Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 13
A comparative study of the five-repetition sit-to-stand test and the 30-second sit-to-stand test to assess exercise tolerance in COPD patients
Authors Zhang Q, Li YX, Li XL , Yin Y , Li RL, Qiao X, Li W, Ma HF, Ma WH, Han YF, Zeng GQ, Wang QY, Kang J, Hou G
Received 8 May 2018
Accepted for publication 25 July 2018
Published 10 September 2018 Volume 2018:13 Pages 2833—2839
DOI https://doi.org/10.2147/COPD.S173509
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Chunxue Bai
Qin Zhang,1 Yan-xia Li,2 Xue-lian Li,3 Yan Yin,1 Rui-lan Li,1 Xin Qiao,1 Wei Li,1 Hai-feng Ma,1 Wen-hui Ma,1 Yu-feng Han,1 Guang-qiao Zeng,4 Qiu-yue Wang,1 Jian Kang,1 Gang Hou1
1Institute of Respiratory Disease, First Hospital of China Medical University, Shenyang, China; 2Department of Respiratory Medicine, First Hospital of Dalian Medical University, Dalian, China; 3Department of Epidemiology, School of Public Health, China Medical University, Shenyang, China; 4State Key Laboratory of Respiratory Disease, National Clinical Research Center of Respiratory Disease, Guangzhou Institute of Respiratory Disease, First Affiliated Hospital of Guangzhou Medical University, Guangzhou, China
Purpose: The sit-to-stand test (STST) has been used to evaluate the exercise tolerance of patients with COPD. However, mutual comparisons to predict poor exercise tolerance have been hindered by the variety of STST modes used in previous studies, which also did not consider patients’ subjective perceptions of different STST modes. Our aim was to compare the five-repetition sit-to-stand test (5STS) with the 30-second sit-to-stand test (30STS) for predicting poor performance in the six-minute walking test and to evaluate patients’ subjective perceptions to determine the optimal mode for clinical practice.
Patients and methods: Patients with stable COPD performed 5STS, 30STS and the 6MWT and then evaluated their feelings about the two STST modes by Borg dyspnea score and a questionnaire. Moreover, we collected data through the pulmonary function test, mMRC dyspnea score, COPD assessment test and quadriceps muscle strength (QMS). A receiver operating characteristic curve analysis of the 5STS and 30STS results was used to predict 6-minute walk distance (6MWD) <350 m.
Results: The final analysis included 128 patients. Similar moderate correlations were observed between 6MWT and 5STS (r=-0.508, P<0.001) and between 6MWT and 30STS (r=0.528, P<0.001), and there were similar correlations between QMS and 5STS (r=-0.401, P<0.001) and between QMS and 30STS (r=0.398, P<0.001). The 5STS and 30STS score cutoffs produced sensitivity, specificity and positive and negative predictive values of 76.0%, 62.8%, 56.7% and 80.3% (5STS) and 62.0%, 75.0%, 62.0% and 75.0% (30STS), respectively, for predicting poor 6MWT performance. The 5STS exhibited obvious superiority in terms of the completion rate and the subjective feelings of the participants.
Conclusion: As a primary screening test for predicting poor 6MWD, the 5STS is similar to the 30STS in terms of sensitivity and specificity, but the 5STS has a better patient experience.
Keywords: sit-to-stand test, six-minute walk test, COPD, exercise endurance
Introduction
Reduced exercise tolerance is one of the significant clinical features of COPD. The six-minute walk test (6MWT) is a common method of assessing the exercise tolerance of COPD patients, whose 6-minute walk distance (6MWD) <350 m demonstrated a significant increase in mortality,1,2 but it has been difficult to popularize in primary medical institutions due to the need for an appropriate site (a 30 m flat course is required, and the layout of the track may influence the performance).3,4 In recent years, the sit-to-stand test (STST) has also been used to indirectly evaluate exercise tolerance5–7 and lower extremity skeletal muscle function. However, the STST currently lacks unified standards, ranging from 5 to 10 repetitions5,8 (measuring the time taken to complete the given number of repetitions of the sit-to-stand action) or 30 seconds to 3 minutes9–11 (measuring the maximum number of sit-to-stand actions completed in a given time). Most studies have assessed the correlation of one of the STST modes with the 6MWD or quadriceps muscle strength (QMS).12,13 At present, no studies have evaluated differences between the different STST modes in predicting poor exercise tolerance (6MWD <350 m) or have taken patients’ subjective perceptions of different modes into account. Therefore, in this prospective study, we compared the correlation between the five-repetition sit-to-stand test (5STS) and the 30-second sit-to-stand test (30STS) with the 6MWT and QMS in COPD patients, and we evaluated patients’ subjective perceptions of the two modes of STST to determine which mode is more suitable for assessing COPD patients in clinical practice.
Patients and methods
Study subjects
A total of 151 consecutive patients with COPD referred to the Department of Respiratory and Critical Care Medicine of the First Hospital of China Medical University and the First Hospital of Dalian Medical University between August 2017 and December 2017 were considered for enrollment in the study. In total, 128 patients with COPD who met the inclusion criterion and did not meet the exclusion criteria were enrolled in the study. The inclusion criterion was a diagnosis of stable-stage COPD according to the Global Initiative for Chronic Obstructive Lung Disease (GOLD), as updated in 2017. The exclusion criteria were as follows: recent exacerbation of COPD within the 4 weeks preceding the test; limitations on walking and performing the sit-to-stand action, including predominant neurological or musculoskeletal limitation (such as hemiplegia and injury or pathology at lower limb); lower limb joint disease or surgery within the 3 months prior to the test; unstable cardiac condition within the 4 months prior to the test5,14 and long-term oral corticosteroid therapy. The study was approved by the research ethics committees of the First Hospital of China Medical University and the First Hospital of Dalian Medical University, and written informed consent was obtained from all patients.
Pulmonary function and assessment of mMRC and COPD Assessment Test (CAT)
Spirometry, whole-body plethysmography and diffusion capacity measurements were performed according to the American Thoracic Society and the European Respiratory Society guidelines using a Jaeger® MasterScreen system (Jaeger®, Viasys Healthcare GmbH, Hoechberg, Germany). Dyspnea was measured using the Chinese version of the mMRC dyspnea score,15,16 and health status was measured using the Chinese version of the CAT.17,18
QMS
According to the manual provided by the manufacturer and a previous description,19 QMS was measured using the knee of the patient in 90° flexion. The plate of a push–pull handheld dynamometer (type: microFET2™; Hoggan, Salt Lake City, UT, USA) was placed with its anterior end 5 cm proximal to the lateral malleolus on the anterior surface of the leg, perpendicular to the long axis of the tibia. The participant was then asked to generate a maximal knee extension force to hold the line in the same position for a duration of 4 seconds by pushing against the dynamometer plate to which the investigator applied increasing force with no encouragement. Two more trials, for which the tested side of the limb alternated, were administered following the same procedure, with a rest interval of 30–60 seconds between attempts.19 The average value of the final two trials on each side was documented as the maximal isometric force generated on each side, and the average forces of the two sides were added to derive the bilateral strength, the QMS.14,19
5STS and 30STS
A chair with a hard seat whose floor-to-seat height was 48 cm was stabilized by placing it against a wall. After a researcher explained the requirements and precautions to the participant, the participant was asked to sit with his or her feet exactly flat on the ground and his or her upper limbs folded across his or her chest and then to stand up all the way and sit down again without using his or her arms.5,9,14,20 The participant was asked to repeat this sit-to-stand action five times as quickly as possible, and the time taken to complete the five repetitions was recorded.5 Then, the participant was asked to repeat as many of the sit-to-stand actions as possible in 30 seconds, and the maximum number completed was recorded.9 The minimum value of three trials of the 5STS and the maximum value of two trials of the 30STS were considered the participant’s score. Once the participant was unable to perform the motion or asked to suspend the test, the test was terminated. Patients performed three 5STSs and two 30STSs with the appropriate number of intervals (>5 minutes).21,22 After every interval, the participant was asked whether he or she was still tired; if the answer was “no”, the tests continued, and if the answer was “yes”, the participant would continue to rest until he or she no longer felt tired. Sensations of breathlessness were scored using the Borg scale before starting the STSTs, after three 5STSs and after two 30STSs. SpO2 and heart rate (HR) were measured continuously using a finger pulse oximeter (type: MD300W1; ChoiceMMedTM, Beijing, China); throughout every STST, ΔSpO2 and ΔHR were calculated. After completing all STSTs, the participants answered the following three questions: 1) are these tests strenuous for you? (if “yes”, turn to Question 2 and then turn to Question 3; otherwise, turn directly to Question 3); 2) which one is more strenuous, the 5STS or the 30STS? and 3) would you prefer the 5STS or the 30STS next time?
6MWT
STSTs were conducted prior to the 6MWT. After the participant had rested seated on a chair for a sufficient length of time (>30 minutes), the 6MWT was performed on a 30 m, flat, straight corridor by two experienced investigators using standardized encouragement strategies, and the 6MWD was measured.23 Continuous measurements of SpO2 and HR were performed using a finger pulse oximeter mentioned before from 1 minute before the beginning of the 6MWT to the fourth minute after the 6MWT. Additionally, sensations of breathlessness were scored using the Borg scale.
Statistical analyses
All data were analyzed using SPSS 20.0 (SPSS for Windows, version 20.0; IBM Corporation, Armonk, NY, USA). Continuous variables are expressed as the median values and IQRs, as well as the minimum and maximum values. Spearman’s rank correlation coefficients were computed to compare the correlations between the STSTs and pulmonary function, including FEV1, residual volume (RV)/total lung capacity (TLC), 6MWD and QMS. Chi-square tests were used to test for differences in the prediction of a poor 6MWD and the subjective feelings of patients. The sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) were calculated. A receiver operating characteristic (ROC) curve analysis and the area under the curve (AUC) were used to determine the optimal cutoff value for the time of the 5STS and the maximal number of the 30STS, particularly for predicting 6MWD <350 m. A P-value <0.05 was considered as significant.
Results
Patient characteristics
A total of 128 patients were enrolled in the final analysis. The baseline characteristics of these patients are given in Table 1. Based on the FEV1% predicted (FEV1% pred) after the use of a bronchodilator, the severity of airway limitation was divided into the following categories: mild (n=14), moderate (n=60), severe (n=34) and very severe (n=20).
Correlation of STSTs with other outcome measures (convergent validity of STSTs)
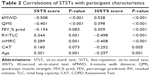
The correlations of the outcomes of the 5STS and the 30STS with the outcomes of the 6MWD (Figure 1), lower extremity muscle strength (Figure 1), pulmonary function and other characteristics of the patients are given in Table 2. In addition, lower extremity muscle strength was measured by assessing QMS. There was a significant strong negative correlation between the 5STS and 30STS scores, as expected (r=−0.783, P<0.001).
Completion rates of different STSTs and subjective feelings of patients
Nine patients (7.0% of total) failed to complete two trials of the 30STS, with two of these patients unable to complete even one trial, while all the patients completed all trials of the 5STS. Among all 128 patients, 88 patients (68.8%) felt that it was strenuous to undergo one or both of the STSTs. Of these 88 patients, most patients (93.2%) felt that the 30STS was more strenuous than 5STS, while six patients (6.8%) thought that the 5STS was more strenuous. When asked which test was preferred if an STST needed to be performed later, 42.2% (54/128) of patients chose the 5STS, 25.0% (32/128) of patients chose the 30STS, and the rest (32.8%, 42/128) thought both were acceptable. Additionally, the 30STS (mean 4.224) resulted in significantly higher Borg dyspnea scores than the 5STS (mean 3.607; P<0.001). ΔHR after 5STS (6±5 beats/min) was significantly lower than ΔHR after 30STS (15±10 beats/min; P<0.001), but there was no significant difference between ΔSpO2 after 5STS (−1%±1%) and ΔSpO2 after 30STS (−1%±1%).
Different STSTs predict a poor 6MWD
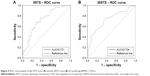
A total of 50 (39.1%) patients had a 6MWD <350 m (median 291 [70] m), with the remaining 78 (60.9%) patients demonstrating 6MWD >350 m (400.5 [73] m). The ROC curve showed that the AUC of the 5STS score predicting poor 6MWD (6MWD <350 m) was 0.731, whereas the AUC of the 30STS score was 0.724 (Figure 2). The cutoff values of the 5STS and 30STS scores were 6.25 and 21.5, respectively. The sensitivity, specificity, PPV and NPV for predicting poor 6MWD analyzed from the cutoff value of the 5STS score were 76.0%, 62.8%, 56.7% and 80.3%, respectively. Our data showed 62.0% sensitivity, 75.0% specificity, 62.0% PPV and 75.0% NPV according to the cutoff value of the 30STS score.
Discussion
In recent years, the STST has been introduced to indirectly assess the exercise tolerance and lower extremity skeletal muscle function of patients with COPD due to its ease of operation and convenience in terms of the space required. However, many different modes of STST exist, and there are no uniform standards; therefore, a comparison of these tests is needed to determine which is the best.
In general, the correlations of the 5STS and the 30STS with exercise tolerance, lower extremity muscle strength and pulmonary function in this study were similar to those in previous studies.5,20,22,24–29 Moderate correlations were observed between the 6MWD and both the 5STS score and the 30STS score (r=−0.508 and r=0.528, respectively), consistent with the results of previous studies.20,24 Additionally, a similar relationship was observed between the 5STS and incremental shuttle walk (r=−0.59).5 Although the STST was used to indirectly evaluate lower extremity muscle strength, a past study5 found only a weak correlation (r=−0.38) between the 5STS and QMS (corresponding data on the correlation between the 30STS and QMS were lacking), similar to our results (r=−0.401 and r=0.398, respectively). In addition, the correlations between the 5STS score and pulmonary function measured by FEV1% pred and RV/TLC (r=−0.190 and r=0.371, respectively) in our data were not as strong as those between the 30STS score and pulmonary function (r=0.344 and r=−0.498, respectively). The weaker correlations between 5STS and FEV1% pred may be explained by the shorter time and the smaller amount of physical effort involved in the 5STS. However, in our study, the results of the two STSTs were higher than those in many European and American studies, which ranged from 11.8 to 19 seconds for the 5STS25–29 and from 10.2 to 13 times for the 30STS.20,22 A similar difference was also observed in body mass index and fat-free mass index. These differences may result from different studies’ inclusion of different ethnicities.
The AUC for the 5STS score was 0.731, which is close to that reported in a previous study (AUC =0.711),29 and the AUC for the 30STS score was 0.724. The performances using their cutoff values demonstrated that the two STSTs are good tools for predicting a poor 6MWD (<350 m). Nevertheless, in addition to having a strong relationship with elements of a patient’s health status, including poor exercise tolerance30,31 and poor pulmonary function,12,32 and reflecting the response to pulmonary rehabilitation,33,34 the role of 6MWT has been demonstrated in predicting long-term mortality35 and quality of life12 and in indicating the need for long-term oxygen therapy36 in COPD patients. The 5STS and 30STS may have potential capacity to predict poor prognosis because 6MWD <350 m is a predictor for high mortality.1,2 It has been reported that the 1-minute STST is strongly associated with long-term morality;37 therefore, the role of 5STS and 30STS in predicting prognosis should be evaluated in further study.
A meta-analysis suggested that the short versions of the STST seem relevant to evaluate leg strength, while the longer versions seem suitable for the evaluation of exercise tolerance. However, previous studies have revealed that both 5STS and 30STS could be used to assess exercise capacity.7,13,38 Further studies with adequate samples need to be performed. Compared with 6MWTs, the STSTs, especially the short versions, are cheap and non-time-consuming and require only basic equipment while being valid, reliable and repeatable.
There were similar correlations of the 5STS and 30STS scores with the 6MWD and QMS, meaning that there was no significant difference in the capacity of the two STST tests to indirectly assess exercise tolerance and lower extremity skeletal muscle strength. Additionally, to the best of our knowledge, few studies of STSTs have taken the subjects’ subjective perceptions into consideration. Our study indicates that the 5STS is clearly superior in terms of the subjective perceptions of the participants, which is consistent with reports that fatigue in healthy volunteers’ quadriceps after the 30STS was more significant than that after the 5STS8 and that the 5STS had a higher completion rate, lower ΔHR and a lower Borg dyspnea score than the 30STS because the 5STS requires less energy and time than the 30STS. Considering the abovementioned points, the 5STS has some advantages as a tool to assess the functional status of COPD patients.
However, there were several limitations in the present study. First, the sample size of this study was relatively small, and the participants were limited to the northern Chinese population. Further investigations should be undertaken in different countries to identify differences in various ethnicities; for example, the 5STS score in Chinese COPD patients is lower than that in European patients.5,14,25,28 Second, this study was cross-sectional, and STST data before and after rehabilitation were not compared; thus, the responses of STSTs to changes in exercise tolerance due to rehabilitation are unknown. Third, data for the 1-minute STST, which have been reported to be a good predictor of increased long-term mortality, were lacking in this study. Our study also could not answer the values of 5STS and 30STS in predicting poor prognosis, which should be evaluated in future studies.
Conclusion
The 5STS and 30STS have similar correlations with poor exercise tolerance and lower extremity skeletal muscle strength. 5STS and 30STS are both reasonable choices for use in clinical and research practices, but 5STS has a better patient experience.
Acknowledgment
This research was supported by the National Key Research and Development Program of China (2016YFC1304103, 2016YFC1304500 and 2016YFC1303900).
Author contributions
GH made substantial contributions to the conception or design of the work. All authors contributed toward acquisition of data for the work. GH, X-lL, QZ, YY and Y-xL performed analysis of data for the work. GH, G-qZ, X-lL and QZ carried out interpretation of data for the work. QZ and GH drafted the work. All authors revised the paper critically for important intellectual content. All authors carried out final approval of the version to be published. All authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Disclosure
The authors report no conflicts of interest in this work.
References
Cote CG, Casanova C, Marín JM, et al. Validation and comparison of reference equations for the 6-min walk distance test. Eur Respir J. 2008;31(3):571–578. | ||
de Torres JP, Casanova C, Cote CG, et al. Six-minute walking distance in women with COPD. COPD. 2011;8(4):300–305. | ||
Sciurba F, Criner GJ, Lee SM, et al. Six-minute walk distance in chronic obstructive pulmonary disease: reproducibility and effect of walking course layout and length. Am J Respir Crit Care Med. 2003;167(11):1522–1527. | ||
Cote CG, Pinto-Plata V, Kasprzyk K, Dordelly LJ, Celli BR. The 6-min walk distance, peak oxygen uptake, and mortality in COPD. Chest. 2007;132(6):1778–1785. | ||
Jones SE, Kon SS, Canavan JL, et al. The five-repetition sit-to-stand test as a functional outcome measure in COPD. Thorax. 2013;68(11):1015–1020. | ||
Bernabeu-Mora R, Medina-Mirapeix F, Llamazares-Herrán E, García-Guillamón G, Giménez-Giménez LM, Sánchez-Nieto JM. The Short Physical Performance Battery is a discriminative tool for identifying patients with COPD at risk of disability. Int J Chron Obstruct Pulmon Dis. 2015;10:2619–2626. | ||
Morita AA, Bisca GW, Machado FVC, Hernandes NA, Pitta F, Probst VS. Best Protocol for the Sit-to-Stand Test in Subjects With COPD. Respir Care. 2018;63(8):1040–1049. | ||
Roldán-Jiménez C, Bennett P, Cuesta-Vargas AI. Muscular Activity and Fatigue in Lower-Limb and Trunk Muscles during Different Sit-To-Stand Tests. PLoS One. 2015;10(10):e0141675. | ||
Jones CJ, Rikli RE, Beam WC. A 30-s chair-stand test as a measure of lower body strength in community-residing older adults. Res Q Exerc Sport. 1999;70(2):113–119. | ||
Crook S, Büsching G, Schultz K, et al. A multicentre validation of the 1-min sit-to-stand test in patients with COPD. Eur Respir J. 2017;49(3):1601871. | ||
Aguilaniu B, Roth H, Gonzalez-Bermejo J, et al. A simple semipaced 3-minute chair rise test for routine exercise tolerance testing in COPD. Int J Chron Obstruct Pulmon Dis. 2014;9:1009–1019. | ||
Ozalevli S, Ozden A, Itil O, Akkoclu A. Comparison of the Sit-to-Stand Test with 6 min walk test in patients with chronic obstructive pulmonary disease. Respir Med. 2007;101(2):286–293. | ||
Vaidya T, Chambellan A, de Bisschop C. Sit-to-stand tests for COPD: A literature review. Respir Med. 2017;128:70–77. | ||
Bernabeu-Mora R, Giménez-Giménez LM, Montilla-Herrador J, García-Guillamón G, García-Vidal JA, Medina-Mirapeix F. Determinants of each domain of the Short Physical Performance Battery in COPD. Int J Chron Obstruct Pulmon Dis. 2017;12:2539–2544. | ||
Bestall JC, Paul EA, Garrod R, Garnham R, Jones PW, Wedzicha JA. Usefulness of the Medical Research Council (MRC) dyspnoea scale as a measure of disability in patients with chronic obstructive pulmonary disease. Thorax. 1999;54(7):581–586. | ||
Cui L, Ji X, Xie M, Dou S, Wang W, Xiao W. Role of inspiratory capacity on dyspnea evaluation in COPD with or without emphysematous lesions: a pilot study. Int J Chron Obstruct Pulmon Dis. 2017;12:2823–2830. | ||
Zhou QT, Mei JJ, He B, et al. Chronic obstructive pulmonary disease assessment test score correlated with dyspnea score in a large sample of Chinese patients. Chin Med J. 2013;126(1):11–15. | ||
Jones PW, Harding G, Berry P, Wiklund I, Chen WH, Kline Leidy N. Development and first validation of the COPD Assessment Test. Eur Respir J. 2009;34(3):648–654. | ||
O’Shea SD, Taylor NF, Paratz JD. Measuring muscle strength for people with chronic obstructive pulmonary disease: retest reliability of hand-held dynamometry. Arch Phys Med Rehabil. 2007;88(1):32–36. | ||
Zanini A, Aiello M, Cherubino F, et al. The one repetition maximum test and the sit-to-stand test in the assessment of a specific pulmonary rehabilitation program on peripheral muscle strength in COPD patients. Int J Chron Obstruct Pulmon Dis. 2015;10:2423–2430. | ||
Smith WN, del Rossi G, Adams JB, et al. Simple equations to predict concentric lower-body muscle power in older adults using the 30-second chair-rise test: a pilot study. Clin Interv Aging. 2010;5:173–180. | ||
Butcher SJ, Pikaluk BJ, Chura RL, Walkner MJ, Farthing JP, Marciniuk DD. Associations between isokinetic muscle strength, high-level functional performance, and physiological parameters in patients with chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2012;7:537–542. | ||
ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories. ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med. 2002;166(1):111–117. | ||
Lv YH, Zhu SF, Zeng XL, et al. Value of five-repetition sit-to-stand test in clinical evaluation of chronic obstructive pulmonary disease. Nan Fang Yi Ke Da Xue Xue Bao. 2016;36(4):477–481. | ||
Spielmanns M, Boeselt T, Gloeckl R, et al. Low-Volume Whole-Body Vibration Training Improves Exercise Capacity in Subjects With Mild to Severe COPD. Respir Care. 2017;62(3):315–323. | ||
Roig M, Eng JJ, Macintyre DL, Road JD, Reid WD. Deficits in muscle strength, mass, quality, and mobility in people with chronic obstructive pulmonary disease. J Cardiopulm Rehabil Prev. 2011;31(2):120–124. | ||
Iwakura M, Okura K, Shibata K, et al. Relationship between balance and physical activity measured by an activity monitor in elderly COPD patients. Int J Chron Obstruct Pulmon Dis. 2016;11:1505–1514. | ||
Janssens L, Brumagne S, Mcconnell AK, et al. Impaired postural control reduces sit-to-stand-to-sit performance in individuals with chronic obstructive pulmonary disease. PLoS One. 2014;9(2):e88247. | ||
Bernabeu-Mora R, Medina-Mirapeix F, Llamazares-Herrán E, Oliveira-Sousa SL, Sánchez-Martinez MP, Escolar-Reina P. The accuracy with which the 5 times sit-to-stand test, versus gait speed, can identify poor exercise tolerance in patients with COPD: A cross-sectional study. Medicine. 2016;95(35):e4740. | ||
Casas A, Vilaro J, Rabinovich R, et al. Encouraged 6-min walking test indicates maximum sustainable exercise in COPD patients. Chest. 2005;128(1):55–61. | ||
Poulain M, Durand F, Palomba B, et al. 6-minute walk testing is more sensitive than maximal incremental cycle testing for detecting oxygen desaturation in patients with COPD. Chest. 2003;123(5):1401–1407. | ||
Spruit MA, Watkins ML, Edwards LD, et al. Determinants of poor 6-min walking distance in patients with COPD: the ECLIPSE cohort. Respir Med. 2010;104(6):849–857. | ||
von Leupoldt A, Taube K, Lehmann K, Fritzsche A, Magnussen H. The impact of anxiety and depression on outcomes of pulmonary rehabilitation in patients with COPD. Chest. 2011;140(3):730–736. | ||
Kerti M, Balogh Z, Kelemen K, Varga JT. The relationship between exercise capacity and different functional markers in pulmonary rehabilitation for COPD. Int J Chron Obstruct Pulmon Dis. 2018;13:717–724. | ||
Casanova C, Cote C, Marin JM, et al. Distance and oxygen desaturation during the 6-min walk test as predictors of long-term mortality in patients with COPD. Chest. 2008;134(4):746–752. | ||
Turner SE, Eastwood PR, Cecins NM, Hillman DR, Jenkins SC. Physiologic responses to incremental and self-paced exercise in COPD: a comparison of three tests. Chest. 2004;126(3):766–773. | ||
Crook S, Frei A, Ter Riet G, Puhan MA. Prediction of long-term clinical outcomes using simple functional exercise performance tests in patients with COPD: a 5-year prospective cohort study. Respir Res. 2017;18(1):112. | ||
Kuo YL. The influence of chair seat height on the performance of community-dwelling older adults’ 30-second chair stand test. Aging Clin Exp Res. 2013;25(3):305–309. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.