Back to Journals » Pediatric Health, Medicine and Therapeutics » Volume 9
A fracture, a family, legal entanglement, expensive investigation, and a familiar disease
Authors Okpechi U, Regis K , Arcia R, Soyemi K
Received 16 May 2018
Accepted for publication 22 June 2018
Published 10 September 2018 Volume 2018:9 Pages 97—100
DOI https://doi.org/10.2147/PHMT.S174250
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Roosy Aulakh

Ujuchukwu Okpechi,1 Kevin Regis,2 Rosibell Arcia,1 Kenneth Soyemi1,2
1Department of Pediatrics, 2Department of Emergency Medicine, Cook County Health and Hospitals System, John H Stroger Jr Hospital, Chicago, IL, USA
Abstract: Osteogenesis imperfecta can be commonly mistaken for child abuse because of similar pattern of injuries. AA is a 3-week-old baby who presented to our emergency department with excessive crying. Skeletal survey revealed subacute spiral fracture of the right humerus, right posterior eighth and ninth ribs, acute fracture of the left femur, bowing of tibia and femur, and osteopenia. Subsequent geneticist examination and genetic testing noted blue sclera and heterozygosity for a variant of COL1A gene.
Keywords: fracture, legal, investigation, infant
Introduction
Osteogenesis imperfecta (OI) can be commonly mistaken for child abuse because of similar pattern of injuries. Most cases are autosomal dominant mutations of type 1 collagen genes.1–4 It is important to acknowledge physical finding and order genetic testing early to prevent hardship to families and decrease medical expenditure.
Patient and observation
AA is a 3-week-old baby who presented to our emergency department (ED) with excessive crying. Parents noticed decreased movement of the left leg and right arm preceding the onset of AA’s sudden irritability. Parents denied recent fall, direct trauma, or shaking AA who lived with parents and two older siblings in a rented apartment in the city while visiting from Africa. There was no family history of easy bruising or fractures, domestic violence, drug/alcohol use, or involvement in social services. ED examination showed growth parameters at 10th percentile; AA was irritable and inconsolable with limited contralateral extremity movement; no bruising, pattern marks, or oral injuries were identified. Skeletal survey revealed subacute spiral fracture of the right humerus, right posterior eighth and ninth ribs, acute fracture of the left femur (Figure 1), bowing of tibia and femur, and osteopenia. Computed tomography scan was normal. MRI/MRA brain revealed left subacute subdural hemorrhage and right parieto-occipital calvarial flattening. Vital signs were normal, other screening laboratory tests were normal; eye examination was negative retinal hemorrhage. Department of Children and Family Services (DCFS) was notified for concern of nonaccidental trauma (NAT); siblings were taken into temporary DCFS custody. Subsequent geneticist examination and genetic testing noted blue sclera and heterozygosity for a variant of COL1A gene. Genes evaluated included BMP1, COL1A1, COL1A2, CRTAP, FKBP10, IFITM5, P3H(LEPRE1), PLOD2, PLS3, PP1B, SERPINF1, SERPINH1, SP7, TMEM38B, and WNT1 (Figure 2). Result was positive for COL1A coding DNA: C.371 G>T variant: pGly224Val (G224V) zygosity: heterozygous classification: pathogenic variant; no other reportable variants were detected by sequencing of the genes included on this panel. A written informed consent has been provided by the patient’s parents to have the case details and any accompanying images published for this study.
  | Figure 1 Fractures at initial presentation. Abbreviations: R, right; L, left. |
  | Figure 2 Algorithm for evaluation of osteogenesis imperfecta. Abbreviations: OI, osteogenesis imperfecta; PE, physical examination. |
Discussion
As visitors to USA, parents were unfamiliar with DCFS operations; subtle cultural differences may have led to communication barrier as parents needed time to process the sequence of events cascading from the diagnosis of fractures and NAT. This was confounded by the emotional stress and uncertainty about safety of their children who were taken into custody with strangers. After AA’s diagnosis was confirmed, parents reappeared in front of a judge who cleared AA for discharge and travel to country of parent’s origin for continuation of care. AA is heterozygous for the G224V pathogenic variant in the COL1A1 gene, consistent with a molecular diagnosis of autosomal dominant OI. Targeted array comparative genomic hybridization analysis with exon-level resolution of the genes on this panel yielded uninterpretable results due to suboptimal quality of the DNA obtained from the submitted specimen. Most pathogenic variants in COL1A1 are sporadic.5,6 Because of the potential for mosaicism in an unaffected parent, variant-specific testing of the parents of AA was made available to help determine if the variant was inherited or arose de novo; in addition, this will provide information required for accurate genetic counseling for this family. Parents did not complete testing as of time of writing; if neither parent is found to carry the G224V variant in the COL1A1 gene, the possibility of mosaicism cannot be excluded, and offspring of either parent may be at risk of carrying this variant. Molecular prenatal diagnosis is available in future pregnancies, if desired; genetic counseling is recommended to discuss the implications of this test report. This multifaceted clinical investigation involved the use of resources; for analysis, cost was stratified into four categories: 1) hospital, 2) social, 3) legal, and 4) family. For hospital services, intensity of service included nine inpatient admission days, 14 specialty consultations (with five services), 23 laboratories, and seven radiological encounters. Laboratory panel testing and services accounted for 47% of AA’s encounters (Figure 3). Social worker, legal services including family court appearances, and DCFS investigative services all contributed to the overall cost. The estimated cost of investigating AA’s fractures using medical consumer price index easily surpassed $500,000 when all the cost factors and drivers are considered.7
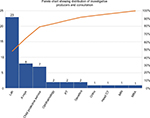  | Figure 3 Services and consultation. Abbreviations: CT, computed tomography; PT, physical therapy. |
Conclusion
It is important in the initial investigative phases of unexplained fractures, families should be promptly provided social and psychological resources to help them cope with the unfortunate circumstances.8 The extent of such investigations when signs suggestive of confounding systemic diseases and consistent history should be balanced to ensure child safety as well as limit unnecessary expenditure.
Disclosure
The authors report no conflicts of interest in this work.
References
Tournis S, Dede AD. Osteogenesis imperfecta - A clinical update. Metabolism. 2018;80:27–37. | ||
Morello R. Osteogenesis imperfecta and therapeutics. Matrix Biol. In press 2018. | ||
Mitaka H. Osteogenesis imperfecta and blue sclera. QJM. 2018. Available from: https://academic.oup.com/qjmed/advance-article/doi/10.1093/qjmed/hcy060/4942476. Accessed August 27, 2018. | ||
Harrington J, Sochett E, Howard A. Update on the evaluation and treatment of osteogenesis imperfecta. Pediatr Clin North Am. 2014;61(6):1243–1257. | ||
Zarate YA, Clingenpeel R, Sellars EA, et al. COL1A1 and COL1A2 sequencing results in cohort of patients undergoing evaluation for potential child abuse. Am J Med Genet A. 2016;170(7):1858–1862. | ||
Caparros-Martin JA, Aglan MS, Temtamy S, et al. Molecular spectrum and differential diagnosis in patients referred with sporadic or autosomal recessive osteogenesis imperfecta. Mol Genet Genomic Med. 2017;5(1):28–39. | ||
Bureau of Labor Statistics. Measuring Price Change in the CPI: Medical Care; 2018. Available from: https://www.bls.gov/cpi/factsheets/medical-care.htm. Accessed May 10, 2018. | ||
Pereira EM. Clinical perspectives on osteogenesis imperfecta versus non-accidental injury. Am J Med Genet C Semin Med Genet. 2015;169(4):302–306. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
