Back to Journals » Cancer Management and Research » Volume 13
A Comparative Analysis of Robotic Single-Site Surgery and Laparoendoscopic Single-Site Surgery as Therapeutic Options for Stage IB1 Cervical Squamous Carcinoma
Authors Gao J, Dang J, Chu J, Liu X, Wang J, You J, Jin Z
Received 30 December 2020
Accepted for publication 2 April 2021
Published 21 April 2021 Volume 2021:13 Pages 3485—3492
DOI https://doi.org/10.2147/CMAR.S299827
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Eileen O'Reilly
Jinghai Gao,* Jianhong Dang,* Jing Chu,* Xiaojun Liu, Jing Wang, Jiahao You, Zhijun Jin
Department of Obstetrics and Gynecology, Shanghai ChangZheng Hospital, Naval Medical University, Shanghai, 200003, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Xiaojun Liu
Department of Obstetrics and Gynecology, Shanghai ChangZheng Hospital, Naval Medical University, No. 415 Fengyang Road, Huangpu District, Shanghai, 200003, People’s Republic of China
Tel +8621-81885873
Email [email protected]
Purpose: To compare perioperative outcomes between robotic single-site surgical technique and conventional laparoendoscopic single-site surgical technique.
Methods: This was a retrospective cohort study involving 67 patients who received robotic single-site surgery or laparoendoscopic single-site surgery for the treatment of stage IB1 cervical squamous carcinoma. The robotic single-site radical hysterectomy technique combined with pelvic lymph node dissections were performed in 32 patients while the laparoendoscopic single-site radical hysterectomy technique combined with pelvic lymph node dissections were performed in 35 patients.
Results: The enrolled patients had been diagnosed with stage IB1 cervical squamous carcinoma. The perioperative outcomes were mean age (51.63± 8.32 years in the lymph node dissection (RSS group) and 53.14± 8.14 years in the lymph node dissection (LESS group), p=0.453); BMIs (23.76± 2.72 in the RSS group and 23.46± 2.28 in the LESS group, p=0.629); shorter operative times (223.56± 15.43 min in the RSS group and 248.61± 20.89 min in the LESS group, p< 0.01) and less estimated blood loss (217.25± 16.77 mL in the RSS group and 294.74± 24.00 mL in the LESS group, p< 0.01). None of the study participants exhibited postoperative pain. There were no statistically significant differences in the length of hospital stay (p=0.865), perioperative complications (p=0.602), duration of closure and removal of catheter (p=0.518) as well as in pathological diagnoses between the two groups.
Conclusion: Robotic single-site surgery can be used in the treatment of early stage cervical cancer as it exhibits acceptable operative times and perioperative outcomes. This surgical technique is feasible and safe.
Keywords: cervical squamous cancer, robotic single-site surgery, laparoendoscopic single-site surgery
Introduction
Cervical cancer is the fourth most common cancer globally in female. This disease causes approximately 311,000 mortalities and 570,000 new morbidities each year.1 Radical hysterectomy and pelvic lymph node dissection are the primary therapeutic options in early stage cervical cancer cases.2 Radical hysterectomy techniques such as uterus excision with the parametrium, bilateral pelvic lymph node dissection, and ureter separation involve difficult procedures. The complications associated with this procedure include severe intraoperative bleeding, nerve injuries, postoperative voiding difficulties, infections, lymphatic edema, fistulas, and delayed healing of the suture.3
Abdominal radical hysterectomy has been a therapeutic option for cervical cancer. Advances in gynecologic laparoendoscopic technology have led to laparoendoscopic radical hysterectomy with lymph node dissection being highly accepted in the surgical world.4 Besides, the Da Vinci surgical system has been developed by Intuitive Surgical Inc. (Sunnyvale, CA, USA), and this robotic surgical technique was approved by the Food and Drug Administration (FDA) for gynecologic procedures in 2007. The robotic radical hysterectomy with lymph node dissection technique is widely being used as a therapeutic option for invasive cervical cancer.5 The utilization of minimally invasive surgical techniques is on the rise in gynecologic oncology. Between 2007 and 2010, the proportions of hysterectomies performed by robotic assistance rose from 5% to 9.5%.6 At present, some patients choose laparoscopic or robotic surgery because of the small trauma and beautiful wound.7
As minimally invasive surgical techniques, laparoendoscopic or robotic surgeries are being performed by a multiport approach. However, this procedure has associated risks such as pain, bleeding, hernia, and infections associated with multiple incisions.8
The concept of laparoendoscopic single-site surgery emerged as a less invasive procedure compared to multiport laparoscopy. Robotic surgery has been incorporated into this technique. Compared to the multiport approach, robotic single-site surgery has many advantages; however, its safety and feasibility are still being evaluated.9
In the period when a commercialized single port was not available, surgical techniques were realized using a homemade single port or a single incision with several fascial punctures.10 The fascial puncture procedures led to skin macerations, fascial tears, gas leakage, and wound healing complications. The homemade single port is associated with prolonged operative time, glove tear, gas leakage, and loosening ligature.11
Therefore, to improve the procedural efficiency of RSS and LESS surgery, a durable, flexible, and well-designed single-site platform are essential. For the completion of RSS and LESS surgeries, we utilized a novel commercialized LAGIS single-site port.
We aimed at comparing perioperative outcomes of the RSS surgery and the LESS surgery as therapeutic options for the treatment of stage IB1 cervical squamous carcinoma. Also, we determined the feasibility and safety of RSS surgery in cervical cancer therapy.
Materials and Methods
Study Participants
A total of 67 stage IB1 cervical squamous cancer patients were retrospectively enrolled according to FIGO 2018 (FIGO pathological oncology Committee) cervical cancer staging. These patients had undergone RSS radical hysterectomy with lymph node dissection (RSS group) using the da Vinci Si System, and laparoendoscopic single-site radical hysterectomy with lymph node dissection (LESS group). Both techniques utilized the LAGIS single-site port (LAGIS® Enterprise Co., Ltd, Taiwan) at ChangZheng Hospital affiliated to Navy Medical University in Shanghai, China. This study was done between November 2018 and October 2019. There were no inclusion criteria for the RSS and LESS approach.
To undergo either RSS or LESS surgical approaches, patients were counseled and informed on their advantages, disadvantages, and cost implications. The surgical choice was the patients’ independent choice. Surgical techniques in both groups utilized the same single-site port (LAGIS single-site port) (Figure 1) manufactured in Taiwan.
 |
Figure 1 Surgical techniques in both groups utilized the same single-site port (LAGIS single-site port) manufactured in Taiwan. |
The RSS radical hysterectomy with lymph node dissection was done as follows: Under general anesthesia, a uterine mobilizer and a Foley catheter were attached to the patients and put at a herringbone position. The LAGIS single-site port, and common robotic instruments except the flexible robotic single-site instruments were used in the RSS group. A trans-umbilical skin incision of a transversal length of 3 cm was made (Figure 2). A 3 cm incision was made on the underlying fascia and peritoneum level to enable surgical movements. A wound retractor (LAGIS® Enterprise Co., Ltd, Taiwan) was placed into the fascia opening, and the LAGIS Single-Site port was inserted through the opening that was covered with the wound protector. A pneumoperitoneum was then created by carbon dioxide infusion up to 14 mmHg. The patient was adjusted to a 15-degree Trendelenburg angle position. The 30-degree 12 mm da Vinci stereo laparoscope connected to the robotic system camera was inserted to confirm atraumatic placement of its primary port. The robotic system was positioned between the patients’ legs and docked at the camera port.
 |
Figure 2 A trans-umbilical skin incision of a transversal length of 3 cm was made. |
After docking, one side of the two 8-mm robotic instrument cannulas was inserted into the robotic arms, while the other side of the cannula was inserted into the multichannel of the LAGIS Single-Site port (the port has four channels; two for the robotic instruments and one each for the robotic camera and surgical assistant). The instruments were then placed under careful stereo laparoendoscopic procedures. Robotic monopolar scissors and fenestrated bipolar forceps were mounted through the cannulas (Figure 3).
 |
Figure 3 Robotic monopolar scissors and fenestrated bipolar forceps were mounted through the cannulas. |
Radical hysterectomy with lymph node dissection was performed in all patients, with some variations. After pelvic lymphadenectomy, the ureter was dissected from the lateral peritoneum towards the ureter tunnel. The infundibulo-pelvic ligament was excised in patients who opted for the removal of their ovaries, while the ovarian ligament was cut for those who opted to preserve their ovaries. To expose the rectal-vagina-peritoneum fold, followed by its incision, the uterus was manipulated towards the anterior. The rectum was then separated from the vagina and pushed to the posterior. This exposed the pararectal space. For the bladder to be moved forward towards the anterior vaginal wall, an incision was made on the bladder peritoneum fold. The uterine artery was isolated and cut at its origin. For the ureteral vessel dissection, the tunnel was developed by placing ventral traction on the uterine vessels and freeing the ureter from the adventitial attachments of the medial and ventral vessels. Incisions were then made on the divided anterior vesico-uterine ligament. Incisions were also made on the posterior vesico-uterine ligament. Exposure of the paravesical and pararectal space was done by dissection of the cardinal and sacral ligaments. Incision of the parametrial tissues was followed by the circumferential incision of the upper vaginal part with a 3 cm margin underneath the vaginal fornix. Tissue samples were obtained from the vagina and measured. A running locking suture was used to close the vaginal cuff. For ovarian preservation, the ovaries were transposed to the abdominal sidewall of the pelvis using 3-0 Vicryl suture. Absorbable continuous locking sutures were used to close the umbilicus fascia and subcutaneous layer with 2-0 and 4-0 Vicryl sutures (Figure 4). The estimation of intraoperative blood loss is evaluated by the amount of blood drawn from the attractor since no gauze is used to wipe the blood during the operation.
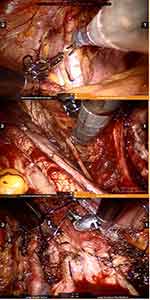 |
Figure 4 Absorbable continuous locking sutures were used to close the umbilicus fascia and subcutaneous layer with 2-0 and 4-0 Vicryl sutures. |
The LESS radical hysterectomy with lymph node dissection procedure was the same as that of the RSS surgery. The only difference was in respect to the instruments used and surgical performance. The LESS surgical procedure was performed through the LAGIS Single-Site port with traditional laparoendoscopic instruments such as dissecting forceps, Johnson & Johnson Ethicon Endo-Surgery GEN11 Generator (5 mm diameter shears and 36 cm length) (Ethicon Endo-Surgery, Inc. Cincinnati, USA), BiClamp (34 cm length) (ERBE Elektromedizin GmbH, Inc. Tubingen, Germany), and needle holders. All these procedures were performed by a gynecologic surgeon who was well versed in robotic and laparoendoscopic procedures.
Data regarding patients’ characteristics and perioperative surgical outcomes were obtained. Perioperative factors such as tumor size as measured by pelvic ultrasonogram or CT/MRI, operative time, estimated blood loss, length of hospital stay, wound complications, Foley catheters, extraction time, and pathological diagnosis after operation were analyzed.
We analyzed the data of 67 cases statistically with a t-test, a chi-squared test, using SPSS Statistics version 26.0. Ethical approval was obtained from the Institutional Review Board of our institute.
Results
Table 1 shows the demographic and clinical characteristics of the study participants. The age, body mass index (BMI), an average diameter of the tumors, and squamous cell carcinoma antigen (SCCA) before the operation revealed that there were no discernable differences between the two groups. In the two approaches, patients had successful surgeries without conversion to other multi-site robotic or laparoendoscopic surgeries. The conversion rate was significantly lower compared to a previously reported rate of 1.5%.12 The mean age of the patients in the two groups was 51.63±8.32 years in the RSS group and 53.14±8.14 years in the LESS group (p=0.453) while the BMI was 23.76±2.72 kg/m2 in the RSS group and 23.46±2.28 kg/m2 in the LESS group (p=0.629). There was no statistical difference in the average diameter of the tumor and SCCA levels between the two groups (p=0.224 and p=0.288, respectively).
 |
Table 1 The Clinical Characteristics of Cases in Both Groups |
Table 2 summarizes the intraoperative, perioperative, and postoperative results. Shorter operative times (223.56±15.43 min in the RSS group and 248.61±20.89 min in the LESS group, p<0.01) and less estimated blood loss (217.25±16.77 mL in the RSS group and 294.74±24.00 mL in the LESS group, p<0.01). From what has been discussed above, the differences in the mean total operation time and the mean estimated blood loss were statistically significant between the two groups p<0.01).
 |
Table 2 Intraoperative, Perioperative and Postoperative Data |
The surgical radicality of the two approaches was comparable. For example, no statistical significance was observed in the average length of excised vaginal tissues in the two groups (p=0.986). Other radicality measures including the average length of the removed cardinal ligament tissue and the number of lymph nodes retrieved exhibited comparable statistical outcomes. In addition, significant differences in the rates of intraoperative blood transfusion or the rate of ovarian preservation between the two groups were not observed. Postoperative pain evaluation for patients who underwent surgery under general anesthesia was done using the PCAs system in our hospital. During PCAs, 0.5L g/kg body weight of fentanyl was injected as rescue analgesia.
Intravenous analgesics were then switched to oral analgesics. The visual analog scale (VAS) system was used to assess pain. The pain was scored by a blinded observer using a verbal numerical rating scale (0 = no pain, 10 = the most severe pain imaginable) at rest, while coughing at 6, 12, 24, and 48 hours post-anesthesia care unit admission Table 3 shows that there was no statistical difference in the mean scores of the two groups at different periods. The average scores of the two groups decreased as time increased. None of the patients complained about postoperative pain.
 |
Table 3 Postoperative Pain Evaluation |
The complication rates in the RSS and LESS groups were 6.25% (2 cases in 32 patients), and 5.71% (2 cases in 35 patients), respectively. The overall complication rate was 5.97%. Differences in the complication rates between the two groups were not statistically significant (p=0.602; Table 2). The combined complication rate of all two procedures was 4 out of 67 cases (5.97%), which was in line with the reported 5.8% in a previous report.13 For the four overall complications, the ureteral injury was reported in two patients (2.99%), one each in the RSS and LESS groups. Treatment of the two cases was done by the implantation of ureteral stents. After 3 months, the ureteral stents were removed by a cystoscope. Bladder injury was documented in one patient (1.49%) of the LESS group. The injured bladder was successfully repaired by using 3-0 Vicryl suture in the operation. In the RSS group, one patient (1.49%) had a case of obturator nerve injury Treatment of this injury was done by using 5-0 Vicryl suture during the operation. There were no incidences of serious vessel injuries, wound infections, or intestinal obstructions.
The differences in the duration of hospital stay after the operation was not statistically different between the two groups (p=0.402; Table 2). Closure duration and postoperative catheter removal durations were not statistically different (p=0.518; Table 2). The refractory urinary retention rate 2 weeks post-operation for RSS, and LESS groups was 21.88% (7 cases in 32 patients), and 17.14% (6 cases in 35 patients), respectively. The overall refractory urinary retention rate was 19.40%. This incidence was higher than that reported in the literature,14 but the catheter was pulled out 3 weeks after operation in their hospital whereas we pulled out the catheter 2 weeks after the operation.
Table 4 shows the pathological diagnoses after an operation. Comparable pathological diagnoses were recorded for the two groups. The statistical differences in the rates of lymphovascular space involvement and bilateral parametrial involvement were not significant between the two groups (p=0.275 and p=0.225, respectively). Equally, the statistical differences in the rates of deep stromal infiltration, vaginal involvement, and metastasis in the pelvic lymph node were not significant (p=0.305; p=0.361 and p=0.289, respectively). The above results showed that there was no significant difference in the range of resection between the two groups, which was in line with the previous report.15
 |
Table 4 Pathological Diagnosis After Operation |
Discussion
Medical and technological advances have led to the development of minimally invasive surgical procedures. The robotic surgical system has lessened the technical challenges associated with laparoendoscopy. This technique has improved surgical dexterity, precision, and visualization.16
Laparoendoscopic single-site surgery presents an opportunity for a potentially scarless, minimally invasive surgery. However, there are technical and surgical difficulties due to space and movement limitations for the instruments.17 The use of RSS in gynecologic surgery was approved in 2013 by the FDA. This procedure has high safety profiles and acceptable surgical outcomes.18,19 RSS retains the advantages of LESS over a multi-site laparoscopic approach. These advantages include decreased postoperative pain with a less predisposition to nerve injuries, improved cosmesis, increased patient satisfaction, shorter hospital stay periods, and a decreased risk of traumatic tissue or vascular injury with trocar placement.20 In contrast to laparoendoscopic single-site surgery, the robotic single-site surgical system solves the problem associated with space and movement by offering better visualization and depth perception.21 The RSS surgical technique, therefore, is easier when compared to the LESS surgical technique.
The Da Vinci surgical system frees surgeons from the conventional bedside operation approach and provides them with overall instrumental and camera control. The physically laborious laparoendoscopic technique is not ergonomically optimal in high-volume operative situations. The robotic 3D-HD vision provides the surgeon with better depth perception and wider vision that enhances surgical performance. In this procedure, the stereo laparoscope can be closely guided to the operative target site under magnification and can perform radical hysterectomy combined with pelvic lymph node dissection by maintaining original planes. These original planes are maintained by curving the da Vinci Single-Site robotic common instruments and LAGIS single-site port. The rotated graspers that can make 360-degree movements in the Da Vinci surgical system make arterial ligation and suturing in easier compared to conventional laparoscopy.
The strengths of this study are as follows. All operations were performed by a single surgeon. This eliminated the possibility of variations in results due to differences in experience, skill set, dexterity, or training. Secondly, the two new surgical approaches (RSS and LESS), were introduced to the hospital at the same time and were performed concurrently during the study period. Therefore, the comparisons are objective and fair.
In addition, the LESS surgical technique has suturing limits while the RSS surgical technique is better for the meticulous suturing of tissues. However, it lacks tactile feedback. Therefore, it has more challenges than the conventional laparoscopy system when performing surgical tasks such as handling tissues like cardinal ligaments that are often stretched with tension. The assistants’ field of vision is different from the surgeons’ while the former sees the surgical field in 2D, the latter, in 3D. This discrepancy can sometimes cause discord between doctors, slowing down the operation.
This study not only measured traditional outcome parameters such as age, BMI, tumor size, operation time, amount of blood loss, and length of hospital stay but also measured parameters of postoperative pain evaluation and operation radicality. When perioperative variables between the two groups were compared, it was established that the mean total operation time and estimated blood loss in the RSS group were less than that in the LESS group. In addition, the less operative time and less estimated blood loss in the RSS group could be associated with the rotating instruments that can make 360-degree movements and robotic 3D-HD vision that gives the operator better depth perception and wider vision. Technical and surgical difficulties in the LESS group are due to space and movement limitations.
Due to technical challenges, when the BMI is over 28 kg/m2, the patients are not deemed suitable for any of these two methods. Patients with a tumor size of more than 4 cm are usually not treated with any of these procedures. Third, measures of radicality were similar in both groups. Fourth, the long hospital stays post-operation compared with other published studies.22 This is attributed to health insurance policies that provide substantially more coverage for in-patient treatment than outpatient treatment.
Study limitations include the small sample size used and the single surgeon involved in all procedures. The fact that our findings are from a single surgeon means that they do not apply to surgeons with less experience.23 Second, this was not a randomized clinical trial, and as such, the comparison between different approaches might be subjective. To compare the operative benefits of the two methods, large sample sizes of cervical cancer cases should be enrolled so that perioperative variables are not affected by the operative experience.
In conclusion, this study suggests that the RSS surgical technique is feasible, safe, and a therapeutic option for cervical cancer. Prospective studies with bigger sample sizes comparing RSS with other methods are recommended to explore its advantages. Surgeons should consider the RSS surgical techniques if they are comfortable with multiport robotic surgeries as this is the most relevant platform from which transition to RSS can be made.
Abbreviations
RSS, robotic single-site; LESS, laparoendoscopic single-site surgical technique; FDA, food and drug administration.
Data Sharing Statement
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Ethics Approval
The protocol of this research has been approved by the Ethics Committee of Shanghai ChangZheng Hospital, and the study complies with the Declaration of Helsinki.
Consent to Participate
All patients have signed written informed consent.
Author Contributions
All authors contributed to data analysis, drafting or revising the article, have agreed on the journal to which the article will be submitted, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no conflicts of interest.
References
1. Bray F, Ferlay J, Soerjomataram I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424. doi:10.3322/caac.21492
2. Saltari M, Corrado G, Patrizi L, Vizza E. Comment: survival rate comparisons amongst cervical cancer patients treated with an open, robot- ic-assisted or laparoendoscopic radical hysterectomy: a five year experience. Surg Oncol. 2016;25:244–245. doi:10.1016/j.suronc.2016.05.005
3. Manchana T, Sirisabya N, Lertkhachonsuk R, et al. Long term complications after radical hysterectomy with pelvic lymphadenectomy. J Med Assoc Thai. 2009;92(4):451–456.
4. Malzoni M, Tinelli R, Cosentino F, Fusco A, Malzoni C. Total laparoendoscopic radical hysterectomy versus abdominal radical hysterectomy with lymphadenectomy in patients with early cervical cancer: our experience. Ann Surg Oncol. 2009;16(5):1316–1323. doi:10.1245/s10434-009-0342-7
5. Nezhat FR, Datta MS, Liu C, Chuang L, Zakashansky K. Robotic radical hysterectomy versus total laparoendoscopic radical hysterectomy with pelvic lymphadenectomy for treatment of early cervical cancer. JSLS. 2008;12(3):227–237.
6. Wright JD, Ananth CV, Lewin SN, et al. Robotically assisted vs laparoscopic hysterectomy among women with benign gynecologic disease. JAMA. 2013;309(7):689–698. doi:10.1001/jama.2013.186
7. Galaal K, Bryant A, Fisher AD, Al-Khaduri M, Kew F, Lopes AD. Laparoscopy versus laparotomy for the management of early stage endometrial cancer. Cochrane Database Syst Rev. 2012;9:CD006655.
8. Shin JH, Howard FM. Abdominal wall nerve injury during laparoendoscopic gynecologic surgery: incidence, risk factors, and treatment utcomes. J Minim Invasive Gynecol. 2012;19(4):448–453. doi:10.1016/j.jmig.2012.03.009
9. Tateo S, Nozza A, Del Pezzo C, Mereu L. Robotic single-site pelvic lymphadenectomy. Gynecol Oncol. 2014;134(3):631. doi:10.1016/j.ygyno.2014.06.027
10. Lin VC, Tsai YC, Chung SD, et al. A comparative study of multiport versus laparoendoscopic single-site adrenalectomy for benign adrenal tumors. Surg Endosc. 2012;26(4):1135–1139. doi:10.1007/s00464-011-2012-7
11. Balaphas A, Hagen ME, Buchs NC, et al. Robotic laparoendoscopy single site surgery: a transdisciplinary re- view. Int J Med Robot. 2013;9(1):1–11. doi:10.1002/rcs.1445
12. Park JY, Nam JH. Laparotomy conversion rate of laparoendoscopic radical hysterectomy for early-stage cervical cancer in a consecutive series without case selection. Ann Surg Oncol. 2014;21(9):3030–3035. doi:10.1245/s10434-014-3707-5
13. Kruijdenberg CB, van den Einden LC, Hendriks JC, et al. Ro-Bot-assisted versus total laparoendoscopic radical hysterectomy in early cervical cancer, a review. Gynecol Oncol. 2011;120:334–339. doi:10.1016/j.ygyno.2010.12.342
14. Ding D, Jiang H, Nie J, et al. Concurrent learning curves of 3-Dimensional and robotic-assisted laparoscopic radical hysterectomy for early-stage cervical cancer using 2-Dimensional laparoscopic radical hysterectomy as a benchmark: a single surgeon’s experience. Med Sci Monit. 2019;25:5903–5919. doi:10.12659/MSM.914952
15. Jeong IG, Khandwala YS, Kim JH, et al. Association of robotic-assisted vs laparoscopic radical nephrectomy with perioperative outcomes and health care costs, 2003 to 2015. JAMA. 2017;318(16):1561–1568. doi:10.1001/jama.2017.14586
16. Gargiulo AR. Computer-assisted reproductive surgery: why it matters to reproductive endocrinology and infertility subspecialists. Fertil Steril. 2014;102(4):911–921. doi:10.1016/j.fertnstert.2014.08.028
17. Eisenberg D, Vidovszky TJ, Lau J, Guiroy B, Rivas H. Comparison of robotic and laparoendoscopic single-site surgery systems in a suturing and knot tying task. Surg Endosc. 2013;27(9):3182–3186. doi:10.1007/s00464-013-2874-y
18. Vizza E, Corrado G, Mancini E, et al. Robotic single-site hysterectomy in low risk endometrial cancer: a pilot study. Ann Surg Oncol. 2013;20:2759–2764. doi:10.1245/s10434-013-2922-9
19. Sendag F, Akdemir A, Oztekin MK. Robotic single-incision transumbilical total hysterectomy using a single-site robotic platform: initial report and technique. J Minim Invasive Gynecol. 2014;21:147–151. doi:10.1016/j.jmig.2013.07.004
20. Jung YW, Kim YT, Lee DW, et al. The feasibility of scarless single-port transumbilical total laparoscopic hysterectomy: initial clinical experience. Surg Endosc. 2010;24:1686–1692. doi:10.1007/s00464-009-0830-7
21. Escobar PF, Knight J, Rao S, Weinberg L. Da Vinci single-site platform: anthropometrical, docking and suturing consideration for hysterectomy in the cadaver model. Int J Med Robot. 2012;8:191–195. doi:10.1002/rcs.448
22. Kim TH, Choi CH, Choi JK, et al. Robotic versus laparoscopic radical hysterectomy in cervical cancer patients: a matched-case comparative study. Int J Gynecol Cancer. 2014;24:1466–1473. doi:10.1097/IGC.0000000000000232
23. Lenihan JP
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
