Back to Journals » Open Access Surgery » Volume 15
A Diagnostic Approach to a Rare Case of a Recto-Cutaneous Fistula Following Recurrent Perianal Abscess: A Case Report
Authors Mekonen Y
Received 29 January 2022
Accepted for publication 4 April 2022
Published 18 April 2022 Volume 2022:15 Pages 39—44
DOI https://doi.org/10.2147/OAS.S360182
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Professor Luigi Bonavina
Yohannes Mekonen
Department of Surgery, Section of General Surgery, Halibet National Referral Hospital, Asmara, Eritrea
Correspondence: Yohannes Mekonen, Department of Surgery, Section of General Surgery, Halibet Regional Referral Hospital, Asmara, Eritrea, Tel +291-1-7155478, Email [email protected]
Background: Perianal abscess is caused by an infection of anal glands located in between the sphincter muscles of the anal canal. An enterocutaneous fistula is a chronic manifestation of an acute perirectal process that forms an anal abscess. The rate of perianal abscess is increasing annually and the incidence of fistula formation following perianal abscess occur reportedly at a higher rate. Precise diagnosis of a recto-cutaneous fistula is a key factor in its eventual management. This article discusses a diagnostic approach to a rare case of a recto-cutaneous fistula using magnetic resonance imaging (MRI).
Case Report: A 24-year-old male presented with a 3 × 3 cm right buttock lesion of 5 months’ duration. The wound had a scanty whitish discharge and flatus passage. He had been diagnosed with perianal abscess twice before, for which incision and drainage was done. The problem did not resolve and he had an additional, yet futile, explorative surgery. Physical examination revealed an opening on right buttock with spontaneous purulent discharge. Laboratory analysis of fluid specimen yielded no active bacterial growth. The patient had prolonged antibiotic treatment with no improvement. Pelvic MRI identified a long and deep fistulous tract extending from the right gluteal region into the muscular plane of the gluteus, invading the pubo-rectalis muscle and above levator ani muscle deep into the rectum, compatible with a recto-cutaneous fistula.
Conclusion: Although rare, recto-cutaneous fistula should be diagnosed as early as possible to avoid long-lasting complications. There are several examinations to diagnose perianal fistula and MRI is of particular interest in assessment of fistula depth, route and extension given its high diagnostic accuracy. This report can aid surgeons in making accurate surgical plans pre-operatively and minimizing harm caused by surgery to patients.
Keywords: perianal abscess, recto-cutaneous fistula, magnetic resonance imaging, MRI
Background
Perianal abscess is a common perianal ailment. It is more common in young men and its incidence rate is increasing annually.1 Anal glands are composed of ducts for secretion of mucus so as to lubricate the anal canal.2 An abscess is caused by an infection of the anal glands and once an inflammatory reaction surfaces at the perianal area, it is called fistula in-ano.3,4 An enterocutaneous fistula is an abnormal connection between an intra-abdominal gastrointestinal tract and the skin and in this case, a recto-cutaneous fistula is one subtype. A high-output enterocutaneous fistula is considered as fistula with >500 mL/24 hours, low output <200 mL/24 hours, and a moderate output as 200–500 mL/24 hours. While majority of these types of fistulae are iatrogenic (75–85%), between 15 and 25% arise spontaneously.5
Recurrence of perianal abscess and development of fistula after treatment of perianal abscess occur reportedly at a rate 6–85%.6 This is owing to the loose anal canal missed during surgery or occult abscesses which may not be diagnosed before surgery. Treatment of such cases is very tough, and the key solution is precise diagnosis before surgical procedure.7 Given the low movement of pelvic organs and higher diagnostic accuracy of magnetic resonance imaging (MRI), high quality images can be acquired, accurately describing the anatomical structures of anal canal and the relationship among perianal abscesses, fistulae, muscles around the anus and rectum.8,9
To the best of the author’s knowledge, there is a paucity of data regarding perianal abscesses in general and complex perianal fistula especially in our country. This case report illustrates an investigative approach to a patient with a rare and atypical presentation of a recto-cutaneous fistula, who came referred to Halibet National Referral Hospital, in Asmara, Eritrea.
Case Presentation
A 24-year-old male patient presented to Halibet National Referral Hospital on October 2021 with a complaint of right buttock lesion of 5 months’ duration. The wound had an intermittent whitish discharge, scanty in amount, exaggerated during activity. He claimed to seldom experience pain, difficulty passing stool and a flatus passage through the buttock opening at most times. He was diagnosed with perianal abscess twice before in a regional hospital nearby, for which he underwent incision and drainage. The problem did not resolve and he had an additional explorative surgery, which was futile (Figure 1A). He is not married, generally in good health without any sign of immune-depression, had no tobacco smoking or drinking habits, and was under no regular treatment. He tested negative for a retro-viral infection.
 |
Figure 1 Images of the patient elucidating the times he had his initial explorative surgery after repeated incision and drainage (A) and following his diagnosis with recto-cutaneous fistula (B). |
Physical examination revealed an opening sinus noted on right upper outer quadrant of the buttock, 3 × 3 cm, with spontaneous scanty purulent discharge (Figure 1B). Digital rectal exam spotted an indurated lesion at around 1 o’clock and a rectal vault with no mass. He was afebrile, not anemic and no lymphadenopathy was found.
The patient was investigated with a complete blood count, chest X-ray and lumbosacral X-ray, which all showed a normal study. A sample from the wound was taken for culture, sensitivity and a gene expert. Laboratory analysis of the fluid specimen yielded no active bacterial growth. The patient also had prolonged treatment with antibiotics, with no improvement seen.
Several differential diagnoses were considered for a recurrent perianal abscess and fistula such as complex fistula, extra-pulmonary tuberculosis, recurring epidermal cyst of gluteal region, hidradenitis suppurativa, pilonidal cyst, mycosis and cutaneous metastatic lesions.
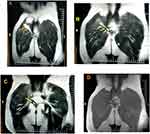
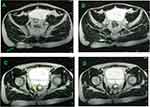
To determine the precise depth and route of the buttock wound, MRI of the pelvic area was performed. Enhancement images, both coronal and transverse, identified a long tortuous band of high signal intensity T2 weighted (T2W1) and isointense signal on T1 weighted (T1W1) (Figures 2 and 3). The external opening of the fistula lies exteriorly in the right side of upper outer quadrant of the gluteal region and the fistula tract goes deep through the muscular plane of the gluteus, invading the pubo-rectalis muscle and up above the levator ani muscle. The internal opening of the fistula tract lies in the lower part of the middle zone of the rectum with a clear boundary. The findings are compatible with a recto-cutaneous fistula.
The patient received prolonged antibiotic therapy as sepsis control, analgesics as pain control and daily wound care. Given the scarcity of expertise on complex perianal surgeries in our country, the patient was referred to abroad for a better management with outpatient follow-up planned.
Discussion
To the best of the author’s knowledge, this is the first reported case of a recto-cutaneous fistula following a recurrent perianal abscess in Eritrea. Health care professionals need to be aware of such entities and have a high index of suspicion, especially in young patients with atypical perianal wounds. Patients who present with an abnormal complaint of a buttock wound following recurrent abscesses not amenable to repeated explorative surgeries need appropriate investigative tools. Nowadays, MRI is used by scholars in developed countries as the gold standard for the assessment and classification of anal fistulae.
Initial fistula formation possesses more pus, yellow and viscous in color, accompanied by a fecal odor. Then, the content decreases, with intermittent pus discharge. If the patient is too tired, pus will increase, and may even have feces outflow. When the tract is open, no pain is usually reported. If the external opening closes and pus collects inside, there may be pain. If purulent content flows out after ulceration, symptoms alleviate. However, stool flows into the tract causes pain and it is aggravated when defecating.10 As much as a common illness, perianal abscess must be detected early to avoid complications. The main complication is a fistula formation, a discomforting and disabling disease. Recurrent abscesses can lead to such conditions and this may be due to therapeutic differences or conventions in reporting and labeling fistulae as recurrences or complications. There are several examinations to diagnose perianal fistula. Of importance is the technique of medical imaging with particular interest in the assessment of perianal fistula depth, route and extension. Currently, pre-operative MRI of perianal abscesses and fistulae has not attracted much attention.
Several protocols for managing enterocutaneous fistula have been advocated by numerous authors. Moreover, it is vital that the patient is treated in a center with substantial experience in managing enterocutaneous fistulae and that a careful and inter-disciplinary approach is used.11,12 Apart from pain and sepsis control as well as daily wound care, surgery remains the ultimate management with an objective of forming no new enterotomy while giving the best chance of cure from the fistula, re-establishing bowel continuity and preserving maximal bowel length.13
Prior to the imaging technique utilized in this case, the peri-rectal region and the previous area of the perianal abscess were meticulously investigated and no opening or signal of a peri-rectal fistula was found. This outcome suggests that the irritation and infectious processes that may have followed the abscesses within the pelvis may have initiated a fistula tract between the rectum and skin. Appropriate diagnosis and judicious follow-up as well as surgical intervention, if needed, can prevent such severe complications. This case report excels in illustrating such investigative need in patients recurrently affected by perianal abscess presenting with complicated perianal wound as such examination avoids unnecessary interventions and lesion progression to an advanced and disabling disease.
Conclusion
Although data regarding the burden of perianal abscess and fistula in Eritrea are quite scarce, a high index of suspicion towards complex perianal fistula is required. Herein, close collaboration with primary care physicians and radiologists was important in diagnosing a rare complex fistula in the patient. The report can help surgeons make accurate surgical plans pre-operatively and minimize the harm caused by surgery to patients, playing a very critical role in postoperative recovery and preservation of defecation function.
Abbreviation
MRI, magnetic resonance imaging.
Data Sharing Statement
Data sharing is not applicable to this report as no datasets were generated or analyzed during the study.
Ethical Approval and Consent for Publication
This case report does not involve any active intervention on the patient and therefore ethics approval is waived.
Written informed consent was acquired from the patient for publication of this report and associated images. A copy of written consent is available for review by the Editor-in-Chief of this journal.
Acknowledgments
Special thanks to Dr. Yonatan Hagos, chief physician in the department of radiology, who assisted in planning and performing the imaging. The case report has not been presented in any scientific meetings.
Author Contributions
The author made a substantial contribution in conception, study design, data acquisition and interpretation of the report; took part in drafting, revising and critically reviewing the article; gave final approval of the version to be published; agreed on the journal to which the article has been submitted; and agreed to be accountable for all aspects of the work.
Funding
This report received no specific grant from any funding agency in the hospital, public, commercial, or not-for-profit sectors.
Disclosure
The author declares that there were no competing interests.
References
1. Singh K, Singh N, Thukral C, Singh KP, Bhalla V. Singh KP and Bhalla V. Magnetic Resonance Imaging (MRI) evaluation of perianal fistulae with surgical correlation. J Clin Diagn Res. 2014;8(6):RC01–4. doi:10.7860/JCDR/2014/7328.4417
2. Gujrathi R, Gupta K, Ravi C, Pai B. Sciatica: an extremely rare complication of the perianal abscess. Pol J Radiol. 2016;81:370–373. doi:10.12659/PJR.897269
3. Festen C, van Harten H. Perianal abscess and fistula-in-ano in infants. J Pediatr Surg. 1998;33(5):711–713. doi:10.1016/s0022-3468(98)90193-2
4. Christison-Lagay ER, Hall JF, Wales PW, et al. Non-operative management of perianal abscess in infants associated with decreased risk for fistula formation. J Pediatr. 2007;120(3):e548–552. doi:10.1542/peds.2006-3092
5. Berry SM, Fischer JE. Classification and pathophysiology of entero-cutaneous fistulas. Surg Clin N Am. 1996;76(5):1009–1018. doi:10.1016/s0039-6109(05
6. Karlsson AJ, Salö M, Stenström P. Salö M and Stenström P. Outcomes of various interventions for first-time perianal abscesses in children. BioMed Res Int. 2016;2016:1–6. doi:10.1155/2016/9712854
7. Kim PH, Park SH, Jin K, et al. Supplementary anal imaging by magnetic resonance enterography in patients with Crohn’s disease not suspected of having perianal fistulas. Clin Gastroenterol Hepatol. 2020;18(2):415–423. doi:10.1016/j.cgh.2019.07.038
8. Yang J, Han S, Xu J. Deep learning-based magnetic resonance imaging features in diagnosis of perianal abscess and fistula formation. Contrast Media Mol Imaging. 2021;2021:1–8. doi:10.1155/2021/9066128
9. Bezzio C, Bryant RV, Manes G, Maconi G, Saibeni S. Maconi G and Saibeni S. New horizons in the imaging of perianal Crohn’s disease: transperineal ultrasonography. Expert Rev Gastroenterol Hepatol. 2017;11(6):523–530. doi:10.1080/17474124.2017.1309285
10. Kalinin AA, Higgins GA, Reamaroon N, et al. Deep learning in pharmacogenomics: from gene regulation to patient stratification. Pharmacogenomics. 2018;19(7):629–650. doi:10.2217/pgs-2018-0008
11. Rahbour G, Gabe SM, Ullah MR, et al. Seven-year experience of enterocutaneous fistula with univariate and multivariate analysis of factors associated with healing: development of a validated scoring system. Colorectal Dis. 2013;15(9):1162–1170. doi:10.1111/codi.12363
12. Irina GR, Genevieve BM. Enterocutaneous fistula: proven strategies and updates. Clin Colon Rectal Surg. 2016;29(2):130–137. doi:10.1055/s-0036-1580732
13. Fazio VW, Coutsoftides T, Steiger E. Coutsoftides T and Steiger E. Factors influencing the outcome of treatment of small bowel cutaneous fistula. World J Surg. 1983;7(4):481–488. doi:10.1007/BF1655937
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.