Back to Journals » Infection and Drug Resistance » Volume 13
A Confirmed Catheter-Related Blood Stream Infection (CRBSI) in an Immunocompetent Patient Due to Myroides odoratimimus: Case Report and Literature Review
Authors Lu Y , Xia W , Zhang X , Ni F, Mei Y
Received 15 October 2019
Accepted for publication 17 December 2019
Published 10 January 2020 Volume 2020:13 Pages 139—144
DOI https://doi.org/10.2147/IDR.S234778
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Joachim Wink
Yanfei Lu, 1, 2,* Wenying Xia, 1, 2,* Xiaohui Zhang, 1, 2,* Fang Ni, 1, 2 Yaning Mei 1, 2
1Department of Laboratory Medicine, Jiangsu Province Hospital and Nanjing Medical University First Affiliated Hospital, Nanjing, People’s Republic of China; 2National Key Clinical Department of Laboratory Medicine, Nanjing, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Fang Ni; Yaning Mei
Department of Laboratory Medicine, Jiangsu Province Hospital, Guangzhou Street No. 300, Nanjing 210029, People’s Republic of China
Tel +86 25-6830-6287
Fax +86 25- 8372-4440
Email [email protected]; [email protected]
Abstract: The genus Myroides are gram-negative bacilli which are completely aerobic, non-motile, non-fermenting and yellow-pigmented with a characteristic fruity odor. Myroides species are widely found in the environment, especially in water and soil, and are considered as low-grade opportunistic pathogens for humans. Myroides infections are most commonly seen in immunocompromised patients and only rarely occur in immunocompetent patients. We here report the first confirmed catheter-related bloodstream infection (CRBSI) due to Myroides odoratimimus in an immunocompetent patient. We also review the literature related to Myroides infections.
Keywords: Myroides odoratimimus, CRBSI, immunocompetent patient
Introduction
Myroides species originally classified as Flavobacterium odoratum,1 they were renamed Myroides in 1996 because of the difference for genotypic and phenotypic data such as nonmotile, good growth at 37°C, halotolerance, and difference in the fatty acid profile.2 The two best-known species are Myroides odoratus and Myroides odoratimimus.1 They are commonly found in the environment, rarely infect humans, but the incidence of Myroides infections has increased in recent years. These infections usually occur in immunocompromised patients, including those with diabetes mellitus, cirrhosis, chronic obstructive pulmonary disease, renal failure, or prolonged corticosteroid therapy,3 with soft tissue infections and urinary tract infections being the most common types. However, infections in immunocompetent hosts have also been described and are occasionally life-threatening.1 We here report a confirmed CRBSI in an immunocompetent patient due to Myroides odoratimimus. Clinicians must be alert to the possibility that this genus can be highly pathogenic even in immunocompetent hosts. Written informed consent was provided by the patient to allow the case details to be published, and our study was approved by the Ethics Committee at Jiangsu Province Hospital.
Case Report
A 48-year-old female presented to our emergency department 2 days after cardiopulmonary resuscitation (CPR). Two days before, the patient suffered a sudden loss of consciousness, with a pale face, salivation at the corners for the mouth, and urinary incontinence, but without nausea, vomiting, or limb twitching. She was immediately admitted to the local hospital resuscitation room. At that time, her blood pressure was as high as 160/103 mmHg while her heart rate dropped to 12 beats per minute, and the electrocardiogram showed third-degree atrioventricular block, serum potassium was only 2.59 mmol/L. There was no significant past medical history other than diarrhea before her loss of consciousness. The patient immediately underwent a series of rescue measures and a temporary pacemaker was implanted to adjust the heart at 60 beats per minute due to her recurrent cardiac and respiratory arrest. Additionally, a chest CT scan revealed exudative lesions in the lungs bilaterally while a head CT scan showed no abnormality. Shortly thereafter, she was transferred to the intensive care unit (ICU) with stable vital signs.
The patient was subsequently admitted to our hospital for further treatment. Upon clinical examination, her temperature was 39.5°C; blood pressure, 92/45 mmHg; heart rate, 60 beats/minute; and respiratory rate, 23 breaths per minute. Physical examination revealed a placed trachea intubation with external mechanically ventilating, an appendectomy incision at the right McBurney’s point, a temporary cardiac pacing catheter at the ipsilateral groin, and a left femoral vein catheterization in place. Laboratory values included a white blood count of 36,610/µL (normal, 4000–10,000) with 88% neutrophils, procalcitonin 4.31 ng/mL (normal, 0–0.05), pro-B type natriuretic peptide 6072 pg/mL (normal, 0–125), hypersensitive troponin T (hs-TropT) 115.5 ng/L (normal, 0–14), ALT 331.5 U/L (normal, 7.0–40.0), and AST 272 U/L (normal, 13.0–35.0). The initial diagnoses of cardiac respiratory arrest, post-CPR syndrome, and third-degree atrioventricular block were put forward and broad empirical therapy with imipenem and vancomycin was initiated.
Three days after hospitalization, the temperature of the patient rose as high as 40.5°C and inflammation indexes were significantly elevated. The left femoral vein catheter was considered to be a possible infection source and therefore removed; the catheter, catheter blood and venous blood cultures were sent for microbiological examination in view of the deteriorating clinical picture.
After 14 h of culture, gram-negative rods were detected from both aerobic blood culture bottles (BACTEC FX, BD Becton, Dickinson and Company) and colistin was applied. Strains were isolated from blood, chocolate, and MacConkey Agar after 24h of incubation in aerobic conditions, which were round, yellow pigmented, non-fermentative, and had a fruity odor. Initial identification of Myroidesspp. was performed using a VITEK2 (BioMerieux) automated system and subsequently confirmed by matrix-assisted laser desorption ionization-time-of-flight mass spectrometry (MALDI-TOF-MS) (BioMerieux) with 99% confidence. Definitive identification was accomplished via 16SrRNA gene sequencing, revealing a 1474-score homology with Myroides odoratimimus. The same organism was isolated from both the left femoral vein catheter and catheter blood, and the positive time of catheter blood culture was earlier than venous blood. Accordingly, a diagnosis of catheter-related bloodstream infection (CRBSI) was confirmed. In the meantime, the patient developed septic shock.
Antimicrobial susceptibility tests (AST) were carried out by automated microdilution broth test (VITEK2, BioMerieux) and interpreted following CLSI M100 guidelines (2019), using the minimum inhibitory concentration (MIC) breakpoints of other non-Enterobacteriaceae and cefoperazone/sulbactam referred to the breakpoint of cefoperazone. The in vitro susceptibility testing of the isolate proved it resistant to the majority of agents tested (i.e., piperacillin, piperacillin/tazobactam, ceftazidime, ceftriaxone, cefepime, aztreonam, imipenem, meropenem, amikacin, gentamicin, tobramycin, ciprofloxacin, levofloxacin, and trimethoprim/sulfamethoxazole), with susceptibility solely to cefoperazone/sulbactam (Table 1). Based on that finding, the patient’s antibiotic treatment was changed to a combination of cefoperazone/sulbactam (1g IV qd) and levofloxacin (3g IV q6h).
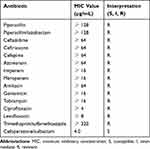 |
Table 1 In vitro Susceptibility of the Myroides odoratimimus Isolate |
After 5 days on the regimen, the infection of CRBSI was under control and no causative organism could be detected in blood culture. The patient had cardiac respiratory arrest again during the time of hospitalization, and a temporary pacemaker was reinstalled. Coronary angiography (CAG) showed the patient had a coronary myocardial bridge, for which a permanency cardiac pacemaker should be considered when the patient stabilizes. Afterwards, the patient was transferred to local hospital for rehabilitation.
Discussion
CRBSI have been increased in recent years due to the widespread use of invasive operations. The most common pathogenic bacteria reported to cause CRBSI were coagulase-negative Staphylococcus (especially Staphylococcus epidermidis), followed by Staphylococcus aureus, Candidaspp. and Enterococcus.4 CRBSI with Myroidesspp. were rarely described. Douce et al reported an outbreak of central venous CRBSI due to contaminated ampoules of water for injection.5 There were another four CRBSI cases reported in cancer patients.6 A case involving a baboon after a porcine kidney graft had a CRBSI because of this genus.7 Among the cases published, our case is the first confirmed CRBSI in immunocompetent patients. Clinical attention should be paid to this emerging pathogen causing CRBSI.
Myroides species have been cultured from blood,3 urine,8 soft tissue,9 bronchoalveolar lavage,10 sputum,11 bile,12 pus13 and pericardial fluid,14 although rarely isolated from clinical specimens. They have also been found in seafood products, meat-processing, flesh flies, grey mullet’s gut, livestock manure, Sagor catfish, and boar semen,15–18 bacteria existing in these non-human hosts may have some connection with the transmission of the pathogen. Myroides infections include cellulitis, urinary tract infection (UTI), bacteremia, necrotizing fasciitis, pneumonia, pericarditis endocarditis, ventriculitis, acalculous cholecystitis, urosepsis, empyema and canaliculitis as well as nosocomial outbreaks.8,12,13,19 Myroides odoratus and Myroides odoratimimus are the two main species of the genus to cause corresponding infections. Myroides odoratus strains are associated with septic soft tissue infections, whereas Myroides odoratimimus is described in cases of urinary infections,20 but not absolutely. Patients infected with Myroides are generally cured or improved, but occasional life-threatening cases have been reported.14,19
Besides the most two common species mentioned above, a series of new species have been identified with the development of molecular techniques and are detailed in Table 2.21–29 These uncommon species apparently do well in both aquatic and soil environments, which are mainly isolated from seawater and soil,21,25 and have not to date been documented as a source of infections in humans except for the species of Myroides injenensis which caused bacteremia and severe cellulitis.30
 |
Table 2 New Species of the Myroides |
Myroidesspp. is not traditionally normal human flora and they are usually considered to be low-grade opportunistic pathogens, Myroidesspp. infection is strongly associated with immunocompromised patients.31 There are some infection cases reported in these hosts.8,11,14,16,31,32 Those infected with the organisms often have underlying diseases such as diabetes mellitus, cirrhosis, chronic obstructive pulmonary disease, renal failure, chemotherapy, immunosuppression for transplantation and prolonged corticosteroid therapy,3,30 which may damage the body’s immunity and make human susceptible to Myroides infections. However, immunocompetent hosts can also be infected although rarely reported.10 We found only six isolated cases of Myroidesspp. infection in immunocompetent hosts (including our case), summarized in Table 3.1,9,10,33,34 Increasing cases in immunocompetent hosts have been published in recent 10 years, four cases were caused by Myroides odoratimimus, four cases being from the Occident and only two cases from Asia (including our Chinese case). Infections in immunocompetent patients were more common in men (4 men, 2 women); patients age ranged 13–72 years old (average 46). All cases have known routes of infection except one developed canaliculitis with no apparent cause.
 |
Table 3 Reports of Infection Due to Members of the Genus Myroides in Immunocompetent Hosts as of September, 2019 |
There are some other risk factors responsible for the Myroides infections. LaVergne et al reported a 74-year-old male developed bacteremia and severe cellulitis caused by Myroides injenensis because of his occupational exposure as a plumber and contact with sewage as well as his alcoholic cirrhosis.30 Another case described a Myroides odoratimimus bloodstream infection in a patient with a chronic diabetic foot ulcer who was exposed to a presumably contaminated water source.3 A 69-year-old man who showed no evidence of immunocompromise frequently swam in a freshwater river suffered a right lower extremity cellulitis, fever, chills and sepsis because of Myroides odoratus, the portal of entry was probably the small abrasion that became contaminated with water during swimming.33 Some other reports have been described infections in the same way.35 Open wounds with exposure to water can be considered as a risk factor to cause rapidly invasive Myroides infections, regardless of the immunity of patients. Maraki et al reported a healthy child developed cellulitis after a pig bite,9 while Willems et al describe a case of fulminant erysipelas with sepsis following a scratch of the domestic dog in a corticosteroid-treated host,36 the two cases above indicated that animal attacks on people may be another risk factor to cause the infections of Myroidesspp. Licker et al described an outbreak of four UTIs caused by Myroides odoratimimus, all patients were immunocompromised and three of them underwent urinary catheterization with a Foley’s catheter upon admission.16 Lorenzin et al also reported a Myroides odoratimimus UTI in an immunocompromised patient who had a permanent urinary Foley’s catheter due to urinary retention.8 There are also some CRBSI cases described.6 Carrying catheters in immunocompromised patients may be important for Myroidesspp. to cause infections. In our case, the patient who had no history of disease was infected with CRBSI due to a left femoral vein catheterization, this should be observed.
Moreover, some works of literature substantiated Myroidesspp. have the capacity of co-aggregation and self-aggregation to form biofilm using crystal violet binding assay19 and the bacterial surface is extremely hydrophobic because of a polysaccharide capsule possessed.8 Biofilms can adhere to both biotic and abiotic surfaces like medical devices and the bacteria can be entrapped within a self-produced extracellular polymeric matrix, which increases pathogenicity in device-related infections and is associated with conventional therapeutic failure, as well as recurrent infections.8,19 Some virulence factors (VFs) of the genus Myroides were identified in several works of literature. Hu et al found some similar virulence factors in the genomes of three clinically pathogenic and three environmental Myroides. odoratimimus strains with the help of VFDB protein Set B database, the VFs included capsule/capsular polysaccharide, intracellular survival and invasion factors, molecular chaperone, urease, acinetobactin, Streptococcal enolase, heme biosynthesis, acyl carrier protein, and T4SS effectors.37
The treatment of Myroidesspp. infections is difficult because the genus is often multi-drug-resistant.30 Many strains have been recognized as resistant to beta-lactams, monobactams and carbapenems due to the production of chromosome-encoded metallo-β-lactamase (MUS-1 and TUS-1),36 Myroides odoratimimus is intrinsically resistant to colistin.36 In addition, a new subclass B1 metallo-β-lactamase gene blaMOC was found which also conferred resistance to most beta-lactams except for aztreonam and cefepime.38 There was another report described MUS-2, a novel variant of the chromosome-encoded β-lactamase MUS-1, reducing the susceptibility to beta-lactams.39 Some strains have shown a susceptibility to β-lactamase inhibitor compounds,30,33,35 and the isolate in our report is sensitive to cefoperazone/sulbactam which is a kind of β-lactamase inhibitor. Perhaps β-lactamase inhibitor compounds can become an option for treating such infections. Myroidesspp. has variable susceptibility to aminoglycosides, quinolones, trimethoprim/sulfamethoxazole31 and tetracyclines. Our patient’s isolate is resistant to all drugs except for cefoperazone/sulbactam. She ultimately responded well to treatment with cefoperazone/sulbactam combining levofloxacin. Given no clear guidelines for the treatment of this genus and the variability in susceptibility testing of different Myroides species, antimicrobial treatment should be based on drug sensitivity results.
Conclusion
In conclusion, with the increasing invasive therapy in clinical, clinicians should be alert to the possibility of Myroidesspp. becoming a new highly pathogenic pathogen in immunocompetent hosts. Identification and antimicrobial susceptibility test should be done in time to guide a reasonable clinical medicine application.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Benedetti P, Rassu M, Pavan G, Sefton A, Pellizzer G. Septic shock, pneumonia, and soft tissue infection due to Myroides odoratimimus: report of a case and review of Myroides infections. Infection. 2011;39(2):161–165. doi:10.1007/s15010-010-0077-1
2. Schröttner P, Rudolph WW, Eing BR, Bertram S, Gunzer F. Comparison of VITEK2, MALDI-TOF MS, and 16S rDNA sequencing for identification of Myroides odoratus and Myroides odoratimimus. Diagn Microbiol Infect Dis. 2014;79(2):155–159. doi:10.1016/j.diagmicrobio.2014.02.002
3. Endicott-Yazdani TR, Dhiman N, Benavides R, Spak CW. Myroides odoratimimus bacteremia in a diabetic patient. Baylor Univ Med Center Proc. 2015;28:342–343. doi:10.1080/08998280.2015.11929268
4. Li H-M. Distribution and clinical characteristics of pathogenic bacteria causing catheter-related bloodstream infections. Pak J Pharm Sci. 2015;28:1163–1166.
5. Douce RW, Zurita J, Sanchez O, Aldaz PC. Investigation of an outbreak of central venous catheter–associated bloodstream infection due to contaminated water. Infect Control Hosp Epidemiol. 2008;29(4):364–366. doi:10.1086/533543
6. Spanik S, Trupl J, Krcmery V. Nosocomial catheter-associated Flavobacterium odoratum bacteraemia in cancer patients. J Med Microbiol. 1998;47(2):183. doi:10.1099/00222615-47-2-183
7. Liu H, Iwase H, Wijkstrom M, et al. Myroides infection in a baboon after prolonged pig kidney graft survival. Transplant Direct. 2015;1(4). doi:10.1097/TXD.0000000000000523
8. Lorenzin G, Piccinelli G, Carlassara L, et al. Myroides odoratimimus urinary tract infection in an immunocompromised patient: an emerging multidrug-resistant micro-organism. Antimicrob Resist Infect Control. 2018;7(1):96. doi:10.1186/s13756-018-0391-4
9. Maraki S, Sarchianaki E, Barbagadakis S. Myroides odoratimimus soft tissue infection in an immunocompetent child following a pig bite: case report and literature review. Br J Infect Dis. 2012;16(4):390–392. doi:10.1016/j.bjid.2012.06.004
10. Girdhar A, Singh A, Usman F, Bajwa A. A rare cause of pneumonia and septic shock in an immunocompetent host. Chest. 2013;144(4):200A. doi:10.1378/chest.1684235
11. Deepa R, Venkatesh K, Parveen JD, Banu ST, Jayalakshmi G. Myroides odoratus and Chryseobacterium indologenes: two rare isolates in the immunocompromised. Indian J Med Microbiol. 2014;32(3):327. doi:10.4103/0255-0857.136592
12. Thomas M, Padmini S, Govindan V, Appalaraju B. Oerskovia turbata and Myroides species: rare isolates from a case of acalculus cholecystitis. Indian J Med Microbiol. 2007;25(3):297. doi:10.4103/0255-0857.34782
13. Mahapatra A, Mohapatra PR, Choudhury S, Deep N. Empyema caused by Myroides odoratimimus in a patient with liver abscess. Lung India. 2019;36(5):459. doi:10.4103/lungindia.lungindia_42_19
14. Prateek S, Gupta P, Mittal G, Singh AK. Fatal case of pericardial effusion due to Myroides odoratus: a rare case report. J Clin Diagn Res. 2015;9(11):DD01. doi:10.7860/JCDR/2015/13028.5790
15. Morrell JM, Núñez-González A, Crespo-Félez I, et al. Removal of bacteria from boar semen using a low-density colloid. Theriogenology. 2019;126:272–278. doi:10.1016/j.theriogenology.2018.12.028
16. Licker M, Sorescu T, Rus M, et al. Extensively drug-resistant Myroides odoratimimus–a case series of urinary tract infections in immunocompromised patients. Infect Drug Resist. 2018;11:743. doi:10.2147/IDR.S161069
17. Ravindran C, Varatharajan GR, Raju R, Vasudevan L, Anantha SR. Infection and pathogenecity of Myroides odoratimimus (NIOCR-12) isolated from the gut of grey mullet (Mugil cephalus (Linnaeus, 1758)). Microb Pathog. 2015;88:22–28. doi:10.1016/j.micpath.2015.08.001
18. Yang Q, Tian T, Niu T, Wang P. Molecular characterization of antibiotic resistance in cultivable multidrug-resistant bacteria from livestock manure. Environ Pollut. 2017;229:188–198. doi:10.1016/j.envpol.2017.05.073
19. Pompilio A, Galardi G, Gherardi G, et al. Infection of recurrent calcaneal ulcer caused by a biofilm-producer Myroides odoratimimus strain. Folia Microbiol (Praha). 2018;63(2):203–207. doi:10.1007/s12223-017-0552-5
20. Lahmer T, Beitz A, Ehmer U, Schmid R, Huber W. Septic shock due to Myroides odoratus in a medical intensive care unit patient with severe necrotising pancreatitis. Anaesth Intensive Care. 2016;44(2):1–2. doi:10.1177/0310057X1604400201
21. Cho S-H, Chae S-H, Im W-T, Kim SB. Myroides marinus sp. nov., a member of the family Flavobacteriaceae, isolated from seawater. Int J Syst Evol Microbiol. 2011;61(4):938–941. doi:10.1099/ijs.0.024067-0
22. Yan S, Zhao N, Zhang X-H. Myroidesphaeus sp. nov., isolated from human saliva, and emended descriptions of the genus Myroides and the species Myroides profundi Zhang et al. 2009 and Myroides marinus Cho et al. 2011. Int J Syst Evol Microbiol. 2012;62(4):770–775. doi:10.1099/ijs.0.029215-0
23. Zhang Z-D, He L-Y, Huang Z, Sheng X-F. Myroides xuanwuensis sp. nov., a mineral-weathering bacterium isolated from forest soil. Int J Syst Evol Microbiol. 2014;64(2):621–624. doi:10.1099/ijs.0.056739-0
24. Tomova A, Tomova I, Vasileva-Tonkova E, et al. Myroides guanonis sp. nov., isolated from prehistoric paintings. Int J Syst Evol Microbiol. 2013;63(11):4266–4270. doi:10.1099/ijs.0.050831-0
25. Ram H, Kumar A, Thomas L, Dastager SG, Mawlankar R, Singh VP. Myroides indicus sp. nov., isolated from garden soil. Int J Syst Evol Microbiol. 2015;65(11):4008–4012. doi:10.1099/ijsem.0.000530
26. Yoon J, Maneerat S, Kawai F, Yokota A. Myroides pelagicus sp. nov., isolated from seawater in Thailand. Int J Syst Evol Microbiol. 2006;56(8):1917–1920. doi:10.1099/ijs.0.64336-0
27. Kim D-S, Paek J, Shin JH, et al. Genome sequence of Myroides injenensis M09-0166T, isolated from clinical specimens. Am Soc Microbiol. 2012;194:2748–2749.
28. Liu T, Zhu L, Zhang Z, Jiang L, Huang H. Draft genome sequence of Myroides sp. N17-2, a multidrug-resistant bacterium isolated from radiation-polluted soils. Genome Announc. 2017;5(46):e01301–e01317. doi:10.1128/genomeA.01301-17
29. Zhang X-Y, Zhang Y-J, Chen X-L, et al. Myroides profundi sp. nov., isolated from deep-sea sediment of the southern Okinawa Trough. FEMS Microbiol Lett. 2008;287(1):108–112. doi:10.1111/fml.2008.287.issue-1
30. LaVergne S, Gaufin T, Richman D. Myroides injenensis bacteremia and severe cellulitis. Open Forum Infect Dis. 2019;6(7). doi:10.1093/ofid/ofz282
31. Beharrysingh R. Myroides bacteremia: a case report and concise review. IDCases. 2017;8:34–36. doi:10.1016/j.idcr.2017.02.012
32. Johnson RJ, Nolan C, Wang SP, Shelton WR, Blaser MJ. Persistent Campylobacter jejuni infection in an immunocompromised patient. Ann Intern Med. 1984;100(6):832–834. doi:10.7326/0003-4819-100-6-832
33. Green BT, Green K, Nolan PE. Myroides odoratus cellulitis and bacteremia: case report and review. Scand J Infect Dis. 2001;33(12):932–934. doi:10.1080/00365540110077065
34. Ali MJ, Joseph J, Sharma S, Naik MN. Canaliculitis with isolation of Myroides species. Ophthal Plast Reconstr Surg. 2017;33(3):S24–S25. doi:10.1097/IOP.0000000000000604
35. Jover-Sáenz A, Pérez-Villar F, Barcenilla-Gaite F. Severe sepsis caused by infected prosthesis joint due to Myroides odoratimimus. Med Clin (Barc). 2016;147(6):276. doi:10.1016/j.medcli.2016.04.011
36. Willems P, Muller J, Verhaegen J, Saegeman V, Desmet S. How to treat a fulminant erysipelas and sepsis caused by Myroides odoratimimus: case report and literature review. Acta Clin Belg. 2017;72(5):331–335. doi:10.1080/17843286.2016.1245173
37. Hu S, Cao L, Wu Y, et al. Comparative genomic analysis of Myroides odoratimimus isolates. MicrobiologyOpen. 2019;8(2):e00634. doi:10.1002/mbo3.2019.8.issue-2
38. Xu S, Chen Y, Fu Z, et al. New subclass B1 Metallo-β-lactamase gene from a clinical pathogenic Myroides odoratus strain. Microb Drug Resist. 2018;24(7):909–914. doi:10.1089/mdr.2017.0233
39. Al-Bayssari C, Gupta SK, Dabboussi F, Hamze M, Rolain J-M. MUS-2, a novel variant of the chromosome-encoded β-lactamase MUS-1, from Myroides odoratimimus. New Microbes New Infect. 2015;7:67–71. doi:10.1016/j.nmni.2015.06.007
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
