Back to Journals » Journal of Asthma and Allergy » Volume 15
A Comparison of the Effectiveness of Asthma Medications on Asthma Exacerbations in Real World National Cohort
Authors Park HJ , Jeon S , Lee HS , Kim BY, Chae YJ, Kim GO, Park JW, Lee JH
Received 21 June 2022
Accepted for publication 8 August 2022
Published 24 August 2022 Volume 2022:15 Pages 1155—1165
DOI https://doi.org/10.2147/JAA.S379394
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Amrita Dosanjh
Hye Jung Park,1 Soyoung Jeon,2 Hye Sun Lee,2 Bo Yeon Kim,3 Yu Jin Chae,3 Gui Ok Kim,3 Jung-Won Park,4,5 Jae-Hyun Lee4,5
1Department of Internal Medicine, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Republic of Korea; 2Biostatistics Collaboration Unit, Yonsei University College of Medicine, Seoul, Republic of Korea; 3Healthcare Insurance Review & Assessment Service, Wonju, Republic of Korea; 4Division of Allergy and Immunology, Department of Internal Medicine, Yonsei University College of Medicine, Seoul, Republic of Korea; 5Institute of Allergy, Yonsei University College of Medicine, Seoul, Republic of Korea
Correspondence: Jae-Hyun Lee, Division of Allergy and Immunology, Department of Internal Medicine, Institute of Allergy, Yonsei University College of Medicine, 50-1 Yonsei-ro, Seodaemun-gu, Seoul, 03722, Republic of Korea, Tel +82-2-2228-1977, Fax +82-2-393-6884, Email [email protected]
Background: Although a wide variety of asthma medications have been developed and are used in clinical practice, there is limited evidence of their comparative effects on asthma exacerbations.
Methods: We used claims data provided by the Health Insurance Review and Assessment Service. We selected subjects commencing asthma treatment between July 1, 2017 and June 30, 2018, with no change in drug regimen. The primary outcome was asthma exacerbation requiring systemic corticosteroids. Cox regression analysis was used to assess outcomes considering the exacerbation-free period.
Results: Of the 254,951 asthma subjects, 107,694 subjects (42.2%) experienced asthma exacerbation. Inhaled corticosteroids (ICSs) (hazard ratio [HR], 0.378– 0.508), ICS-long-acting β2-agonist (LABAs) (HR, 0.284– 0.479), long-acting muscarine antagonists (LAMAs) (HR, 0.432– 0.572), leukotriene receptor antagonists (LTRAs) (HR, 0.371– 0.419), and xanthines (HR, 0.326– 0.482) significantly reduced the rate of first and second exacerbation of asthma (all P-values, < 0.001). The clinical effectiveness of asthma medications varied according to the active ingredient (HR 0.164– 0.670) and was significant for all active ingredients (all P-values, < 0.001). The effectiveness of combination treatment using ICS-LABA and LTRA varied (HR, 0.159– 0.670); however, all combination treatment options evaluated were effective in preventing asthma exacerbations (all P-values, < 0.001). Long-term use of ICS-LABA (HR, 0.278– 0.653), LTRA (HR, 0.259– 0.628), and xanthines (HR, 0.351– 0.783) showed consistent effectiveness (all P-values, < 0.001).
Conclusion: This real-world study showed that the effectiveness of asthma medications varied according to drug type, active ingredient, combination, and period of use, although effectiveness was significant in all cases studied.
Keywords: asthma, medication, exacerbation, real-world data, drug, combination
Introduction
Asthma is a common chronic airway inflammatory disease that requires continuous management with anti-inflammatory drugs. The Global INitiative for Asthma (GINA) guidelines suggest that asthma medications should be prescribed in asthma, although they do not specify specific active ingredients.1 Many patients with asthma use different asthma medications; however, there are insufficient data on the optimal combination of active ingredients. While there is currently increased availability of different categories of medication and regimens for the treatment of asthma, comparison studies between active ingredients or drug combination type are currently lacking and findings are inconsistent.2,3 Many clinicians are aware of the need to prescribe anti-inflammatory asthma medication in patients with asthma and the main difficulty concerns the choice of the optimal active ingredient for the individual patient. To assist clinicians in prescribing the appropriate regimen, large studies in the real-world setting without sponsorship are required to compare the clinical effects of asthma medications according to the active ingredient and drug combinations.
As asthma is a chronic disease, many patients continue their medication for a long time. Continuous use of inhaled corticosteroids (ICSs), as the mainstream of anti-inflammatory treatment, is strongly associated with a decreased risk of asthma mortality.4 Recent guidelines highlight the importance of regularly using ICSs and recommend that ICSs are not stopped completely in all asthma patients.5 Although adherence to ICSs remains low (approximately 22–63%),6,7 many clinicians have tried to educate patients with asthma to continue with regular ICS treatment. However, there are insufficient data concerning the effects of continued use of non-ICS asthma medications. Therefore, we need to compare clinical effects of asthma medication, particularly non-ICS agents, according to the duration of medication use.
All medical institutions in South Korea claim medical expenses through the Korean Health Insurance Review and Assessment Service (HIRA), and this committee approves insurance reimbursement. Therefore, the HIRA collects the claims data including medical visits and medical records for almost the entire national population.8 These claims data provided by the HIRA represent real-world data without any intervention. We aimed to compare the effects of asthma medications according to the drug type, active ingredient, type of drug combination, and duration of medication use based on real-world big data, the HIRA claim data, in Korea.
Materials and Methods
Data
The national health insurance system covers all Korean citizens. The claims data for this national system provided by the HIRA contain all medical visits and the drug regimens prescribed by the medical institutions. We analyzed the HIRA claim data generated between July 1, 2016 and June 30, 2019.
Subjects
The definition of asthma has been previously described.9 Briefly, (1) age ≥15 years; (2) ICD-10 codes for asthma (J45 and J46) as primary diagnosis or first sub-diagnosis; and (3) prescription of asthma medications on at least 2 occasions during outpatient visits10 or prescription of asthma medication following an outpatient visit and admission with systemic corticosteroids during the study period.
We selected patients with asthma commencing medication for the first time between July 1, 2017 and June 30, 2018 (study period). Of these, we excluded subjects who used asthma medication between July 1, 2016 and June 30, 2017 (wash-out period) and selected subjects diagnosed with asthma for the first time during the study period, to minimize the gap of asthma severity. In addition, we excluded subjects who changed their regimen between July 1, 2017 and June 30, 2019 (assessment period) to minimize the confounding effects of multiple use. During the assessment period, clinical outcomes of asthma according to asthma medication, asthma exacerbation requiring systemic corticosteroids were evaluated (Figure 1).
 |
Figure 1 Study design and period. |
Study Design
This study was designed to evaluate the clinical effects of asthma medications according to drug type, active ingredient, drug combination type, and duration of medication use. First, we compared the effects of asthma medications according to the type: inhaled corticosteroid (ICS), ICS-long acting β2-agonist (LABA), long acting muscarine antagonist (LAMA), leukotriene receptor antagonist (LTRA), and xanthines. Second, we classified asthma medication users according to the active ingredients and their dosage. Third, we analyzed the effects of different combinations of ICS-LABA and LTRA. Finally, we classified asthma medication users according to the period of use: <3 months, 3–6 months, 6–9 months, and ≥9 months. In all the subgroup analyses, we excluded subgroups with <100 subjects.
Period of Asthma Medication Use
We calculated the duration of asthma medication use by adding up the number of days on prescription for asthma during the study period.
Charlson’s Comorbidity Index
The Charlson’s comorbidity index (CCI) which predicts disease prognosis was calculated to adjust for underlying diseases which can affect poor clinical outcomes. Well-known underlying conditions, which affect mortality and poor prognosis were assessed using the diagnostic code of claims data between July 1, 2017 and June 30, 2018.
Clinical Outcomes
We defined acute exacerbation of asthma, as the primary clinical outcome, as follows: admission to the medical center (out-patient or in-patient) with asthma symptoms (according to the ICD-10 code of asthma [J45 and J46]) resulting in the use of systemic corticosteroids. We assessed the first and second occurrence of acute exacerbations, and the exacerbation-free period to be used in Cox regression analysis.
Ethics
This study was approved by the Institutional Review Board of Severance Hospital (number: 4-2020-1355). The informed consent requirement was waived due to the minimal risk and retrospective nature of the study design which uses databases.
Statistical Analysis
We generated a time variable from the first date of asthma medication prescribed to the date of the event (first or second acute exacerbation of asthma) and defined this as the exacerbation-free period. Considering this time variable, we used Cox regression analysis to reveal comparative effects of asthma medications. The control group was defined as non-users of asthma medication in all the analysis. In addition, age, sex, and CCI were adjusted for in all the Cox regression analyses. The data were analyzed using SAS Enterprise version 6.1 (SAS Institute Inc., Cary, NC, USA). A P value <0.05 was considered to indicate statistical significance.
Results
Study Subjects
During the study period, 731,933 patients with asthma were assessed. Of these, 640,453 used study drugs (ICS, ICS-LABA, LAMA, LTRA, and/or methyl xanthines). After exclusion of patients who had already used a study drug during the wash-out period, there were 312,242 treatment-naïve patients diagnosed with asthma for the first time during the study period. We further excluded 57,291 patients who changed their regimen during the assessment period. Finally, we analyzed the data of 254,951 patients with asthma to define the effects of asthma medication, to minimize confounding factors (Figure 2).
 |
Figure 2 Study flow. Abbreviations: ICS, Inhaled corticosteroid; LABA, long-acting β2-agonist; LAMA, long-acting muscarine antagonist; LTRA, leukotriene antagonist. |
Baseline Characteristics and Outcomes of Study Subjects
Of the 254,951 patients with asthma, 155,624 (61.0%) were female. The mean age was 55.6±18.3 years. In total, 107,694 subjects (42.2%) had an asthma flare-up during the assessment period. Severe exacerbation requiring in-patient admission occurred in 6379 (2.5%) subjects. Overall, 1901 (0.8%) subjects required admission to the emergency room. Total mortality rate regardless of asthma was 1.21% (Table 1).
 |
Table 1 Baseline Characteristics and Outcomes of Study Subjects |
Clinical Outcomes According to the Type of Asthma Medication
We compared the effects of asthma medication on acute exacerbations according to the type of drug using Cox regression analysis. Subjects using ICSs showed significantly reduced first (hazard ratio [HR], 0.508; 95% confidence interval [CI], 0.495–0.520; P-value, <0.001) and second (HR, 0.378; 95% CI, 0.365–0.391; P-value, <0.001) exacerbation rate compared to that of subjects who did not use the study drugs. ICS-LABA also reduced the rate of first flare-up (HR, 0.479; 95% CI, 0.469–0.488; P-value, <0.001) and second flare-up (HR, 0.284; 95% CI, 0.279–0.290; P-value, <0.001). LAMA, LTRA, and xanthines also significantly reduced acute exacerbation rates (all P-value, <0.001). ICS-LABA was the most effective medication to reduce exacerbations of asthma, and LAMA was the least effective (HR, 0.572–0.432; P-value <0.001) (Figure 3).
Clinical Outcomes According to the Active Ingredient of Asthma Medication
Among ICSs, budesonide (HR for first exacerbation, 0.525; HR for second exacerbation, 0.393), ciclesonide (HR for first exacerbation, 0.378–0.389; HR for second exacerbation, 0.249–0.295), and fluticasone propionate (HR for first exacerbation, 0.233–0.265; HR for second exacerbation, 0.164–0.223) significantly reduced acute exacerbations of asthma (all P-value, <0.001). Among ICSs, fluticasone was the most effective active ingredient preventing asthma exacerbation.
Among the ICS-LABAs, fluticasone furoate-vilanterol was the most frequently prescribed medication, followed by budesonide-formoterol, and fluticasone-salmeterol. These variable composite ICS-LABAs showed variable effects (HR for first exacerbation, 0.326–0.670; HR for second exacerbation, 0.210–0.495), and these were significant (all P-values, <0.001).
Among LAMAs, tiotropium (HR, 0.334–0.446) showed superior effects than ipratropium (HR, 0.450–0.595) (all P-values, <0.001). LTRAs and xanthines had variable but significant effect on reduction of asthma exacerbation (all P-values, <0.001). The difference in effect between the active ingredients in these two medications was small (Table 2).
 |
Table 2 Clinical Outcomes According to the Active Ingredient of Asthma Medication |
Clinical Outcomes According to the Combination of ICS-LABA and LTRA
Regarding the combination of ICS-LABA and LTRA, the combination of fluticasone furoate and montelukast were most frequently prescribed, followed by budesonide-formoterol and montelukast. The effects of the combination of ICS-LABA and LTRA were variable (HR for first exacerbation, 0.305–0.670; HR for second exacerbation, 0.159–0.404), respectively; nevertheless, all combination treatment was effective. Among combinations of ICS-LABA and LTRA, the combination of fluticasone furoate-vilanterol and pranlukast was the most effective in preventing acute exacerbation of asthma (Table 3).
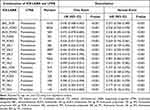 |
Table 3 Clinical Outcomes According to Combination of ICS-LABA and LTRA |
Clinical Outcomes According to the Period of Use of Asthma Medication
All the inhaler type drugs, including ICS, ICS-LABA, and LAMA, showed a decreasing pattern of use, with an increasing period of use. Long-term use of ICS-LABA (HR, 0.278–0.653; all P-value, <0.001), LTRA (HR, 0.259–0.628; all P-value, <0.0001), and xanthine (HR, 0.351–0.783; all P-value, <0.001) showed consistent effects on reducing acute exacerbation of asthma, except for the following. The use of ICS for <6 months in the study period significantly reduced first (HR, 0.411–0.680; both P-value, <0.001) and second (HR, 0.267–0.530; both P-value, <0.001) flare-up. However, ICS use for >6 months did not (HR, 0.922–1.416). LAMA use for <6 months significantly reduced acute exacerbation (HR, 0.377–0.693; all P-value, <0.001); however, LAMA use for >6 months did not (Table 4).
 |
Table 4 Clinical Outcomes According to the Period of Use of Asthma Medication |
Discussion
This study conducted in a real-world setting showed that asthma medications reduce asthma exacerbation and that their clinical effects vary according to drug type, active ingredient, drug type combination, and period of medication use. This study will be a useful guide for clinicians making decisions about prescribing asthma medications. This study has also confirmed that the protective effect of asthma medications depends on consistent use and we recommend that patients with asthma use their medications consistently.
First, we showed that all types of asthma medication reduced exacerbation, although their clinical effects varied. First-line asthma medications (ICSs, ICS-LABA, LTRAs, and xanthines) were effective and effectiveness was comparable (HR, 0.419–0.508 for first exacerbation; HR, 0.284–0.378 for second exacerbation). The ICS-LABA, which is the most frequently recommended combination of drugs prescribed to treat asthma according to GINA guidelines,1 was the most effective drug combination for the prevention of asthma exacerbation. However, the effects of LAMA, a second-line asthma medication,11 were modest, relatively (HR, 0.572 and 0.432, respectively). LAMA is not recommended for use in patients with a first-time diagnosis of asthma, and is generally recommended when first-line asthma medications (ICSs, ICS-LABA, LTRAs, or xanthines) fail to control symptoms.12 We included treatment naïve patients with asthma; therefore, LAMA may not be a suitable choice in the subjects included in this study. In addition, patients requiring LAMA in the first year following a diagnosis of asthma may have severe and uncontrolled asthma with poor clinical outcomes.
Second, we confirmed that asthma medications are associated with different clinical outcomes according to the active ingredient. In ICSs, fluticasone, followed by ciclesonide and budesonide were the most effective medications to reduce asthma exacerbation. The greater clinical efficacy, longer elimination half-life, and higher lipophilicity of fluticasone compared to others may contribute to this finding.13–16 Although previous clinical studies have not definitively confirmed the superior effects of fluticasone over other ICSs,17 the findings of this study support previous pharmacological research. With ICS-LABA, the effects were not quite different according to the active ingredient in this study. Formoterol, a rapid-onset LABA, works faster than other LABAs. Recent well-designed clinical studies have demonstrated the superior efficacy of ICS-formoterol, as maintenance and reliever therapy in the management of asthma compared to that of SABA, as a reliever therapy.18,19 However, real-world studies have shown inconsistent results.20 Further, this study did not demonstrate the superiority of ICS-formoterol over others. Interestingly, a lower dose of the active ingredient of ICS-LABA was more effective than a higher dose. Patients requiring higher doses of ICS-LABA may have severe and uncontrolled asthma with poor clinical outcomes. We speculated that this interesting result is lead to because severe asthma subjects selected high dose of ICS-LABA. We do not think high dose of ICS-LABA lead to poor outcomes. Among LAMAs, tiotropium showed better effects than ipratropium. In Korea, tiotropium is administered by portable devices, while ipratropium is frequently administered by a nebulizer which is frequently used when patients cannot use a portable device because of severe dyspnea, poor condition, or an acute attack of asthma. Therefore, ipratropium users may have severe asthma with poor outcomes. There were no significant differences between LTRAs and xanthines, according to the active ingredient.
Third, the effects of combination therapy with ICS-LABA and LTRAs were variable. The ranking of effects in combination therapy was similar to that in ICS-LABA alone. Almost all cases of combination with ICS-LABA and LTRA showed better effects than ICS-LABA alone. However, the additional effects of LTRA, as an add-on therapy combined with high dose of fluticasone propionate-salmeterol or high dose of fluticasone furoate-vilanterol were not conclusively established. The burden of the diseases is so great in patients with severe asthma, therefore LTRA as add-on therapy does not appear to be effective. In addition, the best effects on exacerbation reduction were observed for the combination of fluticasone furoate-vilanterol and pranlukast. Few studies have compared the efficacy of pranlukast and montelukast, and no significant difference between these treatments has been found in allergic asthma.21 Further research comparing the efficacy of pranlukast and that of montelukast as an added therapy to ICS-LABA is required.
Last, steady use of asthma medications maintains a consistent clinical effect, overall. We recommend good medication adherence for patients with asthma, supporting previous recommendations.22 However, the effect seems to be weak during long-term usage. This phenomenon might be explained similar to the previous results of “less effects at higher dose”: more severe asthma patients may use asthma medications for a longer time than less severe cases. Between the duration and effects, linear correlation was not shown. Variable compliance and the disproportion of the subject number in each category might contribute to it. Especially, prolonged use of ICSs and LAMAs beyond 6 months did not reduce asthma exacerbation. In addition, in Korea, ICS only treatment without LABA is not frequently prescribed. Long-term ICS monotherapy is generally indicated in children, pregnant women, or other patients in whom LABAs are contraindicated. The effects of ICS appear to diminish with use because LABAs cannot be added to the treatment regimen despite clinical need. LAMA could not show significant effects in >6 months users. We postulate that the lack of statistical significance is due to the small number of patients (340 and 203 among 6–9-month users and ≥9-month users, respectively).
It is important to note the strengths of this study. First, this is a real-world study without any intervention during asthma treatment in treatment-naïve asthmatics; therefore, our findings may reflect the reality in clinical practice. Second, this study was conducted by the investigator with no sponsorship from pharmaceutical companies. The results of the comparison between different asthma medications are reliable because there was no conflict of interest. Third, we included almost all asthma patients in Korea. We participated in the Joint Project on Quality Assessment Research in 2021; thus, a government-affiliated organization, HIRA, provided all the original data regarding patients with asthma in Korea.23 Studies conducted by some institutions only have data obtained by the relevant institution; however, this study includes data from all institutions in Korea. This means that if patients with asthma moved from one institution to another for treatment, their data were not lost. Fourth, we designed this study to reveal the pure effects of asthma medication. To minimize the confounding effects of multiple use of asthma medications, we excluded all patients with a change in asthma medication use during the study period. To minimize the effects of previous asthma medication and differences between patients regarding the severity of asthma, we excluded patients who had used asthma medication in the previous year. Last, we did not use simple analysis, rather Cox regression analysis to consider the exacerbation-free period.
Some limitations of this study should be noted. First, we could not classify medications according to the device used to deliver the drug. The effects may vary according to the device used,24,25 although this information could not be obtained in this study due to the nature of the data. Second, some sub-groups include small numbers of patients, as we carefully selected subjects. Third, we could not adjust for asthma severity, although we did our best to control it. Severity of asthma is an important contributing factor in the choice of asthma medication. This confounding factor may affect the interpretation of our results. For example, higher doses of asthma medications should be more effective than lower doses, although in this study, the clinical results were poor among patients on higher doses of medication because severe asthma patient used the higher dose of medications. Last, we could not adjust for some factors predicting exacerbations,26 including lung function, eosinophil count, exposure to environmental allergens, and compliance.
Conclusions
This real-world study which includes almost all patients with asthma in Korea revealed that the effectiveness of asthma medications varied according to drug type, active ingredient, type of combination, and period of medication use. However, all asthma medications showed significant clinical effects on the prevention of asthma exacerbation irrespective of the active ingredient and drug type combination. We recommend that patients with asthma use their medication steadily.
Abbreviations
CI, confidence interval; HIRA, Health Insurance Review and Assessment Service; ICS, Inhaled corticosteroid; LABA, long acting β2 agonist; LAMA, long acting muscarine antagonist; LTRA, leukotriene receptor antagonist; OR, odds ratio; PFT, pulmonary function test; SABA, short-acting β2-agonist.
Data Sharing Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
Ethics Approval and Consent
This study complies with the Declaration of Helsinki. This study was approved by the Institutional Review Board of Severance Hospital (number: 4-2020-1355). The informed consent requirement was waived due to the minimal risk and retrospective nature of the study design which uses databases.
Funding
We are really pleased to have participated in the Joint Project on Quality Assessment Research in 2021 and used quality assessment data of Health Insurance Review & Assessment Service (HIRA). This research was supported by a grant (22213MFDS486) from Ministry of Food and Drug Safety in 2022.
Disclosure
The authors declare that they have no conflicts of interest in relation to this work.
References
1. Reddel HK, Bacharier LB, Bateman ED, et al. Global initiative for asthma strategy 2021. Executive summary and rationale for key changes. Arch Bronconeumol. 2022;58(1):35–51. doi:10.1016/j.arbres.2021.10.003
2. El Baou C, Di Santostefano RL, Alfonso-Cristancho R, et al. Effect of inhaled corticosteroid particle size on asthma efficacy and safety outcomes: a systematic literature review and meta-analysis. BMC Pulm Med. 2017;17(1):31. doi:10.1186/s12890-016-0348-4
3. Shepherd J, Rogers G, Anderson R, et al. Systematic review and economic analysis of the comparative effectiveness of different inhaled corticosteroids and their usage with long-acting beta2 agonists for the treatment of chronic asthma in adults and children aged 12 years and over. Health Technol Assess. 2008;12(19):
4. Suissa S, Ernst P, Benayoun S, Baltzan M, Cai B. Low-dose inhaled corticosteroids and the prevention of death from asthma. N Engl J Med. 2000;343(5):332–336. doi:10.1056/NEJM200008033430504
5. Reddel HK, Bacharier LB, Bateman ED, et al. Global initiative for asthma strategy 2021: executive summary and rationale for key changes. Eur Respir J. 2022;59(1):2102730. doi:10.1183/13993003.02730-2021
6. Barnes CB, Ulrik CS. Asthma and adherence to inhaled corticosteroids: current status and future perspectives. Respir Care. 2015;60(3):455–468. doi:10.4187/respcare.03200
7. Normansell R, Kew KM, Stovold E. Interventions to improve adherence to inhaled steroids for asthma. Cochrane Database Syst Rev. 2017;4:CD012226. doi:10.1002/14651858.CD012226.pub2
8. Choi JY, Yoon HK, Lee JH, et al. Current status of asthma care in South Korea: nationwide the health insurance review and assessment service database. J Thorac Dis. 2017;9(9):3208–3214. doi:10.21037/jtd.2017.08.109
9. Park HJ, Kim SR, Kim S, et al. Impact of the asthma quality assessment program on burden of asthma. J Allergy Clin Immunol Pract. 2021;9(1):419–425 e416. doi:10.1016/j.jaip.2020.08.038
10. Choi JY, Yoon HK, Lee JH, et al. Nationwide pulmonary function test rates in South Korean asthma patients. J Thorac Dis. 2018;10(7):4360–4367. doi:10.21037/jtd.2018.06.109
11. Wang K, Tian P, Fan Y, Wang Y, Liu C. Assessment of second-line treatments for patients with uncontrolled moderate asthma. Int J Clin Exp Med. 2015;8(10):19476–19480.
12. Sobieraj DM, Baker WL, Nguyen E, et al. Association of inhaled corticosteroids and long-acting muscarinic antagonists with asthma control in patients with uncontrolled, persistent asthma: a systematic review and meta-analysis. JAMA. 2018;319(14):1473–1484. doi:10.1001/jama.2018.2757
13. Johnson M. Development of fluticasone propionate and comparison with other inhaled corticosteroids. J Allergy Clin Immunol. 1998;101(4 Pt 2):S434–439. doi:10.1016/s0091-6749(98)70155-1
14. Fuller R, Johnson M, Bye A. Fluticasone propionate–an update on preclinical and clinical experience. Respir Med. 1995;89(Suppl A):3–18. doi:10.1016/0954-6111(95)90259-7
15. Thorsson L, Dahlstrom K, Edsbacker S, Kallen A, Paulson J, Wiren JE. Pharmacokinetics and systemic effects of inhaled fluticasone propionate in healthy subjects. Br J Clin Pharmacol. 1997;43(2):155–161. doi:10.1046/j.1365-2125.1997.d01-1425.x
16. Kelly HW. Establishing a therapeutic index for the inhaled corticosteroids: part I. Pharmacokinetic/pharmacodynamic comparison of the inhaled corticosteroids. J Allergy Clin Immunol. 1998;102(4 Pt 2):S36–S51. doi:10.1016/s0091-6749(98)70004-1
17. Adams N, Bestall JM, Jones PW. Fluticasone versus beclomethasone or budesonide for chronic asthma. Cochrane Database Syst Rev. 2002;(1):CD002310. doi:10.1002/14651858.CD002310
18. Beasley R, Holliday M, Reddel HK, et al. Controlled trial of budesonide-formoterol as needed for mild asthma. N Engl J Med. 2019;380(21):2020–2030. doi:10.1056/NEJMoa1901963
19. Hardy J, Baggott C, Fingleton J, et al. Budesonide-formoterol reliever therapy versus maintenance budesonide plus terbutaline reliever therapy in adults with mild to moderate asthma (PRACTICAL): a 52-week, open-label, multicentre, superiority, randomised controlled trial. Lancet. 2019;394(10202):919–928. doi:10.1016/S0140-6736(19)31948-8
20. Rogliani P, Beasley R, Cazzola M, Calzetta L. SMART for the treatment of asthma: a network meta-analysis of real-world evidence. Respir Med. 2021;188:106611. doi:10.1016/j.rmed.2021.106611
21. Okubo K, Baba K. A double-blind non-inferiority clinical study of montelukast, a cysteinyl leukotriene receptor 1 antagonist, compared with pranlukast in patients with seasonal allergic rhinitis. Allergol Int. 2008;57(4):383–390. doi:10.2332/allergolint.O-08-533
22. Janson SL, McGrath KW, Covington JK, Cheng SC, Boushey HA. Individualized asthma self-management improves medication adherence and markers of asthma control. J Allergy Clin Immunol. 2009;123(4):840–846. doi:10.1016/j.jaci.2009.01.053
23. Choi NK, Shantakumar S, Kim MS, et al. Real-world treatment patterns, outcomes, and healthcare resource utilization in newly treated Korean patients with asthma: a retrospective cohort study. Allergy Asthma Immunol Res. 2022;14(2):220–232. doi:10.4168/aair.2022.14.2.220
24. Small M, Anderson P, Vickers A, Kay S, Fermer S. Importance of inhaler-device satisfaction in asthma treatment: real-world observations of physician-observed compliance and clinical/patient-reported outcomes. Adv Ther. 2011;28(3):202–212. doi:10.1007/s12325-010-0108-4
25. Virchow JC, Crompton GK, Dal negro R, et al. Importance of inhaler devices in the management of airway disease. Respir Med. 2008;102(1):10–19. doi:10.1016/j.rmed.2007.07.031
26. Ban GY, Kim SC, Lee HY, Ye YM, Shin YS, Park HS. Risk factors predicting severe asthma exacerbations in adult asthmatics: a real-world clinical evidence. Allergy Asthma Immunol Res. 2021;13(3):420–434. doi:10.4168/aair.2021.13.3.420
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

