Back to Journals » Patient Preference and Adherence » Volume 13
A Chinese and Western medication adherence scale in patients with Chronic Kidney Disease
Authors Tan J , Luo L, Zhang M, Chen H, Zhang D , Dong C, Xia B, Fu L, Tang F, Liu X, Tan Q, Wu Y
Received 5 March 2019
Accepted for publication 1 August 2019
Published 30 August 2019 Volume 2019:13 Pages 1487—1495
DOI https://doi.org/10.2147/PPA.S207693
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Naifeng Liu
Jiaowang Tan,1,2 Li Luo,3 Min Zhang,3 Huifen Chen,3 Dingjun Zhang,3 Chendi Dong,3 Bingqing Xia,3 Lizhe Fu,1 Fang Tang,1 Xusheng Liu,1 Qinxiang Tan,2 Yifan Wu1
1Renal Division, the Second Affiliated Hospital of Guangzhou University of Chinese Medicine (Guangdong Provincial Hospital of Chinese Medicine), Guangzhou, People’s Republic of China; 2Renal Division, Beijing University of Chinese Medicine Shenzhen Hospital, Shenzhen, Guangdong, People’s Republic of China; 3The Second Clinical College, Guangzhou University of Chinese Medicine, Guangzhou, People’s Republic of China
Correspondence: Yifan Wu
Renal Division, The Second Affiliated Hospital of Guangzhou University of Chinese Medicine (Guangdong Provincial Hospital of Chinese Medicine), No.111, Dade Road, Yuexiu District
, Guangzhou 510120, People’s Republic of China
Tel +86 13 56 032 4448
Email [email protected]
Objective: The self-reported scale is a widely used method to assess patients’ medication adherence in clinical practice, but there is still a lack of medicine adherence measurement scale for patients with Chronic Kidney Disease (CKD). Therefore, this study aimed to develop a medication adherence measurement scale of traditional Chinese medicine and Western medicine, providing a tool for evaluating medicine adherence of CKD patients.
Methods: In the preliminary stage, we formed the prediction scale after three rounds Delphi method and it was filled by 20 patients, who were selected randomly. After pre-investigation and language adaption, we adjusted the prediction measurement scale which included 31 items based on Knowledge-Attitude-Belief Theory. Then, 222 CKD patients in Guangdong Hospital of traditional Chinese Medicine were investigated by this 31-item scale. We screened 31 items by Items analysis theory, including critical ratio, item correlation analysis, internal consistency analysis, principal component analysis and other methods. The left 26 items made up a formal scale. We collected and analyzed data of the 26-item scale and Chinese version of MGL scale, and took their scores correlation analysis as the criterion validity of the 26-item scale. At the same time, we evaluated content validity, Cronbach alpha coefficient and retest reliability of the 26-item scale.
Results: We developed a scale with 26 items and 5 dimensions finally. In the validation analysis, the scale had good construct validity and content validity. The Pearson relation index between respective scores of the scale and Chinese version of MGL scale was 0.426, P<0.01. The scale also had good reliability as its 0.915 in Cronbach alpha, 0.753 in retest reliability and P<0.01.
Conclusion: The scale revealed great reliability and validity, which could be used as a measurement tool to evaluate the medication adherence of patients with CKD.
Keywords: chronic kidney disease, traditional Chinese medicine, adherence medication, scale, Delphi method
Background
CKD is an important global public health problem. According to related literatures, the prevalence of CKD is about 11%.1 Professor Wang Haiyan’s team2 carried out a large-scale epidemiological investigation of chronic kidney disease (CKD) in China, and the results showed that the prevalence of CKD among Chinese adults reached 10.8%, meaning the estimated number of existing CKD patients in China reached 120 million. CKD is a progressive disease. If it progresses to end-stage renal disease (ESRD), renal replacement therapy, including hemodialysis, peritoneal dialysis and kidney transplantation, is required to maintain life. Therefore, it is essential to find effective and conservative treatment methods to delay the progression of CKD. CKD is also a chronic non-communicable disease, and conservative treatment requires a long-term standardized medication. Previous studies have found that the medication adherence of patients with chronic diseases3 is worse than that of patients with acute diseases. The medication adherence of patients with chronic diseases gradually declines4 after 6 months of treatment generally. Clinical researches have reported that their medicine adherence rate is only about 43–78%.4
CKD patients, especially those in stage 3–5, are often associating with other diseases such as hypertension, diabetes, cardiovascular disease, metabolic bone disease and anemia. Complication will make the regimen more complex, more drugs and higher cost, resulting the reducing medication adherence.5–7 Because of the special condition, patients with CKD are faced with more problems in medication,8,9 such as the dosage forms of diversity (such as oral, subcutaneous injection, intravenous drip, etc.), drug side effects (such as hormone and immune inhibitors, etc.), frequency of variability (such as the hormone and the reduction taking after next day, etc.), which makes adherence less positive. According to the literature, the rate of low drug adherence in CKD patients is about 26–28%.5 In China, prescriptions for CKD patients often include proprietary of Chinese medicine and traditional Chinese medicine decoction.10 Traditional Chinese medicine has varied dosage forms, decoction and taste, leading to lower adherence rate.11,12,13 On the one hand, the little positive adherence rate of medication affects the clinical efficacy of patients; on the other hand, it also affects the accurate judgment on drug effect of clinical research. It is necessary to find effective methods to measure the medication adherence and noncompliance reasons of CKD patients accurately, so as to accurately evaluate the effectiveness of treatment programs and make evaluation of clinical treatment measures and the outcome of scientific research programs more objective. On the other hand, timely measures should be taken to reduce the rate of noncompliance, so as to improve the clinical efficacy of CKD patients.
Currently, there are a variety of methods for measuring patients’ medication adherence, which can be roughly divided into non-self-report and self-report.14 Non-self-reporting methods include electronic monitoring, pill counting, drug level testing, etc. Self-report methods include interview, medication diary and patient self-reported scale. Among them, the patient self-reported scale is the most widely used evaluation method at present.15,16 However, there is no suitable scale which concentrates on the medication characteristics of CKD or traditional Chinese medicine.
“Knowledge-Attitude-Belief Practice (KABP)” is a behavioral theory that changes human health behavior. It divides the change of human behavior into three consecutive processes: knowledge acquisition, belief generation and behavior formation.17 By learning knowledge and skills, people will gradually form positive beliefs and attitudes, which will lead to healthy behaviors. We believe that creating the medication adherence scale based on this theory might provide a more thorough judgment of patients’ medication adherence. Based on the guidance of KABP theory and clinical treatment and medication of CKD, we learned from foreign-validated scales and integrated domestic experts’ nephropathy knowledge and experience. We construct a medication adherence measurement scale which is suitable for CKD patients in China.
Methods
Preparation
Items of the scale
This scale was constructed as three processes based on the KABP Theory. In the preliminary study, we used Delphi method three times from March to July in 2017 and experts’ opinions were gradually unified. We finally formed the prediction scale which included 31 items from August to December in 2017. In order to adjust the prediction scale, we randomly selected 20 CKD patients from the chronic disease management department of nephropathy in Guangdong Hospital of Traditional Chinese Medicine for pre-investigation and language adaptation. The adjustments were according to the questions below: Could patients understand the items? Could they answer the scale by themselves? How did they comprehend the item content? Were the items ambiguous? Did it take too long in time? Patients’ opinions and suggestions on the scale were collected and discussed again by researchers. The ambiguous sentences, reading difficulties, unclear references and suggestive sentences were modified, and finally, the prediction scale was developed. The prediction scale has 31 items in total, as shown in Supplementary materials.
Scoring rules of prediction scale
The options (A, B, C, D, E) in each question were scored according to 5 grades. The respective score of A–E options in 1–16, 22–31 question is 5, 4, 3, 2, 1 but in 17–21 question it is inverse. The total score was the summation of scores of 31 items. Its full mark is 155. The higher the summation, the better the patients’ medication adherence.
Clinical investigation
Case source
CKD patients who kept long-term follow-up in the chronic disease department of Guangdong Hospital of Traditional Chinese Medicine were recruited from January to March in 2018.
CKD diagnostic criteria
Refer to the 2012 clinical practice guidelines for improving prognosis of global kidney disease (K/DIGO).18
Inclusion criteria
Made a definite diagnosis according to CKD diagnostic criteria; aged 18–80; consent and willingness to cooperate with investigators.
Exclusion criteria
Pregnant or lactating women; patients with severe heart, brain, liver or hematopoietic diseases; illiterate or dyslexic; having serious mental illness or being unable to consent due to dyslexia for other reasons; hospitalizations due to acute complications.
Sample size estimation
According to the principle that the proportion of sample size and number of variables shall be more than 5:1, more than 200 patients were planned to be included for investigation.
Survey methods
The scale investigators were trained uniformly. Before the investigation, investigators shall explain the purpose and method of this research to patients, and obtained the informed consent of the patient. The scales shall be filled out by patients themselves. Scales needed to be handed out, inspected and taken back timely. The investigator shall immediately modify and supplement the items with missing or wrong fillings on the spot.
Items analysis
Critical Ratio (CR) method and homogeneity test were used to explore the differences between high and low score in each item, and conducted homogeneity test among items. Items with large differences would be screened or modified.
Correlation analysis was adopted to analyze the relevance between each item and a collection of other items. The higher the correlation between a single item and the total score of the scale, the higher the homogeneity between them. If the Pearson correlation coefficient between the scale items and the total score of the scale was very small, the items shall be deleted.
Cronbach’s alpha was tested to evaluate the internal consistency of the scale. If an item reduced the overall Cronbach’s alpha, it might be deleted. Factor analysis was used to identify the correlation between the items and the attributes. If the correlation between an item and the main factors have little correlation, it would be deleted.
Reliability and validity test
After screening items by analysis methods above, we formed the formal measurement scale and then we tested its reliability and validity.
Validity means obtaining the degree of psychological or behavior which scales aimed to measured.19 Construct validity, content validity and criterion-related validity were used to evaluate the formal scale validity. The most widely used medication adherence scale, the Morisky, Green and Levine (MGL) scale,20 has only 4 items, simple evaluation content, but good reliability and validity. Its Chinses version could be used as the preliminary judgment of adherence.19,21
Reliability referred to the stability and consistency of the scale results. The better the reliability of the scale, the smaller the measurement standard error.22 Cronbach’s alpha and retest reliability of each factor and the total scale were measured to test the reliability.
Data entry and statistical analysis
The returned questionnaires were input by a professional person assigned in pairs. If they found wrong data during the period, they shall check the original scale immediately for correction and modification. Missing data would be statistically treated according to their properties.22,23 SPSS17.0 was used to analyze the data. The main methods of statistical analysis included descriptive analysis, independent sample t–test, exploratory factor analysis, correlation analysis, etc.
Result
General situation
226 questionnaires were issued in total and 222 were returned, with a recovery rate of 98%. The filling time of the scale was 7.3±1.2 mins.
Results of items analysis
We carried out exploratory factor analysis, correlation analysis, items analysis, reliability and validity test on prediction scale of traditional Chinese and western medication adherence in CKD patients. The results are shown in Table 1. And the indicators which were more than five would be deleted, and eventually 5 items were deleted, including Item17 “Less hospitalization after taking drugs”, Item18 “Symptoms improvement after taking drugs”, Item22 “Don’t want to take medicine in fact”, Item 29 “Often same Chinese medicine prescription in the past month”, Item30 “Changed the number of drugs in prescription on one’s own in the past month”; then, we formed the formal scale and named it Measurement Scale, see Supplementary materials.
 |
Table 1 Items analysis result |
The options (A, B, C, D, E) in each question were scored according to 5 grades. The respective score of A–E option in 1–16, 20–26 item is 5, 4, 3, 2, 1 but in 17–19 item it is inverse. The total score was the summation of scores of 26 items. Its full mark is 130. The higher the summation, the better the patients’ medication adherence.
Scale validity analysis results
Construct validity
Exploratory factor analysis was conducted to determine whether the retained 26 items could reflect the scale structure correctly. In Bartlett sphericity test, X2=2967.731, P<0.001, KMO=0.891, showed good quality and suitability for factor analysis. By the principal component analysis, the linear rotation shaft with the maximum variation method is carried out on the variance. We got 7 elements which were more than 1 in initial eigenvalues. The 7 shared elements were more suitable as the theoretical structure of the scale, and the explanation rate of the cumulative variance of 7 elements is 68.85%. See Table 2 and Figure 1. Linear rotation of 7 elements was carried out on the 26 items to obtain the component matrix, as shown in Table 3. As can be seen from the component matrix after the rotation axis, shared element 1 covered items 4, 6, 7, 8, 9, 10, 11 and 12; shared element 2 covered items 13, 14, 15 and 16; shared element 3 covered items 1, 2, 3 and 5; shared element 4 covered items 22, 23, 24 and 25; shared element 5 covered items 17, 18 and 19; shared element 6 covered items 20 and 21; and shared element 7 only covered item 26. The elements obtained by exploratory factor analysis were the same as the structure of the prediction scale, indicating that the measurement scale had stable construct validity. According to the theoretical structure of the initial scale, combined with the exploratory factor analysis results, the shared element 5 revealed positive belief in drug taking, and the shared element 6 revealed negative belief in drug taking. Because the two elements consisted of few items, we combined them into an element: medication beliefs. There was only item 26 in shared element 7, so we added it to shared element 4 and named as medication behavior. Item 4 is semantically similar to the item in share element 3, so it was added to shared element 3 and named as basic knowledge of taking medicine. As a result, the final five elements were, respectively, named: basic knowledge on medication (5 items, items 1–5), knowledge about Chinese medicine decoction (item 7 and items 6–12), knowledge about taking Chinese medicine (4 items, items 13–16), medication beliefs (item 5 and items 17–21) and medication behavior (5 items, items 22–26).
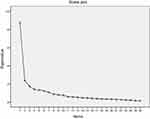 |
Figure 1 Scree plot of the scale. |
 |
Table 2 Cumulative variance interpretation rate in elements analysis |
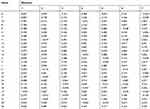 |
Table 3 Elements matrix after rotation axis |
Content validity
The scale was reviewed and investigated by 23 experts in 3 rounds of expert consultation, and modified appropriately according to the experts’ opinions. According to the experts’ opinions, the items reflected the medication adherence of traditional Chinese and western medicine in CKD patients clearly, and the language was clear and easy to understand, without logic confusion, revealing its good content validity.
Calibration correlation validity
222 patients finished the Chinese version of MGL scale while filling the measurement scale. We carried out correlation analysis between the total score of the 26 items and that of the MGL scale, and took it as the calibration validity of the scale. See Table 4. The mean score of the measurement scale was 92.44, and the standard deviation was 14.95. The mean score of the MGL questionnaire was 17.37, and the standard deviation was 2.48. The Pearson correlation coefficient between the scale score and the MGL questionnaire score was 0.426, indicating that there was a correlation between them (see Table 4).
 |
Table 4 The correlation between the scale and Morisky, Green and Levine (MGL) Scale |
Scale reliability analysis results
Internal consistency reliability
The results showed that the total Cronbach’s alpha of 26 items was 0.915, and the Cronbach’s alpha of 5 elements was 0.439–0.930. The internal consistency of the scale was acceptable (See Table 5).
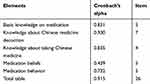 |
Table 5 The internal consistency of the scale (n=222) |
Retest reliability
During filling in the scale, we selected 33 patients from the 222 patients randomly and asked them to refill in the scale within 3 weeks in order to retest reliability statistics. The results showed that the total retest reliability coefficient of the scale was 0.753, and the retest reliability coefficient of each element was 0.472–0.780, indicating that the scale had good stability in retesting, as shown in Table 6.
 |
Table 6 The total and the other factors |
Discussion
Related literatures revealed that adherence had influences on clinical outcomes. An excellent scale of adherence could predict medication adherence accurately, and had correlation with clinical outcomes. For example, the Mediterranean diet score (MDS) on Tehranian adults, which was carried out by Golaleh Asghari’s team, revealed that there was obvious negative correlation between MDS and risk of incident of CKD.24
There were a number of factors which influenced adherence of patients. In summary, it could be divided into three aspects: Knowledge, Belief and Behavior. The measurement scale adopts the Knowledge–Attitude–Belief Practice theory as the theoretical basis to measure the medication knowledge, attitude and behavior of CKD patients, so as to evaluate their medication adherence. For medication knowledge, preliminary construction was mainly referred to the research content before, which was related to the analysis of influencing factors of medication adherence of CKD patients. For medication belief, it was mainly referred to the mature scales, which were based on the health belief model. For medication behavior, modification, which combined features of Chinese and western medicine, was made based on MGL scale. Then, we invited 23 domestic experts in relevant fields to discuss and analyze the preliminary scale, and initially formed a preliminary draft of a 31-item prediction scale. This scale was constructed based on mature theory, previous classic scales, extensive literature research and clinical experience of researchers.
In clinical investigation part, 222 effective scales were collected. We conducted critical ratio method, correlation analysis, Cronbach’s alpha method, factor analysis and other methods; finally, we deleted 5 items and formed a measurement scale with 26 items. 26 items were included in the final scale in total, and it took short time to filling, indicating that the number of items in the scale was appropriate and acceptable.
Then, we carried out validity and reliability analysis. For construct validity, according to the exploratory factor analysis results, the cumulative variance interpretation rate of the 7 elements was 68.855%, and its structure was consistent with the original design, indicating that the three subscales of knowledge, belief and behavior had better construct validity. For calibration correlation validity, the Pearson correlation coefficient of the two was 0.425, p<0.001. Although it indicated an exist correlation, the correlation degree was not good enough. The MGL scale consisted of 4 questions, which covered 3 kinds of behaviors: drug omission, drug inattention and drug withdrawal. But there was lack of medication in traditional Chinese medicine. The measurement scale contained knowledge, belief, behavior and other contents of traditional Chinese medication, which were much more abundant than the MGL scale. Therefore, they were correlated with each other but with low correlation coefficient. The contents included in our scale might be our advantages.
For reliability test, the total Cronbach’s alpha of the final draft of the scale was 0.915, which was better and more reliable than the widely used 2008 MMAS-8 scale with the Cronbach’s alpha of 0.83. However, the Cronbach’s alpha and retest reliability of medication belief were lower. We considered that the condition might relate to the two contrary constructs including positive belief and negative belief in this dimension. Because the two constructs were inverse, the internal consistency coefficient was low. On the other hand, both contents belonged to the same medication belief, the reliability of the scale could be considered acceptable, and it was a more reliable measurement tool for the medication adherence of CKD patients in traditional Chinese and western medicine.
Limitations and prospects of the study
The medication adherence scale of traditional Chinese and western medicine for non-dialysis CKD patients was preliminarily developed. It was inevitable to have deficiencies in the research process because of limited time and knowledge, which were mainly in the following aspects:
First, based on Knowledge–Attitude–Belief Practice theory, the scale was not consistent with scales that were commonly used in health belief theory, and the final form of the scale had a larger proportion of knowledge of medicine but a relatively smaller proportion of behavioral aspects. The results of the survey might not comprehensively reflect the patient’s medication behavior whereas it had a better understanding of the patient’s refusal of medication.
Second, it is a cross-sectional study and without constant follow-up after verifying reliability and validity of the scale. The correlation between good adherence measured by this scale and clinical outcomes is difficult to analyze. We wish to explore more in further study.
Third, chronic disease outpatients of Guangdong Hospital of Traditional Chinese Medicine and urban population took the larger proportion of objects. And the proportion of taking Chinese medicine or proprietary of Chinese medicine was larger, revealing limited population representation. The applicability of the scale needed more researches and more different groups of people for verification.
Conclusion
The measurement scale included 26 items finally, which consisted of 3 dimension (Knowledge, Beliefs, Behavior) and 5 elements. Its 5 elements included basic knowledge on medication (5 items, items 1–5), knowledge about Chinese medicine decoction (item 7 and items 6–12), knowledge about taking Chinese medicine (4 items, items 13–16), medication beliefs (item 5 and items 17–21) and medication behavior (5 items, items 22–26), see Supplementary materials. The content validity, construct validity and calibration correlation validity of the scale achieved benign results. The total Cronbach’s alpha of the scale was 0.915, and the total retest reliability coefficient was 0.753, indicating that the scale had good stability.
Ethics approval
The patients' consent was written informed consent, and this study was conducted in accordance with the Declaration of Helsinki. It was approved by Ethics Committee of Guangdong Provincial Hospital of Chinese Medicine. Petition Number: B2016-93.
Acknowledgments
We greatly thank colleagues from Guangdong Province Hospital of Traditional Chinese Medicine for their contribution to this study. Guangzhou Science and Technology Program key projects: Yi-Fan Wu (2016201604030022); Guangdong Provincial Hospital of Chinese Medicine Program: Yi-Fan Wu (YN2018ZWB04).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Angela C Webster, Evi V Nagler, Rachael L Morton, Philip Masson. Chronic kidney disease. Lancet. 2017;389(10075):1238–1252. doi:10.1016/S0140-6736(16)32064-5
2. Zhang L, Wang F, Wang L, et al. Prevalence of chronic kidney disease in China: a cross-sectional survey. Lancet. 2012;379(9818):815. doi:10.1016/S0140-6736(12)60033-6
3. Mnur SKPRRB, Mphil WYIRRB, Chang AM. Psychosocial correlates of fluid adherence among Chinese haemodialysis patients. J Adv Nurs. 2001;35(5):691–698. doi:10.1046/j.1365-2648.2001.01901.x
4. Chandrashekar K, Meti V, Saritha MK, Hogade AP. Adherence to medication. Int J Res Ayurveda Pharm. 2013;4(2):291–293. doi:10.7897/2277-4343
5. Magacho EJ, Ribeiro LC, Chaoubah A, Bastos MG. Adherence to drug therapy in kidney disease. Braz J Med Biol Res. 2011;44(3):258–262. doi:10.1590/s0100-879x2011007500013
6. SONTAKKE S, BUDANIA R, BAJAIT C, Jaiswal K, Pimpalkhute S. Evaluation of adherence to therapy in patients of chronic kidney disease. Indian J Pharmacol. 2015;47(6):668–671. doi:10.4103/0253-7613.169597
7. ClAXTON AJ, CRAMER J, PIERCE C. A systematic review of the associations between dose regimens and medication adherence . Clin Ther. 2001;23(8):1296–1310.
8. Li J, Wang H, Guirong Y, et al. Relationship between oral medication load and medication adherence after transplantation. Shandong Med J. 2013;53(13):87–88.
9. Judith W, Arjan VZ, Jaap VDB. Self-efficacy and long-term medication use in patients with chronic kidney disease. J Ren Care. 2011;37(3):158–166. doi:10.1111/j.1755-6686.2011.00227.x
10. Paul M, Judd SE, Marie KW, McClellan WM, Safford MM. Low medication adherence and hypertension control among adults with CKD: data from the REGARDS (Reasons for Geographic and Racial Differences in Stroke) study. Am J Kidney Dis. 2010;56(3):447–457. doi:10.1053/j.ajkd.2010.02.348
11. Yifan W, Fuhua L, Lizhe F, et al. Investigation and analysis of treatment adherence in patients with chronic kidney disease. Hebei J Traditional Chin Med. 2012;34(3):471–473.
12. Guan X, Chaqing W. Investigation and analysis of decoction and medication adherence of traditional Chinese medicine. Zhejiang J Traditional Chin Med. 2011;46(5):378–379.
13. Wu Y, Yue L, Pan J, et al. Investigation and analysis of adherence of Chinese medicine patients with hypertension. Guide China Med. 2013;6:2–4.
14. Xu W, Wang Q, Liang W. Application of questionnaire or scale in patient adherence test. Chin J Prev Control Chron Non-communicable Dis. 2007;15(4):403–405.
15. St. Peter WL, Wazny LD, Patel UD. New models of chronic kidney disease care including pharmacists. Curr Opin Nephrol Hypertens. 2013;22(6):656–662. doi:10.1097/MNH.0b013e328365b364
16. Wang W, Lau Y, Loo A, Chow A, Thompson DR. Medication adherence and its associated factors among Chinese community-dwelling older adults with hypertension. Heart Lung. 2014;43(4):278–283. doi:10.1016/j.hrtlng.2014.05.001
17. Bouldin CM, Kimelman D. Development of an antidepressant adherence questionnaire. Acta Psychiatr Scand. 2004;110(3):201. doi:10.1111/j.1600-0447.2004.00350.x
18. Eknoyan G, Lameire N, Eckardt K, et al. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int. 2013. Available from: http://www.kidney-international.org.
19. Dai J, Fu H, Shen Y. Medication compliance of essential hypertension. Chin J Prev Control Chron Dis. 2000;8(03):143–143.
20. Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care. 1986;24(1):67–74.
21. Weihua X, Wang Q, Liang W. Reliability and validity of medication compliance in patients with hypertension in MGL questionnaire. Chin J Prev Control Chron Dis. 2007;15(05):558–560.
22. Kobe JA. Aspects of nutritional knowledge, attitudes and practices of nurses working in the surgical division at the kenyatta national hospital,degree of master. Univ Stellenbosch. 2006;28:1–103.
23. Minglong W. Questionnaire statistical analysis practice: SPSS operation and application[M]. Chongqing: Chongqing University Press; 2010.
24. Farhadnejad H, Mirmiran P, Dizavi A, Yuzbashian E, Azizi F. Adherence to the Mediterranean diet is associated with reduced risk of incident chronic kidney diseases among Tehranian adults. Hypertens Res. 2017;40:96–102. doi:10.1038/hr.2016.98
25. Pei L, Zhang Y, Chou L, et al. Estimation of missing values in scale analysis. Mod Dis Med. 2009;36(1):15–18.
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
