Back to Journals » International Journal of Women's Health » Volume 12
A Multilevel Analysis of Factors Associated with Teenage Pregnancy in Ethiopia
Authors Kefale B , Yalew M , Damtie Y , Adane B
Received 29 May 2020
Accepted for publication 3 September 2020
Published 6 October 2020 Volume 2020:12 Pages 785—793
DOI https://doi.org/10.2147/IJWH.S265201
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Professor Elie Al-Chaer
Bereket Kefale,1 Melaku Yalew,1 Yitayish Damtie,1 Bezawit Adane2
1Department of Reproductive and Family Health, School of Public Health, College of Medicine and Health Sciences, Wollo University, Dessie, Ethiopia; 2Department of Biostatistics and Epidemiology, School of Public Health, College of Medicine and Health Sciences, Wollo University, Dessie, Ethiopia
Correspondence: Bereket Kefale
Department of Reproductive and Family Health, School of Public Health, College of Medicine and Health Sciences, Wollo University, PO Box: 1145, Dessie, Ethiopia
Tel +251933807117
Fax + 251331190586
Email [email protected]
Background: A significant number of girls in Ethiopia begin childbearing at an early age. Teenage pregnancy is the main contributor to maternal and child morbidity and mortality, and the vicious cycle of ill-health and poverty. However limited evidence exists about individual- and community-level factors affecting teenage pregnancy in Ethiopia.
Methods: This study used data from the 2016 Ethiopian Demographic and Health Survey (EDHS). A total of 3381 (weighted) teenagers aged 15– 19 years were included in the study. A two-stage stratified cluster was used. Data were analyzed using Stata version 14. Multilevel mixed effect logistic regression was used to identify factors affecting teenage pregnancy.
Results: Being 17 (AOR=9.26, 95% CI=2.67– 32.04), 18 (AOR=9.53, 95% CI=2.97– 30.04) and 19 years old (AOR=20.01, 95% CI=5.94– 67.39), uneducated (AOR=3.83, 95% CI=1.05– 14.00), primary educated (AOR=3.34, 95% CI=1.01– 11.08), being married (AOR=70.12, 95% CI=27.55– 178.4), and communities with a higher proportion of poor (AOR=3.86, 95% CI=1.80– 8.26) were predictors of teenage pregnancy.
Conclusion: Age, educational status, and marital status from individual-level factors, and community wealth status from community-level factors were predictors of teenage pregnancy. The government should strive to improve female education, and fight against early marriage and sexual initiation.
Keywords: teenage pregnancy, pregnancy in adolescence, multi-level analysis, Ethiopia
Introduction
The World Health Organization (WHO) defines adolescents as people between 10–19 years of age.1 Adolescents constitute about one-sixth and one-fourth of the populations in the World and Sub-Saharan Africa (SSA), respectively.2 Adolescents are not knowledgeable about sexuality, and turn away from sexual and reproductive health services. Due to this, they are victims of sexual and reproductive health risks and consequences.3 About 21 million and 19 million girls aged 15–19 years in the developing world become pregnant and give birth every year, respectively.4 A meta-analysis done in Africa showed that the overall pooled prevalence of teenage pregnancy was 18.8% and 19.3% in Africa and Sub-Saharan African, respectively.5 The prevalence of teenage pregnancy in Ethiopia showed slow reduction; decreased from 16.3% in 2000 to 12.5% in the 2016 Ethiopian Demographic and Health Survey (EDHS).6–8
Teenage pregnancy has serious consequences for both the mother and the newborn. Looking at its consequence for the mother, complications during pregnancy and childbirth are the leading cause of death among girls aged 15–19 years globally.9 Teenage mothers face higher risks of eclampsia, puerperal endometritis, systemic infection, and unsafe abortion.4,10 Teenage pregnancy is an obstacle for girls’ future education and job opportunities.11–13 Unmarried pregnant teenagers are affected by stigma, rejection, or violence by partners, parents, and peers.14,15 Girls who become pregnant before the age of 18 years are more likely to experience violence within a marriage or partnership.15 Babies of teenagers face higher risks of low birth weight, preterm delivery, and severe neonatal conditions.10
As evidenced by different studies there are factors associated with teenage pregnancy which include; age,16–19 marital status,17–21 educational status,17,22,23 employment,17,19,24 residence,16,17,25 occupation,17,26 wealth status,13,26,27 culture,19,28 peer pressure,13,29 family history of teenage pregnancies,18,30 early marriage,31 forced marriage,27 rape,32 community contraceptive use,24 and community wealth status.22,–23,–33
Since reducing the high rate of teenage pregnancy and maternal mortality is one the key Sustainable Development Goals (SDG), target 3.1 and 3.7, it has been addressed by the Ethiopian government and other key development partners.34 For instance, the Ethiopian Federal Ministry of Health (FMOH) developed different strategies and set outcome targets to reduce the rate of teenage pregnancy from 12% to 3%.35,36 Despite the efforts made, teenage pregnancy remains high in Ethiopia.7,16
Studies done previously were local and focused on only individual-level factors based on the assumption of independence of individual observations by ignoring cluster effect. However, individual observations have some degree of correlation within a cluster they belong to. Thus, ignoring the effect of community-level factors leads to a false conclusion. Moreover, previous studies used a small sample size which can also lead to bias in conclusion. Therefore, this study aimed to assess individual- and community-level factors affecting teenage pregnancy using a two-level mixed-effects logistic regression model.
Methods
Study Area, Setting
The study was conducted in Ethiopia, which is one of the Sub-Saharan African countries. It is found in the North-Eastern part of Africa, lies between 3° and 15° North latitude and 33° and 48° East longitude.37 It has a total estimated 114,530,078 population. Females’ age 15–19 years old are estimated to total 6.3 million.38 Ethiopia is one of the poorest counties, with a gross domestic product (GDP) per capita income of US$772. Nearly one-fourth of the populations of Ethiopia are living below the national poverty line.39 Though Ethiopia is making the fastest progress in ensuring access to education in SSA, it still faces challenges; low primary completion rates, a fall in enrollment rates in secondary education (30.7%), and low-quality education at all levels.40
This study was an in-depth secondary analysis of the 2016 EDHS. The EDHS has been conducted every 5 years to provide health and health-related indicators in Ethiopia. The 2016 EDHS is the latest national survey conducted in nine regional states and two administrative cities. The regions include Tigray, Afar, Amhara, Oromia, Somali, Benishangul-Gumuz, Southern Nations, Nationalities and Peoples’ Region (SNNPR), (Gambella, and Harari. Administrative cities include Addis Ababa and Dire Dawa). Administratively, regions in Ethiopia are divided into Zones, and Zones into administrative units called Woredas. Each Woreda is further subdivided into the lowest administrative unit, called Kebeles. During the 2007 census, each Kebele was subdivided into census enumeration areas (EAs), which were convenient for the implementation of the census.7
Study Design and Sampling
The 2016 EDHS was cross-sectional by design. The 2016 EDHS sample was stratified and selected in two stages. In the first stage, stratification was conducted by region and then in each region stratified as urban and rural, yielding 21 sampling strata. A total of 645 EAs (202 in urban areas and 443 in rural areas) were selected with probability proportional to EA size in each sampling stratum. In the second stage, a fixed number of 28 households per cluster were with an equal probability systematic selection from the newly created household listing.
Variable Measurement
The outcome variable was dichotomized as teenage pregnancy (yes/no). A woman was considered as experiencing teenage pregnancy if her age was from 15–19 and if she had ever been pregnant before or during the survey. Regarding media exposure, a woman was considered as having media exposure if she listened to both radio and television at least once a week. The variable wealth index was re-categorized as “Poor”, “Middle”, and “Rich” categories by merging poorest with poorer and richest with richer.25 Community-level variables were computed by aggregating the individual women characteristics into clusters. Then the proportion was calculated by dividing subcategories to the total. Distributions of the proportion of aggregate variables were checked using the Shapiro–Wilk normality test and were not normally distributed. Therefore, these aggregate variables were categorized using the median value. A total of eight community variables were generated. Family disruption was created using the proportion of female-headed houses in their cluster.33 Community educational status was computed based on the proportion of below secondary educational status in their cluster. Community wealth status was computed using the proportion of poor wealth index in each cluster. Community-level literacy was calculated based on the proportion illiterate in each cluster; the same is true for other community-level variables.25
Data Processing and Analysis
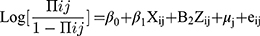
Data were cleaned to check its consistency and missing values. Descriptive statistics such as frequencies, median, and percentages were computed. The data were analyzed using Stata version 14.0. Sampling weights were done to compensate for the non-proportional allocation of the sample to strata as well as for non-responses. The EDHS data are hierarchical, ie, individuals were nested within communities, and Intra-class Correlation Coefficient (ICC) was greater than 10% (ICC=34%). Therefore, a two-level mixed-effects logistic regression model was conducted to estimate both independent (fixed) effects of the explanatory variables and community-level random effects on teenage pregnancy. The log of the probability of being pregnant at teenage was modelled using a two-level multilevel model as follows;41
Where, πij is the probability of being pregnant for the ith teenager in the jth community; 1-πij is the probability of being a non-pregnant teenager; i and j are the level 1 (individual) and level 2 (community) units, respectively; X and Z refer to individual- and community-level variables, respectively; the β’s are the fixed coefficients –therefore, for every one-unit increase in X/Z there is a corresponding effect on the probability of being pregnant as a teenager. Whereas, β0 is the intercept – the effect on the probability of being pregnant as a teenager in the absence of influence of predictors; and uj shows the random effect (effect of the community on a teenager to become pregnant) for the jth community and eij showed random errors at the individual levels. By assuming each community had a different intercept (β0) and fixed coefficient (β), the clustered data nature and the within and between community variations were taken into account.
In the analysis first, bivariable multilevel logistic regression was computed and variables with a P-value less than 0.3 were included in multivariable multilevel logistic regression. Four models were displayed in this analysis, Model 0 (model containing no factors), Model 1 (containing only individual factors), Model 2 (containing only community factors), and Model 3 (both individual- and community-level factors). Variables with a P-value of less than 0.05 had a statistically significant association with the outcome variable. The result of the fixed effect was presented as Adjusted Odds Ratio (AOR) with their 95% confidence interval (95% CI).
The measures of variation (random-effects) were reported using ICC, a proportional change in variance (PCV), and Median Odds Ratio (MOR). The ICC was used to show how much the observation within one cluster resembled each other, and MOR is a measure of unexplained cluster heterogeneity. The ICC was computed using this formula as follows: [ ],
],  where is the estimated variance of clusters. MOR is the median value of the odds ratio between the area at highest risk and the area at the lowest risk when randomly picking out two areas and calculated using the formula [
where is the estimated variance of clusters. MOR is the median value of the odds ratio between the area at highest risk and the area at the lowest risk when randomly picking out two areas and calculated using the formula [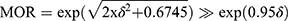 ]. The proportional change in variance (PCV) signifies the total variation attributed by individual-level factors and area-level factors in the multilevel model. Standard error at the cut-off point of ±2 was used to check multicollinearity and there was no multicollinearity. The goodness of fit of the model was checked by the log-likelihood test.
]. The proportional change in variance (PCV) signifies the total variation attributed by individual-level factors and area-level factors in the multilevel model. Standard error at the cut-off point of ±2 was used to check multicollinearity and there was no multicollinearity. The goodness of fit of the model was checked by the log-likelihood test.
Ethical Approval
The EDHS Dataset
An authorization letter was also obtained from CSA for downloading the EDHS data set by requesting the website www.measuredhs.com. Ethical clearance for the primary study (EDHS 2016) was obtained from Ethiopia Health and Nutrition Research Institute Review Board, the Ministry of Science and Technology, Institutional Review Board of ICF International, and the Centers of Disease Control and Prevention (CDC). The accessed data were used for the registered research only. All data were treated as confidential and no effort was made to identify any household or individual respondent interviewed in the survey. The detailed information on methodology and the ethical issue was published in the EDHS report.
Results
Individual-Level Characteristics of Respondents
A total of 3381 women aged 15–19 years were included for analysis. The mean (±SD) age of respondents was 16.9±1.34 years. Five hundred and eighty-eight (17.38%) were married. The mean age (±SD) at first marriage was 15.5±1.7 years. Looking at education, 468 (13.84%) teenagers were not educated. Only 254 (7.5%) teenagers were using contraceptive methods (Table 1).
 |
Table 1 Individual-Level Characteristics of Teenagers, EDHS 2016 (n=3381) |
Community-Level Characteristics of Respondents
More than three-quarters (76.19%) of teenagers were from rural areas. Nearly half (45.1%) of teenagers were from communities with a high proportion of illiteracy. Out of the total respondents, 2172 (64.24%) were from communities with a higher proportion of poor. Nearly two-thirds (64.71%) of teenagers were from communities with a higher proportion of contraceptive non-use (Table 2).
 |
Table 2 Community-Level Characteristics of Teenagers, EDHS 2016 (n=3381) |
Individual- and Community-Level Factors for Teenage Pregnancy
In the final model; age, educational status, marital status, and community wealth status had a statistical association with teenage pregnancy. The odds of experiencing teenage pregnancy among 17 year olds was 9.3-times higher than 15 year olds (AOR=9.26, 95% CI=2.67–32.04). The odds of experiencing teenage pregnancy among 18 yearolds was 9.5-times higher than 15 year olds (AOR=9.53, 95% CI=2.97–30.04). The odds of experiencing teenage pregnancy among 19 year olds was 20-times higher than 15 year olds (AOR=20.01, 95% CI=5.94–67.39).
The odds of experiencing teenage pregnancy among uneducated teenagers was 3.8-times higher compared with secondary or above-educated teenagers (AOR=3.83, 95% CI=1.05–14.00). The odds of experiencing teenage pregnancy among primary level educated teenagers was 3.3-times higher compared with secondary and above-educated teenagers (AOR=3.34, 95% CI=1.01–11.08).
Married teenagers had higher odds of experiencing teenage pregnancy than single teenagers (AOR=70.12, 95% CI=27.55–178.4). The odds of experiencing teenage pregnancy among teenagers who live in communities with a higher proportion of poor were 3.9-times higher compared with teenagers who live in communities with a lower proportion of poor (AOR=3.86, 95% CI=1.80–8.26) (Table 3).
 |
Table 3 Individual- and Community-Level Factors Associated with Teenage Pregnancy, EDHS 2016 (n=3381) |
Random Effects (Measures of Variation)
The value of ICC in the null model was 34%. This implies that 34% of the variation in the level of teenage pregnancy was due to community-level factors. After considering both individual- and community-level factors, ICC was reduced to 28%. The value of PCV was 24%, which is high. This showed that 24% of the community-level variation on teenage pregnancy was explained by the combined factors at both the individual and community levels (Table 4).
 |
Table 4 Measure of Variation for Teenage Pregnancy at Cluster Level by Multilevel Logistic Regression Analysis, EDHS 2016 |
Discussion
This study attempted to identify individual- and community-level factors affecting teenage pregnancy. Age, educational status, marital status, and community wealth status were significant predictors of teenage pregnancy. Seventeen years old and above teenagers had higher odds of experiencing teenage pregnancy than 15 year olds . This is similar to other studies done in Ethiopia16–18 and Nigeria.19 This is due to the fact that as age increases the probability of being sexually active and getting married will be increased. As a result, the chance of getting pregnant and childbirth will also increase.
The odds of experiencing teenage pregnancy among primary and below-educated teenagers were higher than secondary and above-educated teenagers. This finding is supported by studies done in Ethiopia,17 Nigeria,19 Philippines,22 and Japan.23 This may be due to educated adolescents have better knowledge and skills to prevent pregnancy. However, the primary level and uneducated adolescents have limited access to sexual and reproductive health information and services needed to prevent pregnancy. Furthermore, higher-level educated females were more likely to get married at a latter age. They also become confident enough to reject early marriage and sexual abuse.
The odds of experiencing teenage pregnancy among married teenagers were higher than single teenagers. This finding is in line with studies conducted in Ethiopia,17,18,20 Nigeria,19 and Uganda.21 This could be due to the fact that married teenagers became sexually active without knowledge and access for family planning methods and the likelihood of being pregnant will be increased. There is also low family planning utilization (7.5%), and a high unmet need for family planning (22.5%) among adolescent girls. On the contrary to national and international laws that prohibit early marriage, it is one of the most common harmful traditional practices in Ethiopia. According to EDHS 2016, nearly half (47%) of women were married before the age of 18 years.7 This huge magnitude indicates how much fighting early marriage is needed to prevent teenage pregnancy and other sexual and reproductive health problems. The finding of this study suggested that investment in ending child marriage is crucial to reduce teenage pregnancy and its complications. Thus, adherence to the available legal frameworks against child marriage and law enforcement to protect the sexual and reproductive health and human rights of adolescent girls is essential to end child marriage and teenage pregnancy.
Teenagers who live in communities with a higher proportion of poor had higher odds of experiencing teenage pregnancy than teenagers who live in communities with a lower proportion of poor. This is consistent with other studies in SSA33 and Philippines.22 This might be due to teenagers who live in communities with poor wealth status have poor access to education and sexual and reproductive health services including family planning. They are also faced with the problem of early marriage, school dropout, and risky work, ie, commercial sex work. All these reasons make teenagers vulnerable for teenage pregnancy.
The strength of this study is the use of multilevel modelling, and the most recent nationally representative survey. However, the study used secondary data which limits the variable used in the analysis. For instance, EDHS data has no information on family control, parent–children discussion on sexual matters, and cultural practices. Moreover, the data used in this study was cross-sectional, it is impossible to establish causality.
Conclusion
Age, educational status, and marital status from individual-level factors and community wealth status from community-level factors were predictors of teenage pregnancy. The government should strive to improve female education. The government and other concerned bodies should also strive to decrease early marriage and sexual initiation. Moreover, especial attention should be given to the poor population to improve their living conditions and wellbeing.
Abbreviations
CSA, Central Statistical Agency; CDC, Centers of Disease Control and Prevention; EDHS, Ethiopia Demographic and Health Survey; EAs, Enumeration Areas; FMOH, Federal Ministry of Health; GDP, Gross Domestic Product; ICC, Intracluster Correlation Coefficient; MOR, Median Odds Ratio; PCV, Proportional Change in Variance; SDG, Sustainable Development Goals; SSA, Sub-Saharan Africa.
Acknowledgment
We would like to express my deepest gratitude to the Central Statistical Agency of Ethiopia for giving the EDHS dataset and authorizing me to conduct the research.
Disclosure
The authors declare that they have no conflicts of interest for this work.
References
1. International Planned Parenthood Federation (IPPF). Understanding Adolescents, in an IPPF Report on Young People’s Sexual and Reproductive Health Needs. London; 1994. Available from http://www.plannedparenthood.org.
2. United Nations. Department of Economic and Social Affairs, Population Division (2019). World Population Prospects; 2019.
3. Programme for Adolescent’s Health and Development of WHO/UNFPA/UNICEF Study Group on Programming for Adolescent Health. Geneva; 1999: 11. Available from: https://www.who.int/maternal_child_adolescent/documents/trs_886/en/.
4. Darroch J, Woog V, Bankola A, Ashford L. Adding It Up: Costs and Benefits of Meeting the Contraceptive Needs of Adolescents. New York: Guttmacher Institute; 2016. Available from: https://www.guttmacher.org/report/adding-it-meeting-contraceptive-needs-of-adolescents.
5. Kassa GM, Arowojolu AO, Odukogbe AA, Yalew AW. Prevalence and determinants of adolescent pregnancy in Africa: a systematic review and Meta-analysis. Reprod Health. 2018;15(1):195. doi:10.1186/s12978-018-0640-2
6. Central Statistical Authority/ Ethiopia,ORC Macro. Ethiopia Demographic and Health Survey 2000. Addis Ababa: Central Statistical Authority/Ethiopia and ORC Macro; 2001.
7. Central Statistical Agency Addis Ababa Ethiopia. Demographic and Health Survey 2016. Federal Democratic Republic of Ethiopia; 2017.
8. Kassa GM, Arowojolu AO, Odukogbe AA, Yalew AW. Trends and determinants of teenage childbearing in Ethiopia: evidence from the 2000 to 2016demographic and health surveys. Ital J Pediatr. 2019;45(1):153. doi:10.1186/s13052-019-0745-4
9. Global Health Estimates 2015: Deaths by Cause, Age, Sex, by Country and by Region, 2000-2015. Geneva: World Health Organization; 2016. Available from: https://www.who.int/healthinfo/global_burden_disease/estimates/en/index1.html.
10. Ganchimeg T, Ota E, Morisaki N, et al. Pregnancy and childbirth outcomes among adolescent mothers: world Health Organization multi country study. BJOG. 2014;121(Suppl 3):18–40. doi:10.1111/1471-0528.12630
11. Merrick T. Making the Case for Investing in Adolescent Reproductive Health: A Review of Evidence and PopPov Research Contributions. Washington DC: Population and Poverty Research Institute and Population Reference Bureau; 2015. Available from: https://www.prb.org/poppov-adolescent-sexual-reprohealth/.
12. Undiyaundeye FA, Agba AA, Mandeun T. The effect of teenage pregnancy on the girl-child in Nigerian society. Int J Multidiscipl Thought. 2015;5(4):283–289.
13. Gyan C. The effects of teenage pregnancy on the educational attainment of girls at Chorkor, a Suburb of Accra. J Educ Soc Res. 2013;3(3):53. doi:10.5901/jesr.2013.v4n3p53
14. Girlhood Not Motherhood: Preventing Adolescent Pregnancy. New York: UNFPA; 2015. Available from: https://www.unfpa.org/publications/girlhood-not-motherhood.
15. Adolescent Pregnancy: A Review of the Evidence. New York: United Nations Population Fund; 2013. Available from: https://www.unfpa.org/publications/adolescent-pregnancy.
16. Habitu YA, Yalew A, Bisetegn TA. Prevalence and factors associated with teenage pregnancy, Northeast Ethiopia: a cross-sectional study. J Pregnancy. 2018. doi:10.1155/2018/1714527
17. Alemayehu T, Haider J, Habte D. Determinants of adolescent fertility in Ethiopia. Ethiop J Health Devel. 2010;24(1):30–38. doi:10.4314/ejhd.v24i1.62942
18. Ayele BG, Gebregzabher TG, Hailu TT, Assefa BA. Determinants of teenage pregnancy in Degua Tembien District, Tigray, Northern Ethiopia: a community-based case- control study. PLoS One. 2018;13:7. doi:10.1371/journal.pone.0200898
19. Nwosu UM. Contemporary factors of teenage pregnancy in rural communities of Abia state, Nigeria. Int J Commun Med Public Health. 2017;4(2):588–592. doi:10.18203/2394-6040.ijcmph20170295
20. Assefa B, Abiyou M, Yeneneh G, Hiruye A, Mariam DH, Derbew M. Assessment of the magnitude of teenage pregnancy and its associated factors among teenage females visiting Assosa General Hospital. Ethiop Med J. 2015;Supp. 2:25–37.
21. Gideon R. Factors associated with adolescent pregnancy and fertility in Uganda: analysis of the 2011 demographic and health survey data. Soc Sci J. 2013;3(2):30–35. doi:10.5923/j.sociology.20130302.03
22. Habito CM, Vaughan C, Morgan A. Adolescent sexual initiation and pregnancy: what more can be learned through further analysis of the demographic and health surveys in the Philippines. BMC Public Health. 2019;19:1142. doi:10.1186/s12889-019-7451-4
23. Baba S, Iso H, Fujiwara T. Area- level and individual-level factors for teenage motherhood: a multilevel analysis in Japan. PLoS One. 2016;11:11. doi:10.1371/journal.pone.0166345
24. Ezegwui HU, Ikeako LC, Ogbuefi F. Obstetric outcome of teenage pregnancies at a tertiary hospital in Enugu, Nigeria. Nigerian J Clin Pract. 2012. 15(2):147–150. doi:10.4103/1119-3077.97289
25. Birhanu BE, Kebede DL, Kahsay AB, Belachew AB. Predictors of teenage pregnancy in Ethiopia: a multilevel analysis. BMC Public Health. 2019;19:601. doi:10.1186/s12889-019-6845-7
26. Amoran OE. A comparative analysis of predictors of teenage pregnancy and its prevention in a rural town in Western Nigeria. Int J Equity Health. 2012;11(1):37. doi:10.1186/1475-9276-11-37
27. UNFPA.Motherhood in Childhood, Facing the Challenge of Adolescent Pregnancy, State of World Population. UNFPA; 2013. Available from: https://www.unfpa.org/publications/state-world-population-2013.
28. Mchunu G, Peltzer K, Tutshana B, Seutlwadi L. Adolescent pregnancy and associated factors in South Africa youth. Afr Health Sci. 2012;12(4):426–434. doi:http://dx.doi.10.4314/ahs.v12i4.5
29. Vincent G, Alemu FM. Factors contributing to, and effects of, teenage pregnancy in Juba. South Sudan Med J. 2016;9(2):28–31.
30. Wieler EW, Roos LL, Nickel NC. Teenage pregnancy: the impact of maternal adolescent childbearing and older sister’s teenage pregnancy on a younger sister. BMC Pregnancy Childbirth. 2016;16(1):120. doi:10.1186/s12884-016-0911-2
31. Presler-Marshall E, Jones N Charting the future: empowering girls to prevent early pregnancy; 2012. Available from: https://www.odi.org/publications/6689-charting-future-empowering-girls-prevent-early-pregnancy.
32. Tiruneh YZ Teenage pregnancy and motherhood in merkato slums in Ethiopia: perspectives of teenagers and implications for sexual and reproductive health polices and services unpublished thesis; 2010.
33. Odimegwu C, Mkwananzi S. Factors associated with teen pregnancy in sub-Saharan Africa: A multi-country cross-sectional study. Afr J Reprod Health. 2016;20(3):94. doi:10.29063/ajrh2016/v20i3.14
34. United Nations General Assembly. Resolution adopted by the general assembly on. Transforming Our World: The 2030 Agenda for Sustainable Development. New York: United Nations; 2015; 2015 September 25.
35. Federal Democratic Republic of Ethiopia Ministry of Health. National Adolescent and Youth Reproductive Health Strategy: 2016–2020.
36. Federal Democratic Republic of Ethiopia Ministry of Health. National Reproductive Health Strategy: 2016–2020.
37. Commission PC. The 2007 population and housing census of Ethiopia. Available from: http://www.csa.gov.et/census-report/complete-report/census–2007.
38. Ethiopian Population-World meter; 2020. Available from: https://www.worldometers.info/world-population/ethiopia-population/.
39. Current US$. 2018. Available from: https://data.worldbank.org/indicator/NY.GDP.PCAP.CD.
40. GEM Report. Available from: https://gemreportunesco.wordpress.com/2019/07/12/ethiopia-is-making-the-fastest-progress-in-primary-completion-in-sub-saharan-africa-how/.
41. Hox J, Moerbeek M, van de Schoot R. Multilevel Analysis: Techniques and Applications, Third Edition (Quantitative Methodology Series). New York: Routledge; 2018.
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.