Back to Journals » Neuropsychiatric Disease and Treatment » Volume 10
A multidimensional risk factor model for suicide attempts in later life
Authors Chan S, Chiu F, Lam C , Wong S, Conwell Y
Received 25 June 2014
Accepted for publication 30 July 2014
Published 18 September 2014 Volume 2014:10 Pages 1807—1817
DOI https://doi.org/10.2147/NDT.S70011
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Roger Pinder
Sau Man Sandra Chan,1 Fung Kum Helen Chiu,1 Chiu Wa Linda Lam,1 Sau Man Corine Wong,1 Yeates Conwell2
1Department of Psychiatry, The Chinese University of Hong Kong, Hong Kong, People’s Republic of China; 2Department of Psychiatry, University of Rochester, Rochester, NY, USA
Background: Elderly suicide is a public health problem worldwide, and the risk factors are multidimensional. Chronic mental health problems, personality traits, stressful life events, comorbid medical conditions, social isolation, unemployment, and poverty are associated with higher risk for suicide in later life. There was a relative paucity of data on the neurobiological markers of elderly suicide.
Objective: This study examines the conjoint roles of cerebrovascular risk factors (CVRFs) and other established biopsychosocial risk factors in older adults who had made a recent suicide attempt.
Design: A cross-sectional, case-controlled study.
Setting: A tertiary care setting in a public sector and a community setting.
Subjects and methods: Cases (N=77) were nondemented Chinese adults aged ≥65 years, enrolled in a regional psychogeriatric service following a suicide attempt; comparison subjects (N=99) were community-dwelling nondemented older adults with no lifetime history of suicide. Measures of sociodemographic profile, life events, suicidal behavior, Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) Axis I psychopathology, personality traits, functional status, physical health, CVRFs, and executive cognitive functions were administered.
Results: Weighted sum of CVRF score was significantly higher in older women who had made a recent suicide attempt (mean: 10.56; standard deviation [SD]: 5.46) than comparison subjects (mean: 7.24; SD: 4.04) (t=3.52, P=0.001; df=99). Logistic regression showed that CVRF score (Exp[B]: 1.289, P=0.033), DSM-IV depressive disorders (current) (Exp[B]: 348, P<0.001), number of life events in the past 12 weeks (Exp[B]: 10.4; P<0.001), and being married (Exp[B]: 12.2, P<0.048) significantly increased odds for suicide attempt status in older women (Nagelkerke R2: 0.844). Association of CVRF score and suicide attempt status was not observed in older men for whom number of life events in the past 12 weeks (Exp[B]: 9.164; P<0.001), higher neuroticism (Exp[B]: 1.028; P=0.048), and impaired performance on a Modified Card Sorting Test (Exp[B]: 0.646; P=0.032) significantly increased odds for suicide attempt status in a logistic regression model (Nagelkerke R2: 0.611).
Conclusion: Risk factors for cerebrovascular diseases may be associated with higher risk for attempted suicide in older women, but not in older men. Older men and women have distinct risk factor profiles that may inform targeted intervention and prevention strategies.
Keywords: chronic medical illness, cognitive function, suicide, later life
Introduction
Suicide is an adverse clinical outcome driven by complex biopsychosocial risk factors.1 According to the World Health Organization, older adults, being the fastest-growing population segment worldwide, are at greater risk for suicide than any other age group.2,3 Retrospective studies, as well as few prospective ones, have identified chronic mental health problems as risk factors associated with suicide, with particular emphasis on affective disorders, including depression and bipolar disorders, on top of personality traits, stressful life events, comorbid medical conditions, social isolation, unemployment, and poverty.4–6 In the US, the Centers for Disease Control and Prevention regards the state of mental health as the main public health issue related to aging, as the presence of mental health problems such as depression often adversely affects the course and complicates the treatment of other chronic illness.7
While there was a relative paucity of data on the neurobiological markers of elderly suicide, studies on suicide in a nonelder population allude to biological vulnerability factors such as reduced serotonergic modulation and higher stress sensitivity, impaired decision making, and other cognitive impairments.8–10 More recent studies reported on the role of noncoding microribonucleic acid in moderating or mediating synaptic plasticity, stress reactions, serotoninergic function, and major affective disorders, but little is yet known of the direct role of microribonucleic acid in mediating risk for suicide.11 Some case-controlled studies into neurobiological factors associated with late-life depression have suggested important roles of cerebrovascular risk factors (CVRFs).12–15 Vascular pathologies in the brain may also manifest at subsyndromal level in the absence of diagnosable mental illness, given the fact that nondemented older adults with magnetic resonance imaging of subcortical white matter ischemic lesions (manifest as hyperintense signals) or a higher level of clinical CVRFs had more impaired executive cognitive functions.16–22 Among the scarce number of studies, elderly suicide attempters with diagnosable depressive disorder showed more subcortical gray matter hyperintensities with a trend toward having more periventricular signals.23 None of those studies has directly examined the role of vascular risk factors in the presence of other biopsychosocial risk factors for later-life suicide.
Our group reported significantly higher weighted sum of age-adjusted CVRF scores (calculated from American Heart Association [AHA] criteria) in suicide cases than community-dwelling comparison subjects in a community psychological autopsy study of nondemented subjects aged ≥50 years in Monroe County, Rochester, NY, USA.24 The association remained statistically significant after accounting for age, sex, depression diagnosis, and functional status.24 This observation suggests that the risks conferred by CVRFs on later-life completed suicides are not adequately explained by the presence of depressive disorders. It could well be possible that the presence of subsyndromal impairment such as aberrant executive cognitive function or trait impulsivity25–27 may explain partly the relationship between CVRFs and later-life suicide. Such a hypothesis, however, cannot be tested in a psychological autopsy that utilizes exclusively proxy data. Among older adults, there are between two and four suicide attempts for every completed suicide compared with estimates of 8:1 and 20:1 in younger people.28 Older adults are more determined in their efforts to die by suicide.29 Clinical characteristics of older adults who attempt suicide are also remarkably similar to those who die by suicide.30–32 For these reasons, studies of older adults who attempt suicide may provide important information about those likely to complete suicide.
The primary objective of this study, based on previous data, is to test whether CVRFs increase risk for suicide attempts in later life. Further, as a secondary objective, we would like to examine the roles of executive cognitive dysfunction and trait impulsivity in the association of CVRFs with later-life suicide attempts (if any). We thus hypothesize 1) that the sum of CVRFs will be significantly greater in nondemented older adult suicide attempters than in nondemented older adult comparison participants; 2) that a higher sum of CVRFs will be associated with higher risk for suicide attempts after accounting for the effects of age, sex, depressive disorders, and other biopsychosocial risk factors of late-life suicide; and 3) that the association of a higher sum of CVRFs with higher risk for suicide attempts is moderated by impaired executive cognitive function and/or trait impulsivity.
Methods
Design
This was a cross-sectional, case-controlled study.
Subjects, sampling, and enrollment procedure
All suicide attempters were recruited from a regional division of a government-funded Elderly Suicide Prevention Program (ESPP), which is a care management program delivered through multidisciplinary old-age psychiatry teams based in the public sector of hospital services. This regional division of ESPP serves a population of 1.2 million (constituting 20% of the whole population) in the New Territories East District of Hong Kong, People’s Republic of China.33 This program provides expedited service for older adults with suicide ideation, depression, and recent suicide attempts. Eligible participants for this study included only Chinese older adults (aged ≥65 years) who had made a recent suicide attempt and were enrolled in the ESPP during the study period (40 months from the last quarter of 2005 to the first quarter of 2009). Subjects who could not communicate in the Cantonese dialect or those with a diagnosis of clinical dementia were excluded from this study. The key enrollment step involved ESPP case managers who identified eligible cases and referred them to the research team.
Comparison subjects aged ≥65 years and with no lifetime history of suicide attempt were purposively recruited from residential facilities and activity centers for older adults in the same geographical area. The enrollment of comparison subjects was paced with the consecutive enrollment of suicide attempters to the ESPP. In the original research design, it was intended to match each suicide attempter and comparison subject by age (±5 years) and sex. The wide age range adopted was consistent with the prior psychoautopsy studies carried out by our group.24,34 Comparison subjects were assessed as soon as possible after enrollment and, often for practical reasons, much earlier than their counterparts from the ESPP for whom the research interviews were deferred for variable periods of time due to health reasons.
Choice of general population comparison subjects was favored over a well-matched clinical comparison group (such as depressed nonattempters), as our study aimed to identify general risk factors rather than protective factors.32 Given the fact that only 50% of suicide decedents in the previous psychoautopsy on Chinese older adults in Hong Kong had diagnosable major depressive disorder, including dysthymia and adjustment disorder,34 depressed nonattempters are thus not comparable with the attempters group with heterogeneous psychiatric diagnoses. Furthermore, the exclusive use of depressed nonattempters as comparison subjects may preclude the examination of moderational or mediational effects of depressive disorders, based on what has been known of the association of late-life depressive disorders with vascular factors.15
All subjects gave written informed consent. The research protocol was reviewed and approved by the local institutional review board (The Joint Chinese University of Hong Kong – New Territories East Cluster Clinical Research Ethics Committee CRE-2004.103-T).
Data collection
Research interviews with the older adults who had made a recent suicide attempt were conducted in the research clinic. Subjects hospitalized for medically significant clinical problems or psychiatric conditions were interviewed until they were discharged from hospital and had adequately recovered from the medical or associated psychiatric condition related to the index suicide attempt. Comparison subjects were interviewed at either the residential facilities or community centers through which they were recruited. Consents were also sought from all subjects to review their electronic clinical database. Research interviews normally took 1.5–2 hours and were conducted by two senior research associates who had postgraduate degrees in social work and psychology, respectively, were trained in the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) Structured Clinical Interview for DSM-IV Axis I (SCID-I) disorders rating, and had been working in this field for >3 years prior to this study. The following domains were assessed.
Demographics and social circumstances
Sex, age, educational level, marital status, living conditions, and income were charted. Significant life events in the past 12 weeks before the research interview (among comparison subjects) or within 12 weeks prior to the index suicide attempt (among suicide attempters) were charted using an adapted Paykal’s life event checklist that was used in previous psychoautopsy studies on Hong Kong Chinese older adults.31,34
Suicidal behavior
We noted the method(s) and time of the index suicide attempt, as well as the lifetime history of suicide attempts. The level of intent of the index suicide attempt was measured with Beck’s Suicide Intent Scale,35 and the potential lethality of the actual attempt was characterized by the Medical Lethality Scale.36
Psychopathology and personality traits
Current and lifetime DSM-IV Axis I psychiatric diagnoses were established using the SCID-DSM-IV Chinese version. The SCID-DSM-IV Chinese version has shown good reliability and validity in Hong Kong Chinese.37,38 An all-source approach (taking into account clinical information entries available from the electronic clinical database and the clinical notes of case managers) was adopted to arrive at consensus SCID-I diagnosis at research meetings led by the first author (a research psychiatrist).
The NEO Five Factor Inventory (60-item five-point Likert scale, Chinese version), originated from a standardized multitrait measurement tool derived from the five-factor model of personality (neuroticism, extraversion, openness, agreeableness, and conscientiousness), was used to characterize personality traits.39,40 Separate questions on the anger-hostility facet and impulsiveness facet were abstracted from the full version of the Revised NEO Personality Inventory.40
Cognitive functions
All subjects were tested with a brief eleven-item bedside global cognitive test, namely the Cantonese version of the Mini-Mental State Examination (C-MMSE),41 and a Modified Wisconsin Card Sorting Test on frontal executive function.42–44
General physical health status
Based on the categorical physical diagnoses endorsed by the subjects and verified from the clinical database, overall and systematic physical health burden was rated by the research psychiatrist (first author) using the Cumulative Illness Rating Scale (CIRS),45 which gives summary scores of physical illness burden in 13 different body systems by taking into account both number and severity of categorical physical diseases. Subjects’ basic self-care abilities were rated using the Physical Self-Maintenance Scale (PSMS).46
CVRFs
CVRFs were quantified as a weighted sum of severities of specific CVRFs (age, systolic blood pressure, antihypertensive treatment, coronary vessel disease, diabetes mellitus, hypertension, atrial fibrillation, left-ventricular hypertrophy, and cigarette smoking) based on the AHA criteria for risk factors for stroke.47
Statistical analysis
Statistical analyses were conducted with SPSS software (version 20.0). Since the suicide attempters and comparison subjects were matched by age (±5 years), CVRFs used for statistical analysis were adjusted by subtracting the age subscore from the total score to yield the age-adjusted CVRFs in order to avoid overadjustment.24,48
Sample size estimation
With reference to hypothesis 1, we base our sample size calculation on a prior study conducted in Monroe County, Rochester, NY, USA, where the mean weighted sums of CVRF scores by the AHA criteria were compared in cases and comparison subjects.24 The estimated minimum sample size to demonstrate statistically significant difference in the mean weighted sum of AHA CVRFs between cases and controls is a minimum of 60 in each group. At the planning stage, we set the target sample size as 100 cases and 100 comparison subjects in order to optimize the power to test the main hypothesis. It was estimated from past service statistics that the planned sample size, if reached, may involve nearly all eligible suicide attempters served in this regional ESPP team during the study period.
Results
During the 40-month study period, the case managers identified 100 suicide attempters (40 men and 60 women) who were consecutively enrolled in the ESPP. The potentially eligible subjects were all referred to the research team. The median time lag between index attempt and research assessment was 14 weeks (range 1–45 weeks) and all interviews took place in an outpatient setting when the subjects had adequately recovered from the medical consequences of the index attempt and the associated mental health condition. At the first research assessment, 23 (six men, 17 women) suicide attempters were excluded due to clinical diagnosis of dementia. The mean age and C-MMSE score of excluded suicide attempters were 85.6 years (standard deviation [SD]: 7.3) and 13.7 (SD: 2.5), respectively, while the mean age of included suicide attempters without dementia (N=77) was 75.6 years (SD: 7.2) and the mean C-MMSE score was 24.3 (SD: 3.5). Fifteen (8.5%) of the included cases had a history of a previous suicide attempt. Methods used in the index suicide attempt were self-laceration (six cases, 7.8%), drug overdose and ingestion of toxic nonmedicinal chemicals (34 cases, 44.2%), jumping from height (18 cases, 23.4%), hanging (eleven cases, 14.3%), drowning (one case, 0.6%), and inhalation of toxic gas (seven cases, 9%). The mean score on Suicide Intent Scale was 3.4 (SD: 2.2). The median score on the Medical Lethality Index was 1 (mean: 1.5, SD: 0.75).
One hundred comparison subjects (40 men and 60 women) matched with the original 100 cases by age (±5 years) and sex were enrolled and interviewed. One comparison subject (a woman) was excluded from analysis due to a remote episode of lifetime suicide attempt that was not reported initially. The mean age of the remaining 99 comparison subjects was 77.2 years (SD: 7.6).
The included suicide attempters and comparison subjects were not significantly different in mean age (75 years vs 77 years, SD: 7.1 years, t=−1.28, P-value =0.202, df =174), sex ratio (proportion of females 55.8% vs 59%; chi-square: 0.133; P-value =0.76), and distribution of residential status (proportion living in residential facilities =26% vs 36%, chi-square: 2.57; P-value =0.144).
In initial data exploration, analysis of covariance was performed to examine the main effect (categorical membership of suicide attempt) and covariates (sex, age, current depressive disorder) on dependent variable (age-adjusted CVRF score). A significant suicide status by sex interaction was found (Type-III SS: 121, P-value =0.017). In view of the significant sex by suicide status interaction, a sex-stratified approach was adopted in subsequent data analyses.
Comparison of multidomain sociodemographic and clinical risk factor profile in older women with or without recent suicide attempt
Table 1 shows results of comparison across sociodemographic and other risk factors in older women. Five women in the comparison group (8.5%) had current major depressive disorder, all with age at onset >60 years. Of the women who had made a recent suicide attempt, 39 (90.7%) had a current major depressive disorder, all being late-onset cases (age at onset >60 years) and first timer diagnosis after the index attempt. The remaining older women who attempted suicide had adjustment disorder (N=3) and alcohol abuse (N=1). Significantly more older women who had made a recent suicide attempt were married, lived with others, and had current major depressive disorders, lifetime psychiatric disorder, and one or more past suicide attempts (excluding the current index attempt). In terms of physical health status, social stressor, personality traits, and cognitive functions, older women who had made a recent suicide attempt had a significantly higher score on CIRS and PSMS, a greater number of life events in the past 12 weeks, higher scores on the neuroticism factor of the NEO Five Factor Inventory and the impulsiveness facet of the Revised NEO Personality Inventory, fewer categories and a greater percentage of perseverative errors in a Modified Card Sorting Test, as well as a lower score on the C-MMSE.
Testing hypothesis 1, it was found that the weighted sum of age-adjusted CVRF score (age-adjusted CVRFs) was significantly higher among older women who had made a recent suicide attempt (mean: 10.56; SD: 5.46) than comparison subjects (mean: 7.24; SD: 4.04) (t=3.52, P=0.001, df=99). In a subgroup analysis, CVRF score was significantly higher in depressed women who had made suicide attempts than depressed comparison subjects.
Table 2 presents logistic regression models that tested whether age-adjusted CVRFs increased odds for suicide attempts after accounting for age, sex, depressive disorders, and other biopsychosocial risk factors of late-life suicide. A past suicide attempt was not included, as this had been deliberately excluded in comparison subjects. Final models were derived from backward Wald logistic regression. Bonferroni adjustment was used to minimize inflated likelihood of error in model building due to multiple comparisons. In our case, threshold P-value for entry into the model was adjusted by the number of simultaneous hypotheses tested in the simple t-tests and chi-square statistics. The threshold of P-value for entry was determined to be <0.002 for all variables after adjusting for multiple comparisons, with exceptions to “living alone” (P-value =0.042) and “being married” (P-value =0.035), as these factors were reported to be significantly associated with older adult suicide in a recent local psychoautopsy study.31,34
With reference to hypothesis 2, model 1 tested the effects of living alone, being married, life events in the past 12 weeks (abbreviated as LE-12), age-adjusted CVRFs, CIRS, PSMS, current major depressive disorder, and DSM-IV psychiatric diagnosis (lifetime) on the recent suicide attempts. Age-adjusted CVRFs (Exp[B]: 1.289, P=0.033), current major depressive disorder (Exp[B]: 348, P<0.001), LE-12 (Exp[B]: 10.4; P<0.001), and being married (Exp[B]: 12.86, P=0.047) were the predictors retained in the final model (Nagelkerke R2: 0.844).
In order to address the secondary objective (hypothesis 3), we considered the conceptual and strategic criteria of mediator and moderator variables defined in Baron and Kenny’s and MacArthur’s approaches.49 In initial data exploration we did not find significant correlation or association between age-adjusted CVRFs and the putative mediator variables, suggesting that the likelihood of mediatory effects of the putative variables (depression, measures of executive cognitive function, and trait impulsivity) is low. Also, the temporal relationship between the target variable (age-adjusted CVRF) and other putative mediator variables cannot be ascertained in a cross-sectional study design. We thus opted to test the interactional (moderator) model by examining whether age-adjusted CVRFs increase risk for suicide attempt through interaction with depression, impaired executive cognitive function, personality traits, or life events. Model 2 (in Table 2) included all predictor variables retained in model 1 plus variables from cognitive domains (number of category, percentage perseverative errors, and C-MMSE), as well as neuroticism and impulsiveness from the personality domain. The final reduced model yielded again age-adjusted CVRFs, current major depressive disorder, LE-12, and being married (Nagelkerke R2: 0.844). As cognitive function and trait impulsivity did not show any main effect, their interactions with age-adjusted CVRFs (hypothesis 3) were thus not tested.
Comparison of multidomain sociodemographic and clinical risk factor profile in older men with or without recent suicide attempt
Table 3 shows results of comparison across different domains in men. Older men in the comparison group were all free of current psychiatric diagnosis. Among the older men who had made a recent suicide attempt, 26 (76.4%) had a current DSM-IV Axis I psychiatric diagnosis of major depressive episode (age at onset >60 years in all cases) who received no prior treatment before the index attempt, two of whom had comorbid alcohol abuse or dependence. The remaining had diagnoses of alcohol dependence (N=1), schizophrenia (N=1), adjustment disorder (N=5), and psychosis not otherwise specified (N=1), respectively. Significantly more older men who had made a recent suicide attempt were married; had current major depressive disorder, lifetime psychiatric disorder, and a past history of suicide attempt prior to the index attempt; had more impaired function in physical self-maintenance; and had more physical illness burden. Age-adjusted CVRFs were not significantly different between older men who had made recent suicide attempts and comparison subjects (hypothesis 1). Hypotheses 2 and 3 were not tested in older men.
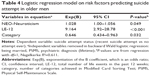
Table 4 shows the results of a logistic regression performed to examine the prediction of categorical membership (suicide attempt status) by including all sociodemographic, cognitive, and personality variables that were shown to have an association with suicide attempt status in univariate analyses. Age-adjusted CVRFs did not enter the regression, as there was no association shown in univariate analyses. Depressive disorder was not included, as there was no diagnosable current depression found in the comparison group. Likewise, past suicide attempt was not included, as this had been deliberately excluded in comparison subjects. The final model was derived from backward Wald logistic regression. Bonferroni adjustment was used to minimize inflated likelihood of error in model building due to multiple comparisons. The threshold P-value for model entry was set to be <0.002 with exceptions to being married (P-value =0.04) and psychiatric diagnosis (lifetime) (P-value =0.055) based on the reported effect on suicide risks in another local psychoautopsy study on older adults.31,34 The model thus tested the effects of being married, LE-12, PSMS, psychiatric diagnosis (lifetime), neuroticism, and number of category on the Modified Card Sorting Test (abbreviated as category) on the recent suicide attempts. LE-12 (Exp[B]: 9.164; P =<0.001), higher neuroticism (Exp[B]: 1.028; P=0.048), and category (Exp[B]: 0.646; P=0.032) were the independent variables retained in the final model (Nagelkerke R2: 0.611).
Discussion
Risk factor model for later-life suicide attempts: new understanding of the conjoint role of CVRFs in the context of other biopsychosocial risk factors
In a case-controlled study on older adults with recent suicide attempt conducted in 2001–2002 through the same old-age psychiatric service in Hong Kong before the establishment of the specialized case management program for elderly suicide prevention, the most significant independent factors associated with attempting suicide were a current diagnosis of major depression, followed by past suicide attempts, the presence of arthritic conditions, impaired function in activities of daily living, and a lower conscientiousness score on the NEO Five Factor Inventory. The prior study did not investigate the role of executive cognitive function and CVRFs. This study, recruiting elderly suicide attempters systematically identified through a similar social and clinical context, reconfirmed the outstanding roles of current depressive disorder and emerging life events in both men and women in the presence of other life challenges in aging, such as daily functional impairment, impaired executive cognitive function, and predisposed personality trait such as high neuroticism. In this clinical sample of older adults who had made recent suicide attempts, our study result supports the possible vulnerability of older women, but not older men, in developing the psychopathological outcome and self-harm acts in the presence of higher CVRF burden.
Before discussing the implications of the main findings, the following methodological limitations should be considered. First, despite the fact that all eligible suicide attempters enrolled for the suicide prevention program during the study period were recruited, the degree of sampling bias cannot be ascertained, as suicide attempters who did not seek medical help were not characterized. On the other hand, comparison subjects were not recruited through random sampling, and hence the risk factor profile of the comparison subjects may not be representative of the older adult population locally. Nonetheless, the prevalence of depressive disorders in our comparison subjects (N=99) was 5%. The same prevalence rate was reported in the elderly control subjects of a local case-controlled psychoautopsy study, in which comparison subjects were recruited randomly from a census registry collected for a thematic household survey of the local government.34 Also, the chosen measures of executive function and trait impulsivity may not be sensitive enough to define the subtle psychopathological changes that mediate the suicide act in nondemented older people. It is also important to note that the cross-sectional nature of the study does not allow any causal relationship to be inferred between the putative risk factor and clinical outcomes. Finally, the inter-rater reliability of the psychiatric diagnoses could not be ascertained, as the research interviews were conducted only once by one SCID rater.
In this study, the summated scores on age-adjusted CVRFs were not significantly different between older men and women in the comparison group (7.71 vs 7.24). The observed association of CVRFs with suicide attempt in women only was unlikely due to the biased sampling of healthy women in the comparison group. Sex difference has been reported across different risk factor studies on mood disorders. Epidemiologic studies consistently report a higher prevalence of depression in adult women than adult men. Explanations offered for this sex difference include reporting tendency and pathophysiologic differences of a biological, psychological, and/or social nature.50–52 Higher prevalence rates among women seem to persist in later-life depression.53 In depressive conditions developed in the context of medical comorbidity, women may be twice as likely to develop poststroke depression than men,54 but increased white matter hyperintensities were found among clinically depressed older men.55 One cannot easily reconcile these conflicting observations from different studies to conclude whether older men or women are more susceptible to the psychopathologic effect of cerebrovascular pathologies. The direction of causality and the host of mediators or moderators acting between the associations of cerebrovascular pathologies with later-life affective disorders remain intriguing. Another study showed that depressive symptoms were associated with subclinical cerebrovascular disease among healthy older women, but not men, suggesting that women may be more susceptible to the affective consequences of poor cerebrovascular health.56 However, the observed association of higher CVRF burden with suicide attempt in women remained significant when the conjoint effect of major depression was examined in a multivariate model in this study. Also, our data suggest that CVRF score was significantly higher in depressed women who had made suicide attempts than depressed comparison subjects. Taken together, our observation and other published data on vascular depression hypothesis and related vascular-related psychopathology do not explain the observed association.
The female-specific association of attempted suicide with a higher burden of CVRFs in our sample is likely a complex one, as it remained significant after accounting for life events, social support, syndromal depression, personality traits, and impaired executive dysfunction in the multivariate models. When our data did not suggest moderating roles of depressive disorder, executive dysfunction, and trait impulsivity, it remains intriguing what are the definable and quantifiable psychopathological pathways linking higher age-adjusted CVRFs and suicide attempt in older women.
Given the knowledge gaps in the mechanisms underlying the associations between CVRFs and suicidal behavior in older adults, our findings may potentially inform targeted intervention for older women with higher cerebrovascular risk. The potential areas for intervention might involve proactive assessment of a fuller spectrum of psychopathological outcome of vascular pathologies in the aging brain, especially in women, tapping into tendency for suicide attempt beyond syndromal depression.
Clinical implications of sex-specific risk factor profile in elderly suicide
Knowledge of the sex-specific risk factor profiles for late-life suicidal behavior may have important clinical implications, as recent studies of community-based interventions in rural Japan and a care management suicide prevention program in Hong Kong showed a sex difference in service utlization.33,50 Earlier studies conducted in Gotland, Sweden, and Padua, Italy, showed that the effect of community-based suicide prevention for older people was specific to women.57,58 We speculate that older men may be less inclined to seek professional help, or the restricted social circle of older men poses significant barriers to timely intervention. The results of this study suggest independent risk conferred by life events among older men who had made a recent suicidal attempt after adjusting for depression diagnosis, trait neuroticism, executive cognitive function, and functional impairment. We thus postulate that risks for suicidal behavior in older men may escalate within a short period of time in reaction to life events, making timely effective intervention less likely to reach these vulnerable older adults.
Conclusion
Risk factors for cerebrovascular diseases, after accounting for age, life events, marital status, physical illness burden, functional impairment, depressive disorders, cognitive impairment, and trait neuroticism, were associated with attempted suicide in older women aged ≥65 years. Such an association was not observed in older men.
Acknowledgments
The authors would like to thank Dr Vivian Leung, former service coordinator of the NTE-ESPP of the Hong Kong Hospital Authority, for kindly facilitating the recruitment of the ESPP clients; Dr Joshua Tsoh for his invaluable comments on the study protocol; Ms Catherine Lee for her dedicated efforts in data collection and networking with the community day centers and residential facilities for older adults; and Ms Shirley Pang and Mr F Lai for their help in data collection. This study was supported by the US National Institute of Health’s Global Health Research Initiative Program for New Investigators Award (5R01TW007256-03; PI: Dr Chan).
Disclosure
The authors have no conflicts of interest to disclose.
References
World Health Organization. The World Health Report 2002: Reducing Risks, Promoting Healthy Life. Geneva, Switzerland: World Health Organization Publication; 2002:1–230. Available from: http://www.who.int/whr/2002/en/whr02_en.pdf?ua=1. Assessed August 25, 2014. | ||
World Health Organization. Figures and Facts About Suicide. Geneva, Switzerland: Department of Mental Health, World Health Organization; 1999:1–122. Available from: http://whqlibdoc.who.int/hq/1999/WHO_MNH_MBD_99.1.pdf. Assessed August 25, 2014 | ||
World population to exceed 9 billion by 2050: developing countries to add 2.3 billion inhabitants with 1.1 billion aged over 60 and 1.2 billion of working age [press release]. New York: United Nations Population Division/DESA; March 11, 2009. Available from http://www.un.org/esa/population/publications/wpp2008/pressrelease.pdf. Accessed August 25, 2014. | ||
Conwell Y, Duberstein PR, Caine ED. Risk factors for suicide in later life. Biol Psychiatry. 2002;52(3):193–204. | ||
Pompili M, Rihmer Z, Akiskal H, et al. Temperaments mediate suicide risk and psychopathology among patients with bipolar disorders. Compr Psychiatry. 2012;53:280–285. | ||
Pompili M, Gonda X, Serafini G, et al. Epidemiology of suicide in bipolar disorders: a systematic review of the literature. Bipolar Disord. 2013;15:457–490. | ||
Centers for Disease Control and Prevention and National Association of Chronic Disease Directors. The State of Mental Health and Aging in America Issue Brief 2: Addressing Depression in Older Adults: Selected Evidence-Based Programs. Atlanta, GA: National Association of Chronic Disease Directors; 2009:1–12. Available from http://www.ncoa.org/improve-health/center-for-healthy-aging/content-library/mental_health_brief_2.pdf. Assessed August 25, 2014. | ||
Mann JJ. Neurobiology of suicidal behavior. Nat Rev Neurosci. 2003; 4(10):819–828. | ||
Jollant F, Bellivier F, Leboyer M, et al. Impaired decision making in suicide attempters. Am J Psychiatry. 2005;162(2):304–310. | ||
Richard-Devantoy S, Berlim MT, Jollant F. A meta-analysis of neuropsychological markers of vulnerability to suicidal behavior in mood disorders. Psychol Med. 2014;44:1663–1673. | ||
Serafini G, Pompili M, Innamorati M, Giordano G, et al. The role of microRNAs in synaptic plasticity, major affective disorders and suicidal behavior. Neurosci Res. 2012;73:179–190. | ||
Alexopoulos GS, Meyers BS, Young RC, et al. Clinically defined vascular depression. Am J Psychiatry. 1997;154(4):562–565. | ||
Alexopoulos GS, Meyers BS, Young RC, et al. ‘Vascular depression’ hypothesis. Arch Gen Psychiatry. 1997;54:915–922. | ||
Thomas AJ, O’Brien JT, Davis S, et al. Ischaemic basis for deep white matter lesion hyperintensities in major depression: a neuropathological study. Arch Gen Psychiatry. 2002;59(9):785–792. | ||
Alexopoulos GS. The vascular depression hypothesis: 10 years later. Biol Psychiatry. 2006;60(12):1304–1305. | ||
Ishii N, Nishihara Y, Imamura T. Why do frontal lobe symptoms predominate in vascular dementia with lacunes? Neurol. 1986;36(3):340–345. | ||
Wolfe N, Linn R, Babikian VL, Knoefel JE, Albert ML. Frontal systems impairment following multiple lacunar infarcts. Arch Neurol. 1990; 47(2):129–132. | ||
Steingart A, Hachinski VC, Lau C, et al. Cognitive and neurologic findings in subjects with diffuse white matter lucencies on computed tomographic scan (leuko-araiosis). Arch Neurol. 1987;44(1):32–35. | ||
Kramer JH, Reed BR, Mungas D, Weiner MW, Chui HC. Executive dysfunction in subcortical ischaemic vascular disease. J Neurol Neurosurg Psychiatry. 2002;72(2):217–220. | ||
Perlmute LC, Tun P, Sizer N, McGlinchey RE, Nathan DM. Age and diabetes related changes in verbal fluency. Exp Aging Res. 1987; 13(1–2):9–14. | ||
Reaven GM, Thompson LW, Nahum D, Haskins E. Relationship between hyperglycaemia and cognitive function in older NIDDM patients. Diabetes Care. 1990;13(1):16–21. | ||
Desmond DW, Tatemichi TK, Paik M, Stern Y. Risk factors for cerebrovascular disease as correlates of cognitive function in a stroke-free cohort. Arch Neurol. 1993;50(2):162–166. | ||
Ahearn EP, Jamison KR, Steffens DC, et al. MRI correlates of suicide attempt history in unipolar depression. Biol Psychiatry. 2001;50(4):266–270. | ||
Chan SS, Lyness JM, Conwell Y. Do cerebrovascular risk factors confer risk for suicide in later life? A case-control study. Am J Geriatr Psychiatry. 2007;15(6):541–544. | ||
Bogner HR, Bruce ML, Reynolds CF III, et al. The effects of memory, attention, and executive dysfunction on outcomes of depression in a primary care intervention trial: the PROSPECT study. Int J Geriatr Psychiatry. 2007;22(9):922–929. | ||
Beaudreau SA, O’Hara R. Late-life anxiety and cognitive impairment: a review. Am J Geriatr Psychiatry. 2008;16(10):790–803. | ||
Heisel MJ, Duberstein PR, Conner KR, Franus N, Beckman A, Conwell Y. Personality and reports of suicide ideation among depressed adults 50 years of age or older. J Affect Disord. 2006;90(2–3):175–180. | ||
Pearson JL. Recent research on suicide in the elderly. Curr Psychiatry Rep. 2002;4(1):59–63. | ||
Conwell Y, Duberstein PR, Cox C, Herrmann J, Forbes N, Caine ED. Age differences in behaviors leading to completed suicide. Am J Geriatr Psychiatry. 1998;6(2):122–126. | ||
De Leo D, Scocco P. Treatment and prevention of suicidal behaviour in the elderly. In: Hawton K, Van Heeringen C, editors. The International Handbook of Suicide and Attempted Suicide. New York: John Wiley and Sons; 2000:556–570. | ||
Tsoh J, Chiu HF, Duberstein PR, et al. Attempted suicide in elderly Chinese persons: a multi-group, controlled study. Am J Geriatr Psychiatry. 2005;13(7):562–571. | ||
Hawton K. Studying survivors of nearly lethal suicide attempts: an important strategy in suicide research. Suicide Life Threat Behav. 2001; 32(1 Suppl):76–84. | ||
Chan SS, Leung VP, Tsoh J, et al. Outcomes of a two-tiered multi-faceted Elderly Suicide Prevention Program in a Hong Kong Chinese community. Am J Geriatr Psychiatry. 2011;19(2):185–196. | ||
Chiu HF, Yip PS, Chi I, et al. Elderly suicide in Hong Kong: a case-controlled psychological autopsy study. Acta Psychiatr Scand. 2004; 109(4):299–305. | ||
Beck AT, Schuyler D, Herman I. Development of suicidal intent scales. In: Beck AT, Resnik HL, Lethieri DJ, editors. The Prediction of Suicide. Maryland: Charles Press Publishers; 1974:45–46. | ||
Beck AT, Beck R, Kavoc M. Classification of suicidal behaviors. 1. Quantifying intent and medical lethality. Am J Psychiatry. 1975;132(3):285–287. | ||
So E, Kam I, Leung CM, Chung D, Liu Z, Fong S. The Chinese-bilingual SCID-I/P project: Stage 1. Reliability for mood disorders and schizophrenia. East Asian Arch Psychiatry. 2003;13(1):7–18. | ||
So E, Kam I, Leung CM, Pang A, Lam L. The Chinese-bilingual SCID-I/P project: stage 2- reliability for anxiety disorders, adjustment disorders and “no diagnosis”. East Asian Arch Psychiatry. 2003; 13(1):19–25. | ||
Costa PT Jr, McCrae RR. Professional Manual: Revised NEO Personality Inventory (NEO-PI-R) and the NEO Five-Factor Inventory (NEO-FFI). Florida: Psychological Assessment Resources, Inc.; 1992. | ||
Yang J, McCrae RR, Costa PTJ, et al. Cross-cultural personality assessment in psychiatric populations: the NEO-PI-R in the People’s Republic of China. Psychol Assess. 1999;11(3):359–368. | ||
Chiu HFK, Lee HC, Chung WS, Kwong PK. Reliability and validity of the Cantonese version of Mini-Mental State Examination. East Asian Arch Psychiatry. 1994;4(2):25–28. | ||
Nelson HE. A Modified Card Sorting Test sensitive to frontal lobe defects. Cortex. 1976;12(4):313–324. | ||
Chan CWY, Lam LCW, Wong TCM, Chiu HFK. Modified Card Sorting Test performance among community dwelling elderly Chinese people. East Asian Arch Psychiatry. 2003;13(2):2–7. | ||
deZubicaray G, Ashton R. Nelson’s (1976) Modified Card Sorting Test: a review. Clin Neuropsychol. 1996;10(3):245–254. | ||
Linn BS, Linn MW, Gurel L. Cumulative Illness Rating Scale. J Am Geriat Soc. 1968;16(5):622–626. | ||
Lawton MP, Brody EM. Physical Self Maintenance Scale (PSMS). Original observer-rated version. Psychopharmacol Bull. 1988;24(4): 793–794. | ||
American Heart Association. Stroke Risk Factor Prediction Chart. Dallas, TX: American Heart Association; 1995. | ||
Lyness JM, Heo M, Datto CJ, et al. Outcomes of minor and subsyndromal depression among elderly patients in primary care settings. Ann Intern Med. 2006;144(7):496–504. | ||
Kraemer HC, Stice E, Kazdin A, Offord D, Kupfer D. How do risk factors work together? Mediators, moderators, and independent, overlapping, and proxy risk factors. Am J Psychiatry. 2001;158(6):848–856. | ||
Oyama H, Watanabe N, Ono Y, et al. Community-based suicide prevention through group activity for the elderly successfully reduced the high suicide rate for females. Psychiatry Clin Neurosci. 2005;59(3): 337–344. | ||
Kessler RC, McGonagle KA, Swartz M, Blaaer DG, Nelson CB. Sex and depression in the National Comorbidity Survey. I: Lifetime prevalence, chronicity and recurrence. J Affect Disord. 1993;29(2–3):85–96. | ||
Grigoriadis S, Robinson GE. Gender issues in depression. Ann Clin Psychiatry. 2007;19(4):247–255. | ||
Mulstant BH, Ganguli M. Epidemiology and diagnosis of depression in late life. J Clin Psychiatry. 1999;60(Suppl 20):9–15. | ||
Paradiso S, Robinson RG. Gender differences in poststroke depression. J Neuropsychiatry Clin Neurosci. 1998;10(1):41–47. | ||
Lavretsky H, Lesser IM, Wohl M, Miller BL. Relationship of age, age at onset, and sex to depression in older adults. Am J Geriatr Psychiatry. 1998;6(3):248–256. | ||
Wendell CR, Hosey MM, Lefkowitz DM, et al. Depressive symptoms are associated with subclinical cerebrovascular disease among healthy older women, not men. Am J Geriatr Psychiatry. 2010;18(10):940–947. | ||
Rutz W, von Knorring L, Wálinder J. Frequency of suicide on Gotland after systematic postgraduate education of general practitioners. Acta Psychiatr Scand. 1989;80(2):151–154. | ||
De Leo D, Dello Buono M, Dwyer J. Suicide among the elderly: the long-term impact of a telephone support and assessment intervention in northern Italy. Br J Psychiatry. 2002;181:226–229. |
 © 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.