Back to Journals » Clinical, Cosmetic and Investigational Dermatology » Volume 15
A Cross-Sectional Study on the Relationship Between Rosacea Severity and Quality of Life or Psychological State
Authors Yang F , Zhang Q , Song D, Liu X, Wang L, Jiang X
Received 23 September 2022
Accepted for publication 5 December 2022
Published 20 December 2022 Volume 2022:15 Pages 2807—2816
DOI https://doi.org/10.2147/CCID.S390921
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jeffrey Weinberg
Fengjuan Yang,1 Qian Zhang,1 Deyu Song,1 Xu Liu,1 Lian Wang,1 Xian Jiang1,2
1Department of Dermatology, West China Hospital, Sichuan University, Chengdu, People’s Republic of China; 2Laboratory of Dermatology, Clinical Institute of Inflammation and Immunology, Frontiers Science Center for Disease-Related Molecular Network, West China Hospital, Sichuan University, Chengdu, People’s Republic of China
Correspondence: Xian Jiang, Email [email protected]
Background: Rosacea appears predominantly in highly visible areas of the facial region.
Objective: To investigate the psychological status and quality of life(QOL) of rosacea.
Methods: We used a hospital-based cross-sectional analytical study design between Jan 1, 2020, and Jan 1, 2021. We analyzed the differences and correlations in the severity of rosacea and its impacts on QOL and mental health, separately.
Results: 469 patients with rosacea were included. The mean Dermatology Life Quality Index (DLQI) score was 12.6± 7.7 and the affected level of DLQI was moderately severe. The total score of Rosacea-specific Quality-of-Life instrument (RosQol) was 2.34 ± 0.84, and the scores of emotion, symptoms, and function were 2.41 ± 0.99, 2.37 ± 0.82, and 2.03 ± 0.89, respectively. 44.8% of patients suffered from anxiety and 37.5% from depression. There were statistically significant differences in the incidence of anxiety (p < 0.001), the DLQL (p =0.02), RosQol emotion (p =0.04), symptom (p < 0.01) and function (p =0.02) scores in the different severity. In addition, worsening QOL was significantly associated with increased disease severity [Spearman’s rank correlation index (r) ranging from 0.171 to 0.266,p< 0.01 (RosQol); r =0.104,p =0.024 (DLQI)]. There was also a positive correlation between anxiety [r =0.155; p< 0.01] and the different severity levels.
Conclusion: Rosacea maybe has a greater significant impact on patient’s QOL and mental health. And the impact of QOL and mental health tend to deteriorate significantly with increasing disease severity. The relationship suggests that QOL assessment is of great interest in clinical practice and should be further explored.
Keywords: rosacea, severity, quality of life, depression, anxiety
Introduction
Rosacea is a chronic recurrent inflammatory disease affecting facial skin, commonly in women aged 30–55.1–3 The estimated prevalence of rosacea ranges from 0.1% to 22%,4–7 while the prevalence was reported as 3.48% in China.8 The pathogenesis of rosacea is complex, involving multiple links such as genetics, microbial dysbiosis, neurovascular dysfunction, and immune system disorders.9–12 Rosacea is characterized by persistent erythema, telangiectasia, papules and pustules, and even rhinophyma. Patients may experience discomfort such as burning, stinging, and tingling sensation. It is clinically characterized by relapses or exacerbations in response to stimuli such as elevated temperature and emotional stress.1,2,13,14 In recent years, studies have shown that rosacea is associated with several systemic diseases.15
Facial features are critical in influencing others’ perceptions of attractiveness and can affect a range of prominent social outcomes, from mate choice and hiring decisions to decisions about social exchange.16–18 Since rosacea appears predominantly in highly visible areas of the facial region, it can affect the patient’s cosmetic appearance and affect patient’s social and occupational interactions. This in turn has a negative impact on the patient’s quality of life (QOL) and mental health.19 Therefore, patients with rosacea suffer from a tremendous psychological burden that should not be underestimated. Nowadays, the impact of rosacea on QOL and mental health is a growing concern for dermatologists. A variety of studies have shown an increased risk of anxiety and depression and impaired QOL in patients with rosacea.20–24 The clinical features are heterogeneous, so the burden of the disease it causes may vary. However, the complex relationship between rosacea severity and QOL and mental health has not been examined in depth.
Methods
Study Design
The study was designed as a cross-sectional, observational study and conducted in the diagnostic room of a tertiary hospital between Jan 1, 2020, and Jan 1, 2021. We collected information by dermatologists asking patient’s information and by patients writing standardized questionnaires.
This study was approved by the Medical Ethics Committee of the West China Hospital of Sichuan University (Clinical Trials.gov ID:2019–248). The work described has been carried out under The Code of Ethics of the World Medical Association (Declaration of Helsinki). All enrolled patients signed the informed consent form.
Inclusion criteria were: (1) diagnosed with rosacea according to the 2019 National Rosacea Society Expert Committee (NRSEC) criteria;14 (2) capable of understanding the content of the questionnaire; (3) read and signed the informed consent.
Exclusion criteria were: (1) Patients with other concurrent facial skin diseases such as acne, seborrheic dermatitis, psoriasis, eczema, and systemic lupus erythematosus; (2) Patients with neuropsychiatric diseases such as migraine, schizophrenia, anxiety disorder, depressive disorder.
Data Collection
Clinical Features of Rosacea and Assessment of Its Severity
Our study analyzed clinical features based on rosacea phenotypes including flushing, persistent erythema, papules and pustules, telangiectasia, phymatous changes, edema, dry sensation, burning sensation as well as stinging sensation. Moreover, our study collected disease duration, and comorbidities of rosacea.
The severity was measured using Investigator’s Global Assessment (IGA) and Clinician’s Erythema Assessment (CEA).25,26 And the CEA assessment referred to the VISIA® system which is the most commonly used to quantify the severity of erythema in studies.27
QOL and Psychological State
Dermatology Life Quality Index (DLQI) was the first dermatology-specific QOL and was the most widely used.28,29 The DLQI comprised of ten items, each with four answers. Each item was scored on a four-point scale: not at all (0); a little (1); a lot (2); very much (3). The DLQI total score was calculated by summing the score of each question, a higher score correlates with a more impaired QoL. The clinical interpretation of the DLQI scores is as follows: Grade 1 (0~1), no impact on the patient’s life at all; grade 2 (2~5), low impact on the patient’s life; grade 3 (6~10), moderate impact on the patient’s life; grade 4 (11~20), very large impact on the patient’s life; grade 5 (21~30), extremely large impact on the patient’s life.
Rosacea-specific Quality-of-Life instrument (RosQol) was a validated tool designed specifically for rosacea patients to assess the QOL, which consisted of 21 rosacea-specific items, grouped into three domains: symptoms, function, and emotion. Each item ranges from 1 (never) to 5 (always), with higher scores indicating greater QOL impairment.30
We assessed the psychological state using the Hospital Anxiety and Depression Scale (HADS) (Zigmond & Snaith, 1983). HADS has been widely applied in screening for anxiety and depression in patients quickly and has shown to demonstrate good to excellent psychometric properties.31–33 HADS was divided into the Anxiety subscale (HADS-A) and the Depression subscale (HADS-D), both containing seven intermingled items (scored from 0 to 3). 0 ~ 7 points represent normal, 8 ~ 10 points represent mild anxiety, and depression, 11 ~ 14 points represent moderate anxiety and depression, and 15 ~ 21 points represent severe anxiety and depression.
Quality Control
Diagnosis of all patients with rosacea was determined by the same senior dermatologist according to the standard of diagnosis, which makes selection bias less likely in this study. The patients were assigned severity scores (IGA and CEA) by specialized dermatologists, and all scores were done by the same doctor. All data were collected by trained study personnel under standard protocols in Dermatology diagnostic room. When collecting data, investigators had a unified, professional and detailed explanation for the questionnaire, so that patients would not misunderstand the content. Each questionnaire was completed in approximately 15–20 minutes. After each questionnaire was completed, data were recorded by two investigators and the original data were checked at the time of data entry.
Statistical Analysis
All statistical analyses were performed using SPSS statistical software (version 28, IBM). Quantitative variables are expressed as the mean ± standard deviation (SD). Categorical data are reported as frequency and percentage.
Patients were divided into different groups according to the severity. The single-factor analysis assessed quantitative variables in different groups and the homogeneity of variance test was evaluated before the single-factor analysis. The Kruskal–Wallis test was used to compare non-normal distribution data. Comparisons between more than three groups of ordered rank data were performed using the Spearman test. The correlation between patients in different severity groups and their QOL and mental state level was assessed using Spearman’s rank correlation. A two-sided p-value < 0.05 was considered statistically significant.
Results
Clinical Features of Rosacea and Assessment of Its Severity
A total of 469 patients with rosacea were included, with an average age of 36.6 ± 10.6 years. The sex ratio was 5.2 (392 female and 77 male).The main clinical features included are summarized in Table 1. The scores of CEA were predominantly mild (46.9%), moderate (29.9%), and severe (6.4%). IGA scores were mild in 33.9%, moderate in 31.6%, and severe and very severe in 20%. Overall, the severity in our study was mainly mild to moderate.
 |
Table 1 Clinical Characteristics of Rosacea |
 |
Table 2 Psychological State (Anxiety and Depression) in Patients with Rosacea |
QOL and Psychological Impact
The results of HAD showed that 44.8% of patients suffered from anxiety and 37.5% from depression, with both anxiety and depression being predominantly mild to moderate (Table 2).
The majority of patients (94.9%) had an unfavorable impact on their QOL. The mean DLQI score was 12.6±7.7 and the impact of rosacea on QOL was mainly moderate to severe (Table 3).
 |
Table 3 DLQI Assessment Results in Patients with Rosacea |
In terms of RosQol, the total score of RosQol was 2.34 ± 0.84, and the total scores of emotion, symptoms, and function were 2.41 ± 0.99, 2.37 ±0.82, and 2.03 ± 0.89, respectively (Table 4).
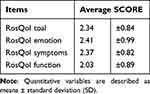 |
Table 4 RosQol Assessment Results in Patients with Rosacea |
Differential Analysis of QOL and Psychological Impact of Rosacea Patients with Different Severity Levels
As can be seen from Table 5, there were statistically significant differences in RosQol emotion (p = 0.04), symptoms (p < 0.01) and function (p = 0.02) at different severity levels (IGA), as well as differences in DLQI (p = 0.02). While from the CEA grouping (Table 6), there was no significant variability between the groups.
 |
Table 5 Variability in QOL and Psychological State (Anxiety and Depression) Between Different Severity Levels (IGA) |
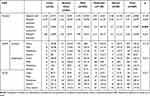 |
Table 6 Variability in QOL and Psychological State (Anxiety and Depression) Between Different Severity Levels (CEA) |
The incidence of anxiety was different with different severity, and the difference was statistically significant (p < 0.001). Furthermore, patients with moderate to severe rosacea had a greater proportion of negatively affected QOL, a higher probability of anxiety and depression, and more severe anxiety and depression.
Correlation Analysis of the Severity of Rosacea with QOL and Psychological Impact
It is summarized from Table 7 that the correlations between the severity of IGA and DLQI (p = 0.024), RosQol emotion (p < 0.01), symptoms (p < 0.01), function (p < 0.01), and anxiety (p <0.01) were all statistically significant. And all the correlations were highly significant and positive.
 |
Table 7 Correlation Between the Severity of Rosacea and Its QOL and Psychological Status (Anxiety and Depression) |
From the perspective of CEA, the correlation coefficients were all positive, and the correlations with RosQol’s symptoms (p < 0.01) and functions (p = 0.025) were also statistically significant.
Discussion
QOL is a term implemented by the World Health Organization that represents an index of people’s ability to lead a productive and enjoyable life.34 However, the impact of skin diseases on patients’ QOL and even psychological well-being has always been a concern for dermatologists. Psoriasis, atopic dermatitis, hidradenitis suppurativa, ichthyosis, acne-related scars, and other skin conditions all have varying degrees of negative impact on QOL.35–39 A study summed up the important role of assessing QOL for diseases in the field of dermatology in the following five categories: inform clinical decisions, clinician-patient communication, awareness of skin disease burden, informing the consultation, and clinical service administration.40 As a result, QOL measures are now routinely incorporated into dermatological studies. DLQI is the most extensively used skin-specific QOL measure in over 40 dermatologic conditions and is also recommended by the ROSacea COnsensus for assessing the burden of patients with rosacea.41 RosQol is a quality-of-life measurement tool specifically for rosacea.25 In our study, the use of these two tools to assess QOL in rosacea can complement each other and make the results convincing.
Our results showed that the impact of rosacea on QOL was mainly moderate to severe and the average score of DLQI was 12.6±7.7, which is within the range reported in systematic reviews (4.1–17.3).42 In our study, all patients were recruited from tertiary hospitals rather than the community and may have had more severe rosacea or more severe impairment of QOL, which may have contributed to selection bias leading to a relatively high DLQI score. In terms of RosQol, the total score of RosQol was 2.3 and the scores of the three aspects of emotion, symptoms, and function were 2.4,2.4,2.0, respectively. There are still relatively few studies on RosQol to assess QOL in rosacea patients, and our results show that rosacea has an adverse impact in three areas: emotion, symptoms, and function, with a more severe impact on emotion and symptoms.
Rosacea not only has a negative impact on the QOL but also affects the psychological health of the patients. Rosacea is associated with multiple comorbidities.43 The most common associated psychosocial comorbidities.24,44–46 And there is a strong correlation between depression and rosacea, the more severe the rosacea, the more severe the depression.47 In addition, emotional factors often act as triggers for rosacea, and patients are frequently exacerbated by emotional stress.23 We used HADS to screen patients with rosacea for anxiety and depression. 44.8% of patients suffered from anxiety and 37.5% from depression. Both anxiety and depression were predominantly mild to moderate in our results, which is consistent with previous studies.48,49 In a sense, HADS is only a screening tool and does not accurately diagnose anxiety and depression, but in general, our study clearly indicates the presence of psychological problems of anxiety and depression in patients with rosacea.
From the perspective of the mechanisms of rosacea and anxiety and depression, recent advances in research have proposed the concept of influencing the gut-brain-skin axis in affecting rosacea comorbidity. Microecological dysbiosis is often observed in patients with psychiatric disorders, and psychological stressors induce various neurotransmitters or neuropeptides to impair the integrity of the gastrointestinal tract, leading to intestinal and systemic inflammation.11,50,51 In addition, rosacea may share some common pathophysiological features with depression and anxiety, and both share similar inflammatory pathways. Interleukin 17 is considered a key cytokine in the pathophysiology of neurological and psychiatric disorders and plays an important role in the development and exacerbation of rosacea. In addition, shared mediators include interleukin (IL)-1, IL-12, and MMP, among others.52–55 All of the above can explain the relationship between rosacea and anxiety and depression in some sense.
Although a large number of previous studies have analyzed the impact of rosacea on the QOL and mental health, there is little research on the different rosacea’s clinical severity has different effects on QOL and mental health. In our study, there were statistically significant differences in the level of impaired QOL and the incidence of anxiety and depression of different severity. And of note, we found that the more severe the disease, the greater its impact on QOL, and the higher the incidence of anxiety and depression in patients. A systematic review also concluded the negative impact on QOL appeared to be associated with disease severity.42 This variability and this trend are very significant from the IGA grouping. While from the CEA grouping, there is no significant variability between the groups. CAE can only evaluate the facial erythema of the patient at the time of consultation. While IGA considers not only facial erythema but also papules, phymatous changes, and other conditions. IGA can better reflect the overall situation of the patient’s face, which means that the IGA is more representative of the severity. These differences between the two scales seem to explain our results. Moreover, Differences in QOL impact between different skin subtypes of rosacea were found in a study, with patients with the papulopustularpersistent (PP), and phymatous (PH) rosacea subtypes likely to carry the greatest QOL burden.56 Therefore, symptoms other than erythema, such as papules, pustules, and phymatous changes, may have a greater impact on the patient, we suspect that this may be associated with papules pustules and phymatous changes often combined with facial erythema, as well as uncomfortable symptoms such as tingling, and the treatment cycle is longer.
Secondly, we performed a correlation analysis of the severity with the grade of QOL and the severity of anxiety and depression, respectively. From our findings, both the degree of QOL affected and the severity of anxiety and depression were statistically positively correlated with the severity of rosacea. Oussedik et al concluded that QOL in patients with rosacea was affected by :(1) physiological factors such as pain, irritation, burning, and dryness; (2) psychosocial factors, such as anger, depression, humiliation, worry, embarrassment, social phobia, anxiety or frustration; And (3) occupational factors such as lost days of work, reduced job opportunities or pharmacoeconomic considerations.20 We speculate that the more severe the clinical symptoms of rosacea, the more the above factors are affected, so the greater the impact on the patient.
As opposed to many other diseases such as hypertension and diabetes, patients with skin diseases bear their disease for the world to see. For the patients with rosacea, the easiest point for others to notice is the facial redness and pustules, which are exacerbated by excitation such as tension and elevated temperatures, leading to psychological problems such as avoidance, low self-esteem, anxiety, and depression. However, the current treatment mainly focuses on clinical symptoms and signs, and the impact on the patient’s mood and QOL is often overlooked. Therefore, dermatologists should pay attention to the psychological state and QOL of patients, especially those with clinically severe symptoms of rosacea. A small case series suggests that cognitive-behavioral therapy conducted by an experienced clinical psychologist may help alleviate clinical symptoms in patients with severe rosacea due to social anxiety from blushing.57 By recognizing the psychosocial burden of rosacea, doctors can treat patients more comprehensively and strive for better outcomes.
Conclusion
In this way, combined disease severity and health-related QOL assessments provide a better insight into the disease burden on health status and overall functioning. The QOL was greatly impaired and should not be ignored among patients with rosacea. Clinicians should raise awareness of the rosacea-related QOL impacts, especially in patients with severe clinical symptoms. And it is recommended that patients with severe clinical symptoms of rosacea should seek psychological help.
Acknowledgments
There are no acknowledgments here.
Funding
This study was supported by Clinical Research Innovation Project, West China Hospital, Sichuan University (grant no.19HXCX010) and the National Natural Science Foundation of China (grant no.82273559).
Disclosure
The authors have no conflict of interest to declare.
References
1. Schaller M, Almeida LMC, Bewley A, et al. Recommendations for rosacea diagnosis, classification and management: update from the global ROSacea COnsensus 2019 panel. Br J Dermatol. 2020;182(5):1269–1276. doi:10.1111/bjd.18420
2. Gallo RL, Granstein RD, Kang S, et al. Standard classification and pathophysiology of rosacea: the 2017 update by the National Rosacea Society Expert Committee. J Am Acad Dermatol. 2018;78(1):148–155. doi:10.1016/j.jaad.2017.08.037
3. van Zuuren EJ, Solomon CG. Rosacea. N Engl J Med. 2017;377(18):1754–1764. doi:10.1056/NEJMcp1506630
4. Alexis AF, Callender VD, Baldwin HE, Desai SR, Rendon MI, Taylor SC. Global epidemiology and clinical spectrum of rosacea, highlighting skin of color: review and clinical practice experience. J Am Acad Dermatol. 2019;80(6):1722–9 e7. doi:10.1016/j.jaad.2018.08.049
5. Tan J, Schofer H, Araviiskaia E, et al. Prevalence of rosacea in the general population of Germany and Russia - The RISE study. J Eur Acad Dermatol Venereol. 2016;30(3):428–434. doi:10.1111/jdv.13556
6. Rueda LJ, Motta A, Pabon JG, et al. Epidemiology of rosacea in Colombia. Int J Dermatol. 2017;56(5):510–513. doi:10.1111/ijd.13491
7. Gether L, Overgaard LK, Egeberg A, Thyssen JP. Incidence and prevalence of rosacea: a systematic review and meta-analysis. Br J Dermatol. 2018;179(2):282–289. doi:10.1111/bjd.16481
8. Li J, Wang B, Deng Y, et al. Epidemiological features of rosacea in Changsha, China: a population-based, cross-sectional study. J Dermatol. 2020;47(5):497–502. doi:10.1111/1346-8138.15301
9. Rainer BM, Kang S, Chien AL. Rosacea: epidemiology, pathogenesis, and treatment. Dermatoendocrinol. 2017;9(1):e1361574. doi:10.1080/19381980.2017.1361574
10. Steinhoff M, Schauber J, Leyden JJ. New insights into rosacea pathophysiology: a review of recent findings. J Am Acad Dermatol. 2013;69(6 Suppl 1):S15–S26. doi:10.1016/j.jaad.2013.04.045
11. Woo YR, Han YJ, Kim HS, Cho SH, Lee JD. Updates on the risk of neuropsychiatric and gastrointestinal comorbidities in rosacea and its possible relationship with the Gut-Brain-Skin Axis. Int J Mol Sci. 2020;21:22. doi:10.3390/ijms21228427
12. Parkins GJ, Maan A, Dawn G. Neurogenic rosacea: an uncommon and poorly recognized entity? Clin Exp Dermatol. 2015;40(8):930–931. doi:10.1111/ced.12630
13. van Zuuren EJ, Arents BWM, van der Linden MMD, Vermeulen S, Fedorowicz Z, Tan J. Rosacea: new concepts in classification and treatment. Am J Clin Dermatol. 2021;22(4):457–465. doi:10.1007/s40257-021-00595-7
14. Thiboutot D, Anderson R, Cook-Bolden F, et al. Standard management options for rosacea: the 2019 update by the National Rosacea Society Expert Committee. J Am Acad Dermatol. 2020;82(6):1501–1510. doi:10.1016/j.jaad.2020.01.077
15. Rainer BM, Fischer AH, Luz Felipe da Silva D, Kang S, Chien AL. Rosacea is associated with chronic systemic diseases in a skin severity-dependent manner: results of a case-control study. J Am Acad Dermatol. 2015;73(4):604–608. doi:10.1016/j.jaad.2015.07.009
16. Little AC, Jones BC, DeBruine LM. Facial attractiveness: evolutionary based research. Philos Trans R Soc Lond B Biol Sci. 2011;366(1571):1638–1659. doi:10.1098/rstb.2010.0404
17. Johnston VS. Mate choice decisions: the role of facial beauty. Trends Cogn Sci. 2006;10(1):9–13. doi:10.1016/j.tics.2005.11.003
18. Zebrowitz LA, Montepare JM. Social psychological face perception: why appearance matters. Soc Personal Psychol Compass. 2008;2(3):1497. doi:10.1111/j.1751-9004.2008.00109.x
19. Halioua B, Cribier B, Frey M, Tan J. Feelings of stigmatization in patients with rosacea. J Eur Acad Dermatol Venereol. 2017;31(1):163–168. doi:10.1111/jdv.13748
20. Oussedik E, Bourcier M, Tan J. Psychosocial burden and other impacts of rosacea on patients’ quality of life. Dermatol Clin. 2018;36(2):103–113. doi:10.1016/j.det.2017.11.005
21. Bewley A, Fowler J, Schofer H, Kerrouche N, Rives V. Erythema of rosacea impairs health-related quality of life: results of a meta-analysis. Dermatol Ther. 2016;6(2):237–247. doi:10.1007/s13555-016-0106-9
22. Huang Y, Yan S, Xie H, et al. Health related quality of life of rosacea patients in china assessed by dermatology life quality index and willingness to pay. Patient Prefer Adherence. 2022;16:659–670. doi:10.2147/PPA.S345258
23. Moustafa F, Lewallen RS, Feldman SR. The psychological impact of rosacea and the influence of current management options. J Am Acad Dermatol. 2014;71(5):973–980. doi:10.1016/j.jaad.2014.05.036
24. Egeberg A, Hansen PR, Gislason GH, Thyssen JP. Patients with rosacea have increased risk of depression and anxiety disorders: a Danish Nationwide Cohort Study. Dermatology. 2016;232(2):208–213. doi:10.1159/000444082
25. Tan J, Liu H, Leyden JJ, Leoni MJ. Reliability of Clinician Erythema Assessment grading scale. J Am Acad Dermatol. 2014;71(4):760–763. doi:10.1016/j.jaad.2014.05.044
26. Seo JK, Shin EJ, Jeong KH, Shin MK. Clinician severity assessment grading scale on erythematotelangiectatic rosacea. Indian J Dermatol. 2021;66(2):203–205. doi:10.4103/ijd.IJD_611_19
27. Zhao S, Wang M, Zhou Y, Yan Y. The therapeutic effects in patients with rosacea: how do we evaluate them? J Cosmet Dermatol. 2022;21(2):506–512. doi:10.1111/jocd.14713
28. Hongbo Y, Thomas CL, Harrison MA, Salek MS, Finlay AY. Translating the science of quality of life into practice: what do dermatology life quality index scores mean? J Invest Dermatol. 2005;125(4):659–664. doi:10.1111/j.0022-202X.2005.23621.x
29. Finlay AY, Khan GK. Dermatology Life Quality Index (DLQI)--a simple practical measure for routine clinical use. Clin Exp Dermatol. 1994;19(3):210–216. doi:10.1111/j.1365-2230.1994.tb01167.x
30. Nicholson K, Abramova L, Chren MM, Yeung J, Chon SY, Chen SC. A pilot quality-of-life instrument for acne rosacea. J Am Acad Dermatol. 2007;57(2):213–221. doi:10.1016/j.jaad.2007.01.048
31. Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand. 1983;67(6):361–370. doi:10.1111/j.1600-0447.1983.tb09716.x
32. Cassiani-Miranda CA, Scoppetta O, Cabanzo-Arenas DF. Validity of the Hospital Anxiety and Depression Scale (Hads) in primary care patients in Colombia. Gen Hosp Psychiatry. 2022;74:102–109. doi:10.1016/j.genhosppsych.2021.01.014
33. Julian LJ. Measures of anxiety: State-Trait Anxiety Inventory (STAI), Beck Anxiety Inventory (BAI), and Hospital Anxiety and Depression Scale-Anxiety (Hads-A). Arthritis Care Res. 2011;63(Suppl 11):S467–S472. doi:10.1002/acr.20561
34. The WHOQOL Group. Development of the World Health Organization WHOQOL-BREF quality of life assessment. Psychol Med. 1998;28(3):551–558. doi:10.1017/S0033291798006667
35. Silverberg JI, Gelfand JM, Margolis DJ, et al. Patient burden and quality of life in atopic dermatitis in US adults: a population-based cross-sectional study. Ann Allergy Asthma Immunol. 2018;121(3):340–347. doi:10.1016/j.anai.2018.07.006
36. Korman NJ, Zhao Y, Pike J, Roberts J. Relationship between psoriasis severity, clinical symptoms, quality of life and work productivity among patients in the USA. Clin Exp Dermatol. 2016;41(5):514–521. doi:10.1111/ced.12841
37. Kirby JS, Butt M, Esmann S, Jemec GBE. Association of resilience with depression and health-related quality of life for patients with hidradenitis suppurativa. JAMA Dermatol. 2017;153(12):1263–1269. doi:10.1001/jamadermatol.2017.3596
38. Sun Q, Ren I, Zaki T, Maciejewski K, Choate K. Ichthyosis affects mental health in adults and children: a cross-sectional study. J Am Acad Dermatol. 2020;83(3):951–954. doi:10.1016/j.jaad.2020.01.052
39. Tan J, Beissert S, Cook-Bolden F, et al. Impact of facial atrophic acne scars on quality of life: a multi-country population-based survey. Am J Clin Dermatol. 2022;23(1):115–123. doi:10.1007/s40257-021-00628-1
40. Finlay AY, Salek MS, Abeni D, et al. Why quality of life measurement is important in dermatology clinical practice: an expert-based opinion statement by the EADV Task Force on Quality of Life. J Eur Acad Dermatol Venereol. 2017;31(3):424–431. doi:10.1111/jdv.13985
41. Tan J, Almeida LM, Bewley A, et al. Updating the diagnosis, classification and assessment of rosacea: recommendations from the global ROSacea COnsensus (ROSCO) panel. Br J Dermatol. 2017;176(2):431–438. doi:10.1111/bjd.15122
42. van der Linden MM, van Rappard DC, Daams JG, Sprangers MA, Spuls PI, Korte J. and de Korte J. Health-related quality of life in patients with cutaneous rosacea: a systematic review. Acta Derm Venereol. 2015;95(4):395–400. doi:10.2340/00015555-1976
43. Holmes AD, Spoendlin J, Chien AL, Baldwin H, Chang ALS. Evidence-based update on rosacea comorbidities and their common physiologic pathways. J Am Acad Dermatol. 2018;78(1):156–166. doi:10.1016/j.jaad.2017.07.055
44. Incel Uysal P, Akdogan N, Hayran Y, Oktem A, Yalcin B. Rosacea associated with increased risk of generalized anxiety disorder: a case-control study of prevalence and risk of anxiety in patients with rosacea. An Bras Dermatol. 2019;94(6):704–709. doi:10.1016/j.abd.2019.03.002
45. Spoendlin J, Bichsel F, Voegel JJ, Jick SS, Meier CR. The association between psychiatric diseases, psychotropic drugs and the risk of incident rosacea. Br J Dermatol. 2014;170(4):878–883. doi:10.1111/bjd.12734
46. Hung CT, Chiang CP, Chung CH, Tsao CH, Chien WC, Wang WM. Risk of psychiatric disorders in rosacea: a nationwide, population-based, cohort study in Taiwan. J Dermatol. 2019;46(2):110–116. doi:10.1111/1346-8138.14705
47. Gupta MA, Gupta AK, Chen SJ, Johnson AM. Comorbidity of rosacea and depression: an analysis of the National Ambulatory Medical Care Survey and National Hospital Ambulatory Care Survey--Outpatient Department data collected by the U.S. National Center for Health Statistics from 1995 to 2002. Br J Dermatol. 2005;153(6):1176–1181. doi:10.1111/j.1365-2133.2005.06895.x
48. Böhm D, Schwanitz P, Stock Gissendanner S, Schmid-Ott G, Schulz W. Symptom severity and psychological sequelae in rosacea: results of a survey. Psychol Health Med. 2014;19(5):586–591. doi:10.1080/13548506.2013.841968
49. Chen M, Deng Z, Huang Y, Li J. Prevalence and risk factors of anxiety and depression in rosacea patients: a cross-sectional study in China. Front Psychiatry. 2021;12:659171. doi:10.3389/fpsyt.2021.659171
50. Arck P, Handjiski B, Hagen E, et al. Is there a ‘gut-brain-skin axis’? Exp Dermatol. 2010;19(5):401–405. doi:10.1111/j.1600-0625.2009.01060.x
51. Koopman M. and El Aidy S. Depressed gut? The microbiota-diet-inflammation trialogue in depression. Curr Opin Psychiatry. 2017;30(5):369–377. doi:10.1097/YCO.0000000000000350
52. Buhl T, Sulk M, Nowak P, et al. Molecular and morphological characterization of inflammatory infiltrate in rosacea reveals activation of Th1/Th17 pathways. J Invest Dermatol. 2015;135(9):2198–2208. doi:10.1038/jid.2015.141
53. Maes M. Depression is an inflammatory disease, but cell-mediated immune activation is the key component of depression. Prog Neuropsychopharmacol Biol Psychiatry. 2011;35(3):664–675. doi:10.1016/j.pnpbp.2010.06.014
54. Beurel E, Toups M, Nemeroff CB. The bidirectional relationship of depression and inflammation: double trouble. Neuron. 2020;107(2):234–256. doi:10.1016/j.neuron.2020.06.002
55. Amir Ali A, Vender R, Vender R. The role of IL-17 in papulopustular rosacea and future directions. J Cutan Med Surg. 2019;23(6):635–641. doi:10.1177/1203475419867611
56. Kini SP, Nicholson K, DeLong LK, et al. A pilot study in discrepancies in quality of life among three cutaneous types of rosacea. J Am Acad Dermatol. 2010;62(6):1069–1071. doi:10.1016/j.jaad.2009.08.020
57. Su D, Drummond PD. Blushing propensity and psychological distress in people with rosacea. Clin Psychol Psychother. 2012;19(6):488–495. doi:10.1002/cpp.763
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
