Back to Journals » International Medical Case Reports Journal » Volume 12
A Case Of Ipilimumab-Induced Unusual Serous Retinal Detachment In Bilateral Eyes
Authors Miyakubo T, Mukai R , Nakamura K , Matsumoto H , Akiyama H
Received 29 July 2019
Accepted for publication 9 October 2019
Published 19 November 2019 Volume 2019:12 Pages 355—361
DOI https://doi.org/10.2147/IMCRJ.S225173
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Tomoko Miyakubo, Ryo Mukai, Kosuke Nakamura, Hidetaka Matsumoto, Hideo Akiyama
Department of Ophthalmology, Gunma University Graduate School of Medicine, Maebashi, Gunma, Japan
Correspondence: Ryo Mukai
Department of Ophthalmology, Gunma University Graduate School of Medicine, 3-39-15 Showa-Machi, Maebashi, Gunma 371-8511, Japan
Tel +81 27 220 8338
Fax +81 27 233 3841
Email [email protected]
Purpose: Ipilimumab is an immune checkpoint inhibitor that is now widely used for patients with metastatic malignant melanoma. However, this immune checkpoint inhibitor can induce related adverse events in various organs. Here, we report a case of bilateral drug (ipilimumab)-induced serous retinal detachment (SRD), and the characteristic features found during swept-source optical coherence tomography (SS-OCT).
Case: A 78-year-old man with metastatic melanoma received 4 cycles of dacarbazine, nimustine, vincristine, and interferon-beta starting in January 2014, followed by 47 cycles of nivolumab starting in September 2014. Treatment with ipilimumab was started in June 2017. After 2 cycles of ipilimumab, the patient noticed impairment of the visual field in both of his eyes (at day 22) and visited our department in August 2017. Best corrected visual acuity at this initial visit was 16/20 in both eyes, while a fundus examination revealed SRD and retinal pigment epithelial detachments in both eyes. When using the horizontal and vertical 12 mm B-scanned images of SS-OCT, we detected SRD accompanied by a widely distributed high reflection of the photoreceptor outer segment, including the area where the SRD appeared. In addition, the image also showed the interdigitation zone was indistinguishable. Fluorescein angiography showed little leakage in the maculae. During his course of follow-up examinations, there was an increase in the SRD at the beginning, after which it then gradually decreased. However, the obscurity of the interdigitation zone remained.
Conclusion: Ipilimumab may cause impairment of the outer retinal layer. We suggest that this is a presumed ipilimumab-induced SRD.
Keywords: ipilimumab, metastatic malignant melanoma, serous retinal detachment
Introduction
Ipilimumab is an immune checkpoint inhibitor that is widely used in the treatment of patients with metastatic malignant melanoma. Ipilimumab blocks cytotoxic T-lymphocyte-associated antigen 4 (CTLA-4), thereby leading to enhanced T-cell activation for the tumor. CTLA-4 also presents on the surface of regulatory T-cells, and inhibits regulatory T-cells that can lead to enhanced tumor immunity.1 However, this immune checkpoint inhibitor can induce related adverse events in various organs. For example, systemic complications such as type Ⅰ diabetes, hypothyroidism, hypopituitarism, colitis and hepatitis have been reported. Ophthalmologic complications have also been reported and include iridocyclitis, optic neuritis,2 chorioretinitis and Vogt-Koyanagi-Harada-like syndrome with impaired hearing and vitiligo.3
Recently, remarkable advances in optical coherence tomography (OCT) have made it possible to detect and clearly visualize horizontal and vertical 12 mm B-scanned images.
Here, we report characteristic findings found in swept-source OCT (SS-OCT) images obtained in a case of bilateral drug (ipilimumab)-induced serous retinal detachment.
Case Report
A 78-year-old man had exanthema on his head and visited the Department of Dermatology in the general hospital in October 2009. It was removed by surgery. Pathological examinations of the removed specimens led to a diagnosis of malignant melanoma. He received a course of follow-up examinations for 4 years because the cancer did not metastasize. Then, the malignant lesions were found to have spread to the right lung, which were then removed during an additional surgery. He was subsequently diagnosed as T4aN0M1 Stage IV. Based on a second opinion, he visited the Department of Dermatology in our hospital and he elected to receive 4 cycles of dacarbazine, nimustine, vincristine, and interferon-beta starting in January 2014. After finding new metastasis in the liver and lungs, he was additionally administered nivolumab. However, 3 months later, further metastasis to the bones, pleura, and peritoneum were found. Therefore, in June 2017, it was decided to start the patient on a new treatment with ipilimumab. He had received ipilimumab at 3mg/kg (weight of him was 55.5kg) every 3 weeks for 4 cycles according to the protocol. After 2 cycles of ipilimumab, the patient noticed impairment of the visual field in both of his eyes at 22 days after the last administration and visited our department in August.
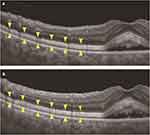
At his initial visit, best corrected visual acuity was 16/20 in both eyes and there were no abnormal findings in either the anterior chamber or optic media. Fundus examination revealed serous retinal detachment (SRD) and several retinal pigment epithelial detachments in both eyes (Figure 1). Fluorescein angiography (Spectralis HRA+OCT; Heidelberg Engineering GmbH) revealed no obvious leakage in either of the SRD areas. Indocyanine green angiography (Spectralis HRA+OCT; Heidelberg Engineering GmbH) showed neither leakage during both the early and late phases nor any abnormal choroidal hyperpermeability (Figure 2). SS-OCT (Topcon DRI OCT Triton Swept Source OCT, Topcon, Japan) identified SRD accompanied by a widely distributed high reflection of the photoreceptor outer segment when using the horizontal and vertical 12 mm B-scanned images. High reflection of the photoreceptor outer segment was detected in both areas where the SRD appeared and did not appear. In normal retina, ellipsoid zone and interdigitation zone are distinguishable, however in these suffered areas, the distribution of the high reflection was not used to differentiate between the interdigitation zone and the ellipsoid zone. SS-OCT also detected thickening (maximum diameter 75 μm) of the photoreceptor outer segment (Figure 3). Fundus autofluorescence (FAF) showed there were no abnormalities (Figure 4). After this evaluation, he was administered 4 cycles of ipilimumab. During his course of follow-up examinations, initially there was a slight increase in the SRD during 4 cycles of ipilimumab, after which the SRD then gradually decreased, and the impairment of his visual field stabilized. Although best corrected visual acuity was 16/20 in both eyes, the SRD and obscurity of the interdigitation zone remained (Figure 5). He had hyperopia at the initial visit and no shift occurred during a course of follow-up examinations.
 |
Figure 4 Autofluorescence at the initial visit. The right and left eye exhibited no abnormal hyperfluorescence in the macular area. |
Discussion
SS-OCT performed in a case of malignant melanoma treated by ipilimumab revealed SRD in both eyes. This was accompanied by high reflection and thickening of the photoreceptor outer segment that resulted from the indistinguishability of the interdigitation and ellipsoid zones. These regions corresponded to the area where the SRD appeared and the adjacent macular area. These results suggest that ipilimumab may cause impairment of the outer retinal layer.
Several clinicians have reported on cases with ocular side effects of ipilimumab, with the typical cases of immune-related ocular side effects appearing to be similar to Vogt-Koyanagi-Harada-like syndrome.2,3 However, our current case did not have findings suggestive of Vogt-Koyanagi-Harada-like syndrome, nor did it have any typical angiographic findings which suggested the presence of central serous chorioretinopathy (CSC).
SS-OCT evaluations in this case did reveal characteristic images of the outer retinal layer including: 1) high reflection in the area where the SRD appeared and in the adjacent retinal area, 2) the interdigitation zone was indistinguishable in the area where the high reflection appeared, and 3) there was thickening of the photoreceptor outer segment in the same area. A previous study that used OCT to examine CSC patients reported finding elongation of the photoreceptor outer segment in these subjects.4 Although elongation of the photoreceptor outer segment was also detected in our current case, the high reflection of the photoreceptor outer segment that we additionally observed in the adjacent outer retina was not seen in patients with typical CSC (Figure 6). Matsumoto et al reported that fundus granular-hyperfluorescence in SRD was observed in the FAF patterns in CSC.5 Even so, FAF did not identify any prominent abnormalities in our case (Figure 4). Based on these findings, it is our belief that ipilimumab was responsible for the damage in the outer retina, and this is a presumed ipilimumab-induced SRD.
It has been reported that OCT can be used in commotio retinae cases to detect thickening and high reflection of the outer part of the photoreceptor that have been recently interpreted as being the ellipsoid zone.6 Evaluations of histological sections from commotio retinae specimens have shown the presence of intercellular edema of the glial cells and fragmentation of the photoreceptor outer segment.6,7 Thus, these histological changes may correspond to the thickening and high reflection of the outer part of the photoreceptor. In addition, the swelling observed at the junction between the inner and outer segment of the photoreceptor in the retinal light damage model may cause the undistinguishable detection of the retinal pigment epithelium and ellipsoid bands in the OCT images.8 To our knowledge, there were two reports that showed similar OCT findings to those in our case during the course of chemotherapy with immune checkpoint inhibitor for malignant melanoma.9 Recently, Sandhu et al reported a case of paraneoplastic polymorphous vitelliform maculopathy during vemurafenib and pembrolizumab treatment and OCT findings were similar to those in our case.10
In our current case, the overall high reflection and thickening of the photoreceptor outer segment observed by the SS-OCT might have been due to the destruction of the photoreceptor outer segment that was potentially impaired by ipilimumab.
Although ipilimumab treatment was continued after the appearance of SRD due to the priority of dealing with the patient’s general condition, his visual acuity was maintained. Ipilimumab therapy is currently only used in patients with malignant melanoma, recent indications have suggested that the use of ipilimumab will be expanded to non-small cell lung cancer, small cell lung cancer, and bladder cancer. Ophthalmic complications directly connected to ipilimumab therapy are rare, with an incidence of less than 1%.11 Even so, there should be careful follow-up examinations in patients receiving ipilimumab due to a potential increase in ocular complications related to the administration of ipilimumab.
Findings for our current case suggest that ipilimumab may impair the outer retinal layer over a wide range, and thus patients being administered ipilimumab are required to undergo ophthalmic evaluations using OCT.
Ethics Statement
Written informed consent for the publication of the case details was obtained from the patient in this case report. Institutional approval was not required to publish the case details.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Watanabe E, Kishida T and Mazda O. Fundamentals of the tumor immunotherapy. J Kyoto Pref Univ Med. 2017;126(6):377–389.
2. Hahn L, Pepple KL. Bilateral neuroretinitis and anterior uveitis following ipilimumab treatment for metastatic melanoma. J Ophthal Inflamm Infect. 2016;6(1):14. doi:10.1186/s12348-016-0082-3
3. Wong RK, Lee JK, Huang JJ. Bilateral drug (ipilimumab)-induced vitritis, choroiditis, and serous retinal detachments suggestive of vogt-koyanagi-harada syndrome. Retin Cases Brief Rep. 2012;6(4):423–426. doi:10.1097/ICB.0b013e31824f7130
4. Matsumoto H, Kishi S, Otani T, Sato T. Elongation of photoreceptor outer segment in central serous chorioretinopathy. Am J Ophthalmol. 2008;145(1):162–168. doi:10.1016/j.ajo.2007.08.024
5. Matsumoto H, Kishi S, Sato T, Mukai R. Fundus autofluorescence of elongated photoreceptor outer segments in central serous chorioretinopathy. Am J Ophthalmol. 2011;151(4):617–623 e1. doi:10.1016/j.ajo.2010.09.031
6. Itakura H, Kishi S. Restored photoreceptor outer segment in commotio retinae. Ophthalmic Surg Lasers Imaging. 2011;42 Online:e29–e31. doi:10.3928/15428877-20110224-03
7. Mansour AM, Green WR, Hogge C, Histopathology of commotio retinae. Retina. 1992;12(1):24–28. doi:10.1097/00006982-199212010-00006
8. Mukai R, Akiyama H, Tajika Y, Shimoda Y, Yorifuji H, Kishi S. Functional and morphologic consequences of light exposure in primate eyes. Invest Ophthalmol Vis Sci. 2012;53(10):6035–6044. doi:10.1167/iovs.12-9608
9. Mantopoulos D, Kendra KL, Letson AD, Cebulla CM. Bilateral choroidopathy and serous retinal detachments during ipilimumab treatment for cutaneous melanoma. JAMA Ophthalmol. 2015;133(8):965–967. doi:10.1001/jamaophthalmol.2015.1128
10. Sandhu HS, Kolomeyer AM, Lau MK, et al. Acute exudative paraneoplastic polymorphous vitelliform maculopathy during vemurafenib and pembrolizumab treatment for metastatic melanoma. Retin Cases Brief Rep. 2019;13(2):103–107. doi:10.1097/ICB.0000000000000604
11. Hodi FS, O’Day SJ, McDermott DF, et al. Improved survival with ipilimumab in patients with metastatic melanoma. N Engl J Med. 2010;363(8):711–723. doi:10.1056/NEJMoa1003466
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.