Back to Journals » Diabetes, Metabolic Syndrome and Obesity » Volume 15
A Cross-Sectional Study of Serum Ferritin Levels in Vietnamese Adults with Metabolic Syndrome
Authors Tran TN, Tran HD, Tran-Huu TT , Tran DM, Tran QN
Received 31 January 2022
Accepted for publication 4 May 2022
Published 12 May 2022 Volume 2022:15 Pages 1517—1523
DOI https://doi.org/10.2147/DMSO.S360689
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Antonio Brunetti
Thua Nguyen Tran,1 Huu Dang Tran,2 Thanh Tung Tran-Huu,2 Duc Minh Tran,1 Quang Nhat Tran1
1Department of General Internal Medicine and Geriatrics, Hue Central Hospital, Hue City, Vietnam; 2Department of Internal Medicine, Hue University of Medicine and Pharmacy, Hue City, Vietnam
Correspondence: Thua Nguyen Tran, Department of General Internal Medicine and Geriatrics, Hue Central Hospital, 16 Le Loi Street, Hue City, 530000, Vietnam, Tel +84903597695, Email [email protected]
Background: Metabolic syndrome is one of the most common public health concerns in the 21st century. Several previous studies have shown an association between increased serum ferritin levels and other components of metabolic syndrome and the risk of metabolic syndrome. They conclude that ferritin can be viewed as a predictor of metabolic syndrome risk. This study investigates some main features of metabolic syndrome and the serum ferritin levels in a Vietnamese adult cohort with metabolic syndrome.
Methods: A descriptive cross-sectional study was conducted on 207 patients who were treated at the General Internal Medicine-Geriatric Department, Hue Central Hospital, from May 2018 to August 2020. Patients were divided into two groups: the study group (104 patients with metabolic syndrome) and the control group (103 patients without metabolic syndrome and no serum ferritin-mediated disease). The metabolic syndrome was diagnosed by a joint interim statement of the International Diabetes Federation/American Heart Association/National Heart, Lung, and Blood Institute/World Heart Federation/International Atherosclerosis Society/International Association for the Study of Obesity in 2009.
Results: Hypertriglyceridemia–hypertension–hyperglycemia (50.9%) is the most common combination of metabolic syndrome components. The mean serum ferritin concentration was 391.62± 181.97ng/mL and 124.55± 63.95ng/mL in the metabolic syndrome and control groups, respectively. In the metabolic syndrome group, increased ferritin concentration accounted for 86.54% for men, the mean serum ferritin concentration was 453.064 ± 161.75ng/mL (increased ferritin concentration accounted for 96.15%) for women; the mean serum ferritin concentration was 330.17 ± 181.71 ng/mL (increased ferritin concentration accounted for 86.54%).
Conclusion: The serum ferritin level is significantly increased in Vietnamese patients with metabolic syndrome.
Keywords: metabolic syndrome, ferritin, hypertension
Background
Metabolic syndrome is one of the most concerning public health problems in the twenty-first century worldwide.1 According to the National Health Nutrition Examination Survey III, metabolic syndrome involves about 24% of adults, about 47 million with metabolic syndrome, of which 44% are over 50 in the United States.2 Serum ferritin is an iron-carrying protein that exists both inside and outside the cell and is found almost everywhere in the body, such as liver, spleen, marrow, duodenum, striatum, and many other anatomical areas. It can store and releases iron and acts as a buffer against iron deficiency and iron overload. In the absence of any identifiable cause of iron excess, dysmetabolic iron overload syndrome is associated with various components of metabolic syndrome.3 Many studies around the world have shown an association between increased serum ferritin levels and other components of metabolic syndrome as well as the risk of metabolic syndrome,4–6 studies have come to some conclusion that ferritin can be viewed as a predictor of metabolic syndrome risk.7,8 The meta-analysis study of Suarez-Ortegón et al showed that there was a significant overall positive association between ferritin and metabolic syndrome. Hepatic injury, body mass index (BMI), and type of ferritin assay appear to influence the ferritin- metabolic syndrome association.9 Up to now, there is a lack of reports on the relationship between ferritin and metabolic syndrome in Vietnam. Therefore, we carried out this study to investigate some main features of metabolic syndrome and the ferritin levels in a Vietnamese adult cohort with metabolic syndrome.
Materials and Methods
A cross-sectional descriptive study was carried out on 207 patients at the General Internal Medicine - Geriatrics Department, Hue Central Hospital, from May 2018 to August 2020. All participants were informed about the purpose of the study. Written consent was obtained from all participants before data collection. The patients were classified into two groups: the study group (104 patients) and the control group (103 patients).
The inclusion criteria for the study group were patients aged ≥18 years diagnosed with metabolic syndrome.
Diagnosis of metabolic syndrome must be fulfilled at least 3 out of 5 following criteria of International Diabetes Federation (IDF)/American Heart Association (AHA)/ National Heart, Lung, and Blood Institute (NHLBL)/ World Heart Federation (WHF)/International Atherosclerosis Society (IAS)/ International Association for the Study of Obesity (IASO) 200910 (Table 1).
 |
Table 1 Diagnostic Criteria for Metabolic Syndrome According to IDF/AHA/NHLBL/WHF/IAS/IASO-2009.10 |
The inclusion criteria for the control group were patients without metabolic syndrome and no serum ferritin-mediated disease.
The exclusion criteria for both groups were patients with: (1) a history of chronic liver diseases or chronic kidney diseases; (2) a history of iron metabolism disorder; (3) those with anemia or infectious diseases; (4) those using iron supplements; (5) pregnant women.
All patients in both groups underwent detailed physical and clinical examinations. Their anthropometric measurements like height, weight, and waist circumference were measured using standard procedures and techniques. Serum ferritin level was performed by using an automated Chemiluminescence Immunoassay system. The normal range of serum ferritin defined at Hue Central Hospital laboratory was 12–280 ng/mL (male) and 12–150 ng/mL (female). Other blood tests (blood lipid, blood glucose) were done simultaneously as the serum ferritin test.
All data were statistically analyzed using SPSS version 18.0 (SPSS, Chicago, USA). The distributions of the participant characteristics were converted into percentages, and the successive data were presented as mean values with standard deviations. The mean value difference in serum ferritin levels for characteristics of the subjects and the metabolic syndrome components were calculated using an independent t-test and analysis of variance (ANOVA). The significance level for all of the statistical data was set as p<0.05.
Results
Table 2 shows the characteristics of age and gender. The average age of the study group was higher than the control group (66.36 ± 14.74 vs 60.02 ± 19.06). This gap was clearer in the female group (67.88 ± 11.98 vs 57.88 ± 19.07, p<0.001), the difference in male patient’s age in the two groups was not significant (p=0.4136).
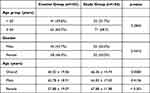 |
Table 2 Characteristics of Age and Gender Distribution |
The rate of central obesity in the group with metabolic syndrome was 58.7%, men accounted for 17.26%, and women accounted for 40.74%; meanwhile, the average BMI value was 21.60 ± 2.68. The BMI group from 18.5 to 22.9 had the highest rate of 61.4%. The group with BMI ≥ 25 kg/m2 accounted for 9.2%.
In anthropometric indicators of the two groups, only the difference in waist circumference had statistical significance; the average waist circumference in the study group was higher than the control group (Table 3). This difference was shown in the male group (85.13 ± 5.24 vs 79.78 ± 3.87, p<0.001) and female group (80.96 ± 3.42 vs 76.93 ± 4.68, p<0.001). The difference in height, weight, and BMI between the two groups was not significant.
 |
Table 3 Anthropometric Indicators by Gender for 2 Groups with and without Metabolic Syndrome |
Table 4 presents the ratio of the components of the metabolic syndrome. The prevalence of all components of the metabolic syndrome in the study group was higher than in the control group. The prevalence of hypertension, increased triglycerides, and increased fasting blood glucose in the study group were 90.38%, 84.62%, and 75.96%, while those in the control group were 9.70%, 16.59%, and 18.45. The prevalence of Reduced HDL-C and central obesity in the study group was 58.65% and 58.7%; these rates in the control group were 32.04% and 16.5%.
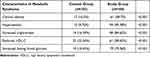 |
Table 4 The Ratio of the Components of the Metabolic Syndrome |
Most of the patients in the study group had an increased serum ferritin level (91.35%). In comparison, this rate in the control group was significantly less than a quarter of patients (24.26%) (Table 5).
 |
Table 5 Serum Ferritin Status in the Study Group |
In the patients with Increased serum ferritin in the control group, the number of female patients was higher than male patients (14 patients vs 11 patients), but in the study group, the number of male patients with Increased serum ferritin was higher than female patients (50 patients vs 45 patients).
The control group had a lower mean serum ferritin concentration than the study group. This difference also presented in both patient gender of the two groups, the mean serum ferritin concentration of male patients and female patients in the control group was lower than in the study group.
The average serum ferritin level of the control group was 124.55 ± 63.95 compared with the study group, all of the groups with any three common metabolic syndrome components’ s average serum ferritin level was higher than the control group with high statistical significance (p<0.001), the highest average serum ferritin level was in increased G – increased TG – hypertension group (399.11 ± 177.62), and the lowest one was in increased G – increased waist circumference – hypertension group (346.24 ± 173.88) (as shown in Table 6).
 |
Table 6 Mean Serum Ferritin Concentration of the Group of 3 Common Metabolic Syndrome Components |
Discussion
General Characteristics of Research Subjects
The older you get, the higher your risk of diseases, including metabolic syndrome. Many domestic and foreign studies have concluded that the metabolic syndrome increases gradually with age and increases significantly after 50, with the greatest concentration from 50–70 years old.4 According to Ledesma et al (2015), the study on 3386 subjects with the average age of metabolic syndrome was 52.2 ± 5.2.11 The results of our study showed that the age of the disease group was 66.36 ± 14.74 years old, and the control group was 60.02 ± 19.06 years old. The difference in age between the two groups was statistically significant.
Women are less active than men, menstruation, maternity, especially menopause, and a lack of estrogen, risk factors for insulin resistance and metabolic syndrome. Some epidemiological studies on metabolic syndrome in Vietnam show that the proportion of women with metabolic syndrome is higher than that of men.12,13 In our study, the equal rate of men and women with the metabolic syndrome was 50%; the reason may be that the number of metabolic syndrome patients we studied was only 104, which was not representative of the population in Hue – Vietnam.
Waist circumference is an important component of metabolic syndrome. It is considered a useful screening tool for diagnosing metabolic syndrome in men and women, and waist circumference has been adjusted to match race and Asian region. For example, the average waist circumference for Chinese was 84.34 ± 0.16 cm for men and 81.27 ± 0.15 cm for women,;14 in Vietnam, according to the study by Le et al, the average waist circumference of Polycystic Ovary Syndrome women with metabolic syndrome was 84.33±8.84 cm.15 In our study, the average waist circumference in men with metabolic syndrome was 85.13 ± 5.24 cm and in the controlled group was 79.78 ± 43.87 cm. In women with the metabolic syndrome was 80.96 ± 3.42 cm and in the control group was 76.93 ± 4.68 cm.
Metabolic Syndrome Components and Serum Ferritin Concentrations in Subjects with Metabolic Syndrome
According to the 2009 consensus, all five factors contribute to the diagnosis of metabolic syndrome, including central obesity, increased TG, decreased HDL-C, increased G0, and increased blood pressure. However, the most prominent components of metabolic syndrome are different in each region. For example, in the study of Sigit, the most prominent components were hypertension (61%) and hyperglycemia (51%) in the Indonesians, and hypertension (62%) and abdominal obesity (40%) in the Dutch population,16 The study of Shahbazian showed the rate: increased waist circumference 29.4%, increased TG by 40.7%, reduced HDL-C 40.2%, hypertension 15.4%, hyperglycemia was 37.8%.17 In our study, the results in the group with metabolic syndrome: hypertension accounted for the highest rate of 90.38%, followed by increased TG at 84.62%, increased G0 at 75.96%, and increased waist circumference was 58.7%, and decreased HDL-C was 58.65%. In the control group, reduced HDL-C was 32.04%, followed by an increased blood glucose of 18.45%, increased TG of 16.59%, central obesity of 16.5%, and hypertension of 9.70%. The rate of central obesity, increased TG, decreased HDL-C, hypertension, and increased G0 in the group with metabolic syndrome were statistically significantly higher than in the control group (p <0.001).
According to a study of Sirinapa Siwarom, the most common combination of Thailand people is waist circumference, low HDL-C, and triglyceride criteria.18 On the other hand, the common combination of metabolic syndrome in our study is hyperglycemia–hypertriglyceridemia–hypertension, with 53 cases (50.9%). Other common forms were increased TG - increased blood pressure - decreased HDL-C, increased abdominal circumference - increased TG - increased blood pressure. This difference can be attributed to the differences in living and eating habits of people in Vietnam compared to those of other countries reported in studies.
Characteristics of Ferritin Concentrations in Subjects with Metabolic Syndrome
In healthy people, serum ferritin of elderly people is lower than younger people.19 Still, it is not the same with metabolic syndrome patients. Ledesma al (2015) studied 3386 subjects with metabolic syndrome; the mean ferritin concentration was 201.4 ± 114.2 and increased gradually with age.11 According to our study, the rate of metabolic syndrome increased with increasing ferritin concentration compared with the age group over 60 years old, accounting for 68.3% higher than the group under 60 years old, 31.7%.
Many studies have focused on the association between serum ferritin and metabolic syndrome in recent years. There is a positive association between elevated serum ferritin and metabolic syndrome and its components.5,6 According to Päivi Hämäläinen, Increases in serum ferritin over 6.5 years were associated with the development of Metabolic syndrome in both men and women.20 In our study, the mean concentration of total ferritin in the metabolic syndrome group, was 391.63 ± 181.97ng/mL, statistically significantly higher than the total ferritin concentration in the control group. 124.55 ± 63.95ng/mL, p <0.01, and the mean concentration ferritin level of male patients and female patients in the metabolic syndrome group were also higher than those of the same gender in the control group.
Conclusion
In Vietnamese adults with metabolic syndrome, increased glucose - Increased TG – Hypertension is the most common combination of components of metabolic syndrome, which also has the highest average serum ferritin level. The most common component of metabolic syndrome is hypertension.
In the same exclusion criteria, the rate of increased serum ferritin and serum ferritin levels in patients with metabolic syndrome were higher than in those without metabolic syndrome.
Ethics Statements
The study protocol was approved by the Ethics Committee of Hue Central Hospital in accordance with the principles of the Helsinki Declaration and written informed consent was obtained from each subject.
Disclosure
The authors have declared that no competing interest exists in this work.
References
1. Shaw JE, Sicree RA, Zimmet PZ. Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Res Clin Pract. 2010;87(1):4–14. doi:10.1016/j.diabres.2009.10.007
2. Ford ES, Giles WH, Dietz WH. Prevalence of the metabolic syndrome among US adults: findings from the third National Health and Nutrition Examination Survey. JAMA. 2002;287(3):356–359. doi:10.1001/jama.287.3.356
3. Deugnier Y, Laine F. [Dysmetabolic iron overload syndrome: a systemic disease?]. Presse medicale. 2014;43(6 Pt 1):625–627. doi:10.1016/j.lpm.2014.03.008
4. Tang Q, Liu Z, Tang Y, et al. High serum ferritin level is an independent risk factor for metabolic syndrome in a Chinese male cohort population. Diabetol Metab Syndr. 2015;7:11. doi:10.1186/s13098-015-0004-9
5. Wang M, Zhao A, Szeto IM, et al. Association of serum ferritin with metabolic syndrome in eight cities in China. Food Sci Nutr. 2020;8(3):1406–1414. doi:10.1002/fsn3.1408
6. Jehn M, Clark JM, Guallar E. Serum ferritin and risk of the metabolic syndrome in U.S. adults. Diabetes Care. 2004;27(10):2422–2428. doi:10.2337/diacare.27.10.2422
7. Yi KH, Hwang JS, Lim SW, Lee JA, Kim DH, Lim JS. Ferritin level is associated with metabolic syndrome and elevated alanine aminotransferase in children and adolescents. J Pediatric Endocrinol Metab. 2016;29(12):1337–1344. doi:10.1515/jpem-2016-0045
8. Fang X, Min J, Wang F. A dose-response association between serum ferritin and metabolic syndrome? Atherosclerosis. Dec. 2018;279:130–131.
9. Suarez-Ortegon MF, Ensaldo-Carrasco E, Shi T, McLachlan S, Fernandez-Real JM, Wild SH. Ferritin, metabolic syndrome and its components: a systematic review and meta-analysis. Atherosclerosis. 2018;275:97–106. doi:10.1016/j.atherosclerosis.2018.05.043
10. Alberti KG, Eckel RH, Grundy SM, et al. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009;120(16):1640–1645. doi:10.1161/CIRCULATIONAHA.109.192644
11. Ledesma M, Hurtado-Roca Y, Leon M, et al. Association of ferritin elevation and metabolic syndrome in males. Results from the Aragon Workers’ Health Study (AWHS). J Clin Endocrinol Metab. 2015;100(5):2081–2089. doi:10.1210/jc.2014-4409
12. Binh TQ, Phuong PT, Nhung BT, Tung Do D. Metabolic syndrome among a middle-aged population in the Red River Delta region of Vietnam. BMC Endocr Disord. 2014;14:77. doi:10.1186/1472-6823-14-77
13. Pham DT, Nguyen HT. Prevalence of Metabolic Syndrome in Rural Areas of Vietnam: a Selected-Randomized Study. Arch Pharmacy Practice. 2019;10(2):43–50.
14. Han LL, Wang YX, Li J, et al. Gender differences in associations of serum ferritin and diabetes, metabolic syndrome, and obesity in the China Health and Nutrition Survey. Mol Nutr Food Res. 2014;58(11):2189–2195. doi:10.1002/mnfr.201400088
15. Le MT, Nguyen VQH, Truong QV, Le DD, Le VNS, Cao NT. Metabolic Syndrome and Insulin Resistance Syndrome among Infertile Women with Polycystic Ovary Syndrome: a Cross-Sectional Study from Central Vietnam. Endocrinol Metab. 2018;33(4):447–458. doi:10.3803/EnM.2018.33.4.447
16. Sigit FS, Tahapary DL, Trompet S, et al. The prevalence of metabolic syndrome and its association with body fat distribution in middle-aged individuals from Indonesia and the Netherlands: a cross-sectional analysis of two population-based studies. Diabetol Metab Syndr. 2020;12:2. doi:10.1186/s13098-019-0503-1
17. Shahbazian H, Latifi SM, Jalali MT, et al. Metabolic syndrome and its correlated factors in an urban population in South West of Iran. J Diabetes Metab Disord. 2013;12(1):11. doi:10.1186/2251-6581-12-11
18. Siwarom S, Aekplakorn W, Pirojsakul K, et al. Metabolic syndrome in Thai adolescents and associated factors: the Thai National Health Examination Survey V (NHES V). BMC Public Health. 2021;21(1):678. doi:10.1186/s12889-021-10728-6
19. Worwood M. Indicators of the Iron Status of Populations: Ferritin. Vol. 2. Geneva (Switzerland): Joint World Health Organization/Centers for Disease Control and Prevention Technical Consultation on the Assessment of Iron Status at the Population Level; 2007.
20. Hamalainen P, Saltevo J, Kautiainen H, Mantyselka P, Vanhala M. Serum ferritin levels and the development of metabolic syndrome and its components: a 6.5-year follow-up study. Diabetol Metab Syndr. 2014;6(1):114. doi:10.1186/1758-5996-6-114
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
