Back to Journals » Clinical, Cosmetic and Investigational Dermatology » Volume 15
A Case of Giant Basal Cell Carcinoma of the Ear Complicated by Primary Cutaneous Aspergillosis
Authors Yao Y, Li T, Huang Y, Cheng H
Received 10 October 2022
Accepted for publication 13 December 2022
Published 23 December 2022 Volume 2022:15 Pages 2841—2844
DOI https://doi.org/10.2147/CCID.S392871
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Anne-Claire Fougerousse
Yabo Yao, Tianhao Li, Yuanen Huang, Hongbin Cheng
Department of Dermatology, Hospital of Chengdu University of Traditional Chinese Medicine, Chengdu, People’s Republic of China
Correspondence: Hongbin Cheng, Department of Dermatology, Hospital of Chengdu University of Traditional Chinese Medicine, No. 39, Shi-er-qiao Road, Jinniu District, Chengdu, People’s Republic of China, Email [email protected]
Abstract: A 78-year-old female patient with right ear agenesis presented with a skin manifestation of approximately 7 cm × 8 cm deep-invasive ulcer with well-defined borders and a small amount of yellow purulent discharge visible at the base, surrounded by pearl-like margins in a dyke-like elevation, covered with a small amount of necrotic tissue and black crust. The disease lasted for more than 20 years and was diagnosed as giant basal cell carcinoma complicated by primary cutaneous aspergillosis after two histopathological examinations of the skin lesions. There are similarities in the clinical manifestations of these two diseases, which need to be differentiated, and the simultaneous complications are infrequent. It has not been reported.
Keywords: giant basal cell carcinoma, primary, cutaneous aspergillosis
Case Report
A 78-year-old woman presented to the dermatology department with a skin ulcer with pain around her right ear for more than 20 years. The patient developed a nodule the size of a pea-sized behind her right ear with no apparent cause 20 years ago, accompanied by itching. Since then, the lesion gradually expanded and formed an ulcer with painful itching. She was previously in good health with no underlying disease and no similar family history.
On physical examination, a deep ulcer of about 7cm × 8cm with clear borders is visible in the right ear, a small amount of yellow purulent discharge is visible at the base, surrounded by pearl-like edges in a dyke-like elevation, covered with a small amount of necrotic tissue and black scabs, and the right ear is absent (Figure 1).
 |
Figure 1 Clinical feature. The lesion on the right ear. |
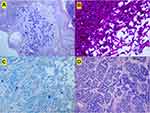
Blood tests showed haemoglobin 108 g/L, red cell count 3.65×1012/L, C-reactive protein 11.83 mg/L, and Immunoglobulin E 1660 IU/mL. Mycobacteria were detected in stool 1–2. Bacterial culture of skin lesion secretions isolated Klebsiella oxytoca and Proteus mirabilis. Fungal D-glucan test, aspergillus galactomannan, the fungal smear of skin lesion secretions and culture were negative. CT scans of the head and chest showed brain atrophy, right middle ear mastoiditis, scattered foci of fibrosis in both lungs, and left pleural thickening. Histopathological examination of the lesions showed visible Aspergillus clusters, mostly neutrophil-dominated inflammatory necrotic tissue and keratinized epithelium (Figure 2A). Periodic Acid-Schiff stain showed fungal hyphae, which were septate and branched (Figure 2B). Alcian blue staining shows fungal mycelium and spores (Figure 2C). The initial diagnosis was primary cutaneous aspergillosis, and there was no significant improvement after 2 months of treatment with itraconazole capsules (200 mg bid). A second histopathological examination showed a basal cell-like tumor mass in the dermis with extensive infiltration between the fibers and a fenestrated arrangement of cells around the mass (Figure 2D). No fungus was seen in the lesion on this histopathological examination. A diagnosis of giant basal cell carcinoma complicated by primary cutaneous aspergillosis disease was made. Surgical excision was recommended, but the patient refused due to financial reasons and continuous follow-up.
Discussion
Basal cell carcinoma (BCC) is the most common skin tumor in the human body, which is more common in older people and more common in men than women, with a male-to-female ratio of about 2:1.1 Ultraviolet radiation and PTCH1 gene mutations are its main causative factors, and inactivating mutations of PTCH1 are found in 90% of patients with sporadic BCC.2 Surgical resection is effective for most primary BBC, with a less than 2–8% recurrence rate at 5 years after surgery.3 In addition to conventional surgical therapy, Mohs microsurgery can be used, which has the advantage of completely removing tumor cells by histopathological examination and maximum preservation of normal tissue. Giant basal cell carcinoma (GBCC) refers to BCC with a diameter of ≥5 cm, and this clinical subtype is rare, accounting for about 0.5–1% of BBCs.4 GBCC is aggressive and can infiltrate deep tissues involving muscle, cartilage, and bone, and may metastasize, so the prognosis is often poor.5,6
Aspergillus is widely present in cereals, soil, air, and other nature and is a common opportunistic pathogenic fungus. Primary Cutaneous Aspergillosis is the direct invasion of pathogenic fungi into damaged skin, such as trauma sites, burns, intravenous catheters, surgical wounds, and closed dressing impregnated areas. Clinical lesions present in a variety of ways, including erythema, ulcers, papules, and nodules. The characteristic pathological manifestation of cutaneous aspergillosis can be seen as clear, separated mycelium branched at 45°. Treatment includes amphotericin B, itraconazole, or terbinafine.
Conclusion
Our patient suffered from BCC, which caused the ear ulcers for a long time, and the skin barrier was destroyed during the period without regular and standardized treatment, and coupled with long-term agricultural activities, the huge ulcerated surface was exposed to the air, leading to opportunistic infection by Aspergillus, which further aggravated and concealed the disease. After antifungal treatment, the fungal infection at the ulcer improved, and at this time, no fungal organism was seen on pathological biopsy, which allowed the diagnosis of BCC to be confirmed.
We presented a rare case of basal cell carcinoma complicated by primary cutaneous aspergillosis. Two biopsies were performed successively in combination with history and physical examination, and the diagnosis was finally confirmed. Early detection and diagnosis as well as early treatment are of great benefit to this disease. Many primary dermatologists do not know enough about skin cancer, so there are some difficulties in the diagnosis of such disease. We suggest more medical training to improve the diagnostic ability of skin tumors to better serve patients.
Ethics Statement
Written informed consent for publication of their clinical details and clinical images was obtained from the proxy. No institutional approval was required.
Funding
This work was supported by Sichuan Provincial Department of Science and Technology Key R&D Program (No.2022YFS0413) and Hospital of Chengdu University of TCM Scientific Research Capacity Enhancement “Hundred Talents Program” (No.P2020042).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Asgari MM, Moffet HH, Ray GT, et al. Trends in basal cell carcinoma incidence and identification of high-risk subgroups, 1998–2012. JAMA Dermatol. 2015;151(9):976–981. doi:10.1001/jamadermatol.2015.1188
2. Peris K, Fargnoli MC, Garbe C, et al. Diagnosis and treatment of basal cell carcinoma: European consensus-based interdisciplinary guidelines. Eur J Cancer. 2019;118:10–34. doi:10.1016/j.ejca.2019.06.003
3. Trakatelli M, Morton C, Nagore E, et al. Update of the European guidelines for basal cell carcinoma management. Eur J Dermatol. 2014;24(3):312–329. doi:10.1684/ejd.2014.2271
4. Betti R, Inselvini E, Moneghini L, et al. Giant basal cell carcinomas: report of four cases and considerations. J Dermatol. 1997;24(5):317–321. doi:10.1111/j.1346-8138.1997.tb02797.x
5. Archontaki M, Stavrianos SD, Korkolis DP, et al. Giant Basal cell carcinoma: clinicopathological analysis of 51 cases and review of the literature. Anticancer Res. 2009;29(7):2655–2663.
6. Lorenzini M, Gatti S, Giannitrapani A. Giant basal cell carcinoma of the thoracic wall: a case report and review of the literature. Br J Plast Surg. 2005;58(7):1007–1010. doi:10.1016/j.bjps.2005.04.017
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.