatory levels are related to sarcopenia.27 Feliciano et al28 and Petrova et al29 have found that high NLR in patients diagnosed with colorectal cancer or non-small-cell lung cancer is related to the occurrence and development of sarcopenia. Sarcopenia is characterized by decreased skeletal muscle mass and function that are common in cancer patients and associated with adverse outcomes of many cancers, including esophageal and gastric cancer.30,31 Sarcopenia has also been proven to be associated with poor prognosis in patients who underwent TACE or hepatectomy.17,19,32 According to the calculated cutoff levels, 210 (57.7%) patients were diagnosed with sarcopenia. There was a significant difference in the OS between patients with or without sarcopenia. In the training cohort, the median survival time was 16.2 months versus 9.4 months. For patients in the validation cohort, the median OS was 14.9 months versus 10.6. In this study, a third lumbar vertebra skeletal muscle mass index (L3-SMI) was used to define sarcopenia, compared with common systemic nutrition indicators such as body mass index (BMI),33 L3-SMI was obtained from abdominal CT images before TACE, it can avoid the influence of weight gain caused by accompanying symptoms such as ascites and reflect the muscle content of the body more precisely.
The widespread use of TACE has stimulated the development of scoring systems to predict patient survival. Several milestone models have been developed in past decade, including the HAP score, ALBI-TAE score, and six-and-twelve score. Among them, the HAP score was further verified and showed good performance in an international cohort of 3030 patients.34 While the ALBI-TAE score and six-and-twelve score have not been verified in external cohort so far. Of note, the HAP score was developed in BCLC-A and BCLC-B stages HCC population while the ALBI-TAE score and six-and-twelve score were developed in only BCLC-B stage HCC population. However, TACE was applied in HCC patients across BCLC A-C stages in clinical practice. Therefore, a common model is needed to predict the prognosis of BCLC A-C HCC patients after TACE. In the current study, the nomogram showed better prediction ability than these models in same population, with a higher C-index (0.782/0.728) compared to the HAP score (0.492/0.451), ALBI-TAE score (0.599/0.615), and six-and-twelve score (0.628/0.635). Theoretically, the nomogram may be beneficial to screen HCC candidates for TACE and rationalize the application of TACE in clinical practice.
There are some limitations in this study. First, the data of study population were retrospectively collected from a single high-volume center, and the external validation was not conducted. Second, as this was a retrospective study, muscle strength loss was not included to measure sarcopenia. Thirdly, most patients in this study were infected with HBV. While the performance of this nomogram in HCC population with hepatitis C virus or non-alcoholic fatty liver disease was not clear yet.
Conclusion
A novel nomogram based on NLR and sarcopenia may be useful to predict the prognosis of HCC patients who underwent TACE across BCLC A-C stage patients.
Abbreviations
BCLC, Barcelona Clinic Liver Cancer; HCC, hepatocellular carcinoma; NLR, neutrophil-to-lymphocyte ratio; ALBI, albumin-bilirubin; ALT, alanine aminotransferase; AST, aspartate aminotransferase; AFP, alpha-fetoprotein; L3-SMI, third lumbar vertebra skeletal muscle mass index; HBV, hepatitis B virus; HCV, hepatitis C virus; OS, overall survival; TACE, transarterial chemoembolization; CI, confidence interval; IQR, interquartile range; AUROC, areas under receiver operating characteristic curve; BMI, body mass index; CT, computed tomography; NAFLD, non-alcoholic fatty liver disease; HAP, hepatoma arterial-embolization prognostic.
Data Sharing Statement
All relevant data are available within the manuscript and its supplementary material files. Further enquiries can be directed to the corresponding author (Jinhe Guo, [email protected]).
Ethical Approval and Informed Consent Statement
Written informed consent for data use was obtained from all patients. This study was approved by the Ethics Committee of Zhongda Hospital, Medical School, Southeast University.
Acknowledgments
The authors thank the patients and their families for participating in this study.
Author Contributions
All authors made a significant contribution to the work whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; agreed to submit to the current journal; and agreed to be accountable for all aspects of the work.
Funding
The study was supported by Jiangsu Province Key Research and Development Plan Program (BE2020785, BE2022855), National Natural Science Foundation of China (81827805, 82001935), Zhi-Shan Scholar Program of Southeast University (2242022R40069), and National Key Research and Development Program (2018YFA0704100, 2018YFA0704104). The funders of the study had no role in study protocol design, data analysis and interpretation, or writing of the report.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Llovet JM, Kelley RK, Villanueva A, et al. Hepatocellular carcinoma. Nat Rev Dis Primers. 2021;7(1):6. doi:10.1038/s41572-020-00240-3
2. Sung H, Ferlay J, Siegel RL, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71(3):209–249. doi:10.3322/caac.21660
3. European Association for the Study of the Liver. Electronic address eee, European Association for the Study of the L. EASL Clinical Practice Guidelines: management of hepatocellular carcinoma. J Hepatol. 2018;69(1):182–236. doi:10.1016/j.jhep.2018.03.019
4. Chang Y, Jeong SW, Young Jang J, Jae Kim Y. Recent Updates of Transarterial Chemoembolization in Hepatocellular Carcinoma. Int J Mol Sci. 2020;21(21):8165. doi:10.3390/ijms21218165
5. Liu PH, Hsu CY, Hsia CY, et al. Prognosis of hepatocellular carcinoma: assessment of eleven staging systems. J Hepatol. 2016;64(3):601–608. doi:10.1016/j.jhep.2015.10.029
6. Kadalayil L, Benini R, Pallan L, et al. A simple prognostic scoring system for patients receiving transarterial embolisation for hepatocellular cancer. Ann Oncol. 2013;24(10):2565–2570. doi:10.1093/annonc/mdt247
7. Lee IC, Hung YW, Liu CA, et al. A new ALBI-based model to predict survival after transarterial chemoembolization for BCLC stage B hepatocellular carcinoma. Liver Int. 2019;39(9):1704–1712. doi:10.1111/liv.14194
8. Wang Q, Xia D, Bai W, et al. Development of a prognostic score for recommended TACE candidates with hepatocellular carcinoma: a multicentre observational study. J Hepatol. 2019;70(5):893–903. doi:10.1016/j.jhep.2019.01.013
9. Diakos CI, Charles KA, McMillan DC, Clarke SJ. Cancer-related inflammation and treatment effectiveness. Lancet Oncol. 2014;15(11):e493–503. doi:10.1016/S1470-2045(14)70263-3
10. Mei Z, Shi L, Wang B, et al. Prognostic role of pretreatment blood neutrophil-to-lymphocyte ratio in advanced cancer survivors: a systematic review and meta-analysis of 66 cohort studies. Cancer Treat Rev. 2017;58:1–13. doi:10.1016/j.ctrv.2017.05.005
11. Templeton AJ, McNamara MG, Seruga B, et al. Prognostic role of neutrophil-to-lymphocyte ratio in solid tumors: a systematic review and meta-analysis. J Natl Cancer Inst. 2014;106(6):dju124. doi:10.1093/jnci/dju124
12. Young S, Cam I, Gencturk M, et al. Inflammatory Scores: comparison and Utility in HCC Patients Undergoing Transarterial Chemoembolization in a North American Cohort. J Hepatocell Carcinoma. 2021;8:1513–1524. doi:10.2147/JHC.S335183
13. Zhang Q, Song MM, Zhang X, et al. Association of systemic inflammation with survival in patients with cancer cachexia: results from a multicentre cohort study. J Cachexia Sarcopenia Muscle. 2021;12(6):1466–1476. doi:10.1002/jcsm.12761
14. Cruz-Jentoft AJ, Sayer AA. Sarcopenia. Lancet. 2019;393(10191):2636–2646. doi:10.1016/S0140-6736(19)31138-9
15. Cruz-Jentoft AJ, Bahat G, Bauer J, et al. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing. 2019;48(1):16–31. doi:10.1093/ageing/afy169
16. Hsu CS, Kao JH. Sarcopenia and chronic liver diseases. Expert Rev Gastroenterol Hepatol. 2018;12(12):1229–1244. doi:10.1080/17474124.2018.1534586
17. Loosen SH, Schulze-Hagen M, Bruners P, et al. Sarcopenia Is a Negative Prognostic Factor in Patients Undergoing Transarterial Chemoembolization (TACE) for Hepatic Malignancies. Cancers. 2019;11(10):1503. doi:10.3390/cancers11101503
18. Voron T, Tselikas L, Pietrasz D, et al. Sarcopenia Impacts on Short- and Long-term Results of Hepatectomy for Hepatocellular Carcinoma. Ann Surg. 2015;261(6):1173–1183. doi:10.1097/SLA.0000000000000743
19. Fujiwara N, Nakagawa H, Kudo Y, et al. Sarcopenia, intramuscular fat deposition, and visceral adiposity independently predict the outcomes of hepatocellular carcinoma. J Hepatol. 2015;63(1):131–140. doi:10.1016/j.jhep.2015.02.031
20. Jelic S, Sotiropoulos GC; Group EGW. Hepatocellular carcinoma: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2010;21(Suppl 5):v59–64. doi:10.1093/annonc/mdq166
21. Tsochatzis EA, Bosch J, Burroughs AK. Liver cirrhosis. Lancet. 2014;383(9930):1749–1761. doi:10.1016/S0140-6736(14)60121-5
22. Tsurusaki M, Murakami T. Surgical and Locoregional Therapy of HCC: TACE. Liver Cancer. 2015;4(3):165–175. doi:10.1159/000367739
23. Park JW, Chen M, Colombo M, et al. Global patterns of hepatocellular carcinoma management from diagnosis to death: the BRIDGE Study. Liver Int. 2015;35(9):2155–2166. doi:10.1111/liv.12818
24. Llovet JM, De Baere T, Kulik L, et al. Locoregional therapies in the era of molecular and immune treatments for hepatocellular carcinoma. Nat Rev Gastroenterol Hepatol. 2021;18(5):293–313. doi:10.1038/s41575-020-00395-0
25. Greten FR, Grivennikov SI. Inflammation and Cancer: triggers, Mechanisms, and Consequences. Immunity. 2019;51(1):27–41. doi:10.1016/j.immuni.2019.06.025
26. Johnson PJ, Dhanaraj S, Berhane S, Bonnett L, Ma YT. The prognostic and diagnostic significance of the neutrophil-to-lymphocyte ratio in hepatocellular carcinoma: a prospective controlled study. Br J Cancer. 2021;125(5):714–716. doi:10.1038/s41416-021-01445-3
27. Bano G, Trevisan C, Carraro S, et al. Inflammation and sarcopenia: a systematic review and meta-analysis. Maturitas. 2017;96:10–15. doi:10.1016/j.maturitas.2016.11.006
28. Feliciano EMC, Kroenke CH, Meyerhardt JA, et al. Association of Systemic Inflammation and Sarcopenia With Survival in Nonmetastatic Colorectal Cancer: results From the C SCANS Study. JAMA Oncol. 2017;3(12):e172319. doi:10.1001/jamaoncol.2017.2319
29. Petrova MP, Donev IS, Radanova MA, et al. Sarcopenia and high NLR are associated with the development of hyperprogressive disease after second-line pembrolizumab in patients with non-small-cell lung cancer. Clin Exp Immunol. 2020;202(3):353–362. doi:10.1111/cei.13505
30. Lin JX, Lin JP, Xie JW, et al. Prognostic Value and Association of Sarcopenia and Systemic Inflammation for Patients with Gastric Cancer Following Radical Gastrectomy. Oncologist. 2019;24(11):e1091–e1101. doi:10.1634/theoncologist.2018-0651
31. Elliott JA, Doyle SL, Murphy CF, et al. Sarcopenia: prevalence, and Impact on Operative and Oncologic Outcomes in the Multimodal Management of Locally Advanced Esophageal Cancer. Ann Surg. 2017;266(5):822–830. doi:10.1097/SLA.0000000000002398
32. Yabusaki N, Fujii T, Yamada S, et al. Adverse impact of low skeletal muscle index on the prognosis of hepatocellular carcinoma after hepatic resection. Int J Surg. 2016;30:136–142. doi:10.1016/j.ijsu.2016.04.049
33. Hagstrom H, Tynelius P, Rasmussen F. High BMI in late adolescence predicts future severe liver disease and hepatocellular carcinoma: a national, population-based cohort study in 1.2 million men. Gut. 2018;67(8):1536–1542. doi:10.1136/gutjnl-2016-313622
34. Waked I, Berhane S, Toyoda H, et al. Transarterial chemo-embolisation of hepatocellular carcinoma: impact of liver function and vascular invasion. Br J Cancer. 2017;116(4):448–454. doi:10.1038/bjc.2016.423
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.