Back to Journals » Journal of Pain Research » Volume 15
A Bibliometric Analysis of the Top 100 Cited Articles in Anterior Cervical Discectomy and Fusion
Authors Wang X, Lin Y, Wang Q, Gao L, Feng F
Received 22 May 2022
Accepted for publication 23 September 2022
Published 11 October 2022 Volume 2022:15 Pages 3137—3156
DOI https://doi.org/10.2147/JPR.S375720
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Professor Krishnan Chakravarthy
Xun Wang,1 Yanze Lin,1 Qiongtai Wang,1 Liqing Gao,1 Fabo Feng2
1Zhejiang Chinese Medical University, Hangzhou, Zhejiang 310053, People’s Republic of China; 2Center for Plastic & Reconstructive Surgery, Department of Orthopedics, Zhejiang Provincial People’s Hospital (Affiliated People’s Hospital, Hangzhou Medical College), Hangzhou, Zhejiang, 310014, People’s Republic of China
Correspondence: Fabo Feng, Center for Plastic & Reconstructive Surgery, Department of Orthopedics, Zhejiang Provincial People’s Hospital (Affiliated People’s Hospital, Hangzhou Medical College), Hangzhou, Zhejiang, 310014, People’s Republic of China, Email [email protected]
Study design: A bibliometric analysis.
Objective: To identify and analyze the top 100 cited articles in anterior cervical discectomy and fusion.
Summary of Background Data: Anterior cervical discectomy and fusion (ACDF) is one of the most routine surgical procedures in spine surgery. Many surgeons and academics have researched ACDF thoroughly and published numerous articles. However, there is no relevant bibliometric analysis. Therefore, our study aims to identify and analyze the top 100 cited articles in ACDF to identify the research trends.
Methods: We searched the Web of Science (WOS) Core Collection database with restrictions and identified the top 100 cited publications in ACDF for analysis.
Results: The citation counts of the top 100 cited publications ranged from 37 to 361 (mean 67.42). All studies were published between 2008 and 2019, with 2013 and 2015 the most prolific years. The journals Spine and Journal of Neurosurgery-Spine provided the majority of the articles. Overall, the 100 articles came from 12 countries, with the United States being the top producer, followed by China and South Korea. The most frequent keywords were “spine”, “anterior cervical discectomy and fusion”, “interbody fusion”, ‘arthrodesis’, “follow-up”, “decompression”, and “ACDF”.
Conclusion: ACDF has been regarded as a classical gold standard in anterior cervical surgery, and the emergence of new surgical procedures has not affected its status. Cervical disc arthroplasty still needs further research and development. As the first bibliometric analysis of ACDF, this bibliometric study is meant to provide guidance for clinicians and scholars to research the development trend of this field.
Keywords: anterior cervical discectomy and fusion, ACDF, citation analysis, bibliometric, Web of Science, VOSviewer
Introduction
Compared with the lumbar sacral or thoracic spine, anterior access to the cervical is very typical.1–3 Since the introduction of anterior cervical discectomy and fusion (ACDF) in the 1950s, it has been commonly used for treating cervical spine diseases due to its superior clinical efficacy and credible safety4 and has become one of the most common surgical procedures in spine surgery.5,6 The procedure involves the removal of the diseased disc and the implantation of autogenous or allograft implants to restore the stability of the operative vertebral body and achieve direct anterior decompression.7 Indications for ACDF include cervical degenerative disc disease (CDDD), cervical spinal stenosis, and partial ossification of the posterior longitudinal ligament (OPLL).8–10 In recent years, cervical disc arthroplasty (CDA), endoscopic spine surgery (ESS), and other procedures have developed rapidly and have been used to treat cervical spine diseases. CDA preserves the operating segment’s range of motion and reduces the occurrence of adjacent segment degeneration (ASD).11 ESS is considered a safe and effective alternative for cervical spine diseases in the future due to minor tissue damage and fewer complications.12 However, whether CDA and ESS will affect the development trend of ACDF is still unknown.
There are many clinicians and scholars who study ACDF procedure worldwide and have published a large number of valuable reference articles. In recent years, with the rise of surgical methods such as CDA and cervical endoscopic surgery, as well as the development of precision medicine and rehabilitation medicine, the development trend of ACDF may also change. However, to the best of our knowledge, no scholar has conducted a comprehensive analysis of ACDF to identify the most influential research in this field. Therefore, our study is meant to define and analyze the list of top 100 cited papers in ACDF, summarize the research types, identify the research trend in this field, and analyze whether the emergence of new technologies will impact the status of ACDF as the gold standard.
Bibliometrics analysis is the qualitative and quantitative evaluation of research in a specific field by applying multiple methods, which have been commonly used in spine surgery. The number of citations for each article is one of the indicators to evaluate the value of the article. A high citation number means more scholars’ recognition and greater contribution to the field’s development. To our knowledge, this study is the first bibliometric analysis of ACDF. We analyzed research trends based on the most influential articles in ACDF in our study.
Materials and Methods
Search Strategy
We thoroughly searched the WOS Core Collection database to ascertain the top 100 cited articles in ACDF published between 1985 and 2022 on JAN 22, 2022. The specific search strategies are as follows: using CNKI (China national knowledge infrastructure) to identify keywords and synonyms: “anterior cervical discectomy and fusion”, “anterior cervical discectomy with fusion” and “ACDF”. Then, search the WOS Core Collection database with the keywords and synonyms identified. Select “Article” or “Review” publications published in English between 1985 and 2022.
The query is as follows: (((TI=(anterior cervical discectomy with fusion OR anterior cervical discectomy and fusion OR ACDF)) AND DT=(Article OR Review)) AND LA=(English)) AND PY=(1985–2022). A total of 890 articles were searched. All articles were arranged from most to least cited. The top 100 were exported, with title, author, citation number, country, journal, year of publication, and article number noted for further analysis.
Data Analysis
According to the title and abstract, each publication was allocated to a study type and grouped into diagnostic, therapeutic, prognostic, economic, systemic, or non-systemic reviews. The data was analyzed using VOSviewer and Microsoft Excel 2019. VOSviewer is a Java-based software that can analyze and visualize bibliometrics data. We used VOSviewer to build visual co-occurrence networks of the author, keyword, and year of publication. We used Microsoft Excel 2019 to convert data from the WOS Core Collection database into tables and figures.
Result
Basic Characteristics
A total of 890 ACDF-related publications were retrieved and ranked in descending order according to citation frequency. We selected the top 100 articles and marked them from No.1 to 100 (Table 1).6,9,13–110 The citations of the top 100 papers were between 37 and 361 times, with 6742 total and 67.42 mean. Among the articles,
Results of the prospective, randomized, controlled multicenter Food and Drug Administration investigational, device exemption study of the ProDisc-C total disc replacement versus anterior discectomy and fusion for the treatment of 1-level symptomatic cervical disc disease
 |
Table 1 The Top 100 Cited Publications in ACDF |
by Murrey, D et al was the highest cited article.
There were seventeen systematic reviews, nine non-systematic reviews, and seventy-four primary studies among the top 100 publications.
Distribution of Publication Years
All studies were published between 2008 to 2019. From 2013 to 2015, 42 highly cited articles were published, which was the most active period. The most productive year was 2013 (17 publications), followed by 2015 (14 publications) (Figure 1). The earliest article was “Anterior cervical discectomy and fusion for unstable traumatic spondylolisthesis of the axis” by Ying, Z et al in Feb 2008. The latest article was “Machine learning for prediction of sustained opioid prescription after anterior cervical discectomy and fusion” published in 2019 by Karhade, AV et al
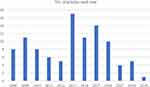 |
Figure 1 Total number of articles published per year. |
Distribution of Authors
In terms of the number of author publications, there are 89 first authors among the top 100 articles and ten first authors with more than two articles. With three articles (No.30, 52, 74 in Table 1), Lied, B was considered the most prolific first author, and the other nine authors contributed two articles per person (Table 2).
 |
Table 2 Authors with More Than Two Articles |
VOSviewer’s Density Visualization function visualizes the co-author relations between all authors by clustering them (Figure 2). Phillips FM, McAfee PC, Howell KM, and five other authors were part of the primary cluster. Anderson PA and three additional authors formed another significant cluster.
 |
Figure 2 VOSviewer density visualization shows co-authorship and clusters among all authors in the top 100 cited articles. |
Distribution of Country/Region and Institution
We identified 81 institutions based on correspondence addresses, and 15 institutions had repeatedly published articles (Table 3). The top three institutions were Rush Univ, USA, Carolina Neurosurg & Spine Associates, USA, and Soochow Univ, China, with three publications each. In terms of countries and regions, twelve different countries and regions contributed to the top 100 articles, among which the United States, with 65 articles, contributed 60.2% of all articles and 66.5% of total citations, followed by China (17 articles) and Korea (8 articles) (Figure 3). Moreover, all articles from North America were contributed by the United States, with 65 articles and 4671 citations. China, Korea, and Japan are the primary sources of Asian articles, with 27 articles and 1537 citations in total. Articles from Europe were composed of seven countries (Norway, United Kingdom, Germany, Italy, Netherlands, Denmark, and Switzerland), with 12 articles and 595 citations. Oceania had only four articles (216 citations) published by Australia. Yet, no publications from South America and Africa were included (Figure 4).
 |
Table 3 Institutions with More Than Two Articles |
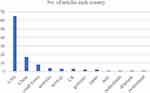 |
Figure 3 Articles published by each country. |
 |
Figure 4 Map of worldwide research productivity. |
Distribution of Publication Journals
The top 100 articles retrieved in our study were from 21 different journals (Table 4), and the top three journals account for 51% of all articles. Spine ranked first with 24 articles, followed by Journal of Neurosurgery-Spine (15 articles) and Spine Journal (12 articles) (Figure 5). Unsurprisingly, Spine has an absolute advantage in the total number of citations (1434 times). However, the journal with the highest average citations was Journal of Bone And Joint Surgery-American Volume (100.5 times), followed by Spine Journal (93.5 times) and Journal of Neurosurgery-Spine (81.5 times).
 |
Table 4 The Total Amount of Articles in Each Journal |
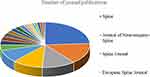 |
Figure 5 The number of articles published in each journal. |
Distribution of Article Types and Keywords
Categorizing all the articles, we found that “therapeutic” (n=65) was the most common type, followed by systemic reviews (n=17), non-systemic reviews (n=9), and “prognostic” (n=9) (Table 5).
 |
Table 5 Categorizing by Article Types |
The co-occurrence network analysis function of VOSviewer was used to analyze the keywords with a minimum frequency of eight. The 33 high-frequency keywords were divided into “procedure”, “disease and symptoms”, and “prognosis” (Figure 6). Overall, the most frequent keyword was “spine” (38), followed by “anterior cervical discectomy and fusion” (36), “interbody fusion” (34), “arthrodesis” (32), “follow-up” (26), “decompression” (23), and “ACDF” (22).
Discussion
ACDF represents one of the most popular procedures in spine surgery.111,112 In 1958, Smith and Robinson firstly described the application of anterior cervical approach as the therapeutic of spine disorders.113 Since then, with numerous modifications introduced by surgeons, ACDF has been considered a gold standard for cervical spondylosis, and the number of related publications has steadily increased. As far as we know, no scholar has conducted a comprehensive analysis of ACDF to define the most significant studies. Our article is the first to analyze ACDF by bibliometric analysis.
According to our study, the publications related to ACDF showed a steady increasing trend before 2013, while the number of articles published in 2013 increased by 240% compared with 2012. From 2013 to 2019, 62% of highly cited articles were published in the seven years. This trend indicated that ACDF research had attracted more attention in recent years, which may relate to an increased risk of cervical spondylosis caused by the aging population and lousy lifestyle such as using smartphones for a long time.114 The earliest article in our study was published by Ying, Z et al on February 1, 2008, and the most cited one was published by Murrey, D et al in April 2009. ACDF was initially described in 1958, and Cloward used Wiltberger’s lumbar interbody dowel fusion procedure on the cervical spine in November of the same year.4 To date, ACDF has long been considered the initial and gold standard of anterior cervical surgery.115–117 Interestingly, Ying, Z et al creatively described the application of ACDF in treating spondylolisthesis of the axis. They believed ACDF might be a feasible surgical procedure for unstable traumatic spondylolisthesis of the axis (TSA),100 which provided a reference for applying ACDF in treating other cervical spine diseases. The surgical procedure of ACDF has been unchanged for more than 60 years, recognizing its reliability and effectiveness. However, more trials and innovations are necessary to push it forward.117
In terms of national publications, the United States dominates with 65% of the total (Figure 3). This might be due to the following reasons: As previously mentioned, the ACDF was first described and modified by American scholars. Among the first ten articles in the top 100, nine articles were published by institutions in the United States. Moreover, in the United States, ACDF is the most routinely performed cervical spine procedure, with more than 500,000 ACDF procedures performed between 1990 to 1999 alone. The clinical outcomes of most cases were good or excellent.111 According to a recent study, 1,212,475 ACDFs were performed in the United States between 2004 and 2014, accounting for more than 80% of cervical spine procedures.118 The United States still dominated the institution publications: 11 of the 15 most productive institutions were affiliated to the United States (Table 3), explaining why the United States leads the world in total publications.
In terms of research topic and hotspot, we found the top four high-frequency keywords were “spine”, “anterior cervical discectomy and fusion”, “interbody fusion”, and “arthrodesis”. Meanwhile, through the analysis of the title and abstract, we found that the procedures comparison (n=36) was the most common topic type, especially ACDF versus CDA (n=28). Therefore, we concluded that the comparison between ACDF and CDA was a contemporary research hotspot in cervical surgery and had received significant attention. The articles by Murrey, D et al with the most total cited and the highest average number of citations and their latest publication on cervical surgery were reviews involving the ACDF versus CDA. ACDF is regarded as the standard surgical procedure for CDDD.119 However, in addition to the common complications of ACDF, there are rare but disastrous complications, such as esophageal tear, pharyngeal perforation, and even expectoration of the entire ACDF construct.120 Moreover, several publications showed that changes in the biomechanical of adjacent segments after ACDF may result in adjacent segment degeneration (ASD).121 CDA was introduced to protect spinal biomechanics and reduce the incidence of ASD.122 In 1966, Fernstrom introduced the concept of CDA.123 Limited by the technology available at the time, the initial device was a ball bearing implanted in the lumbar disc space. After more than 50 years of development, the artificial discs used in the clinic have the characteristics of bionic, stable, and shock absorption.124 Nine artificial discs have received US FDA approval: Prestige ST, Prestige LP, Prodisc-C, Bryan, Secure-C, PCM, Mobi-C, M6-C, and Simplify.125 Compared with ACDF, CDA was superior or equivalent in terms of length of stay (LOS), clinical indicators, range of motion (ROM) of the cervical spine, adverse events, and reoperation rates.29,97,109,126 Although CDA has some advantages over ACDF in surgical outcomes, the indications of CDA are relatively narrow, the procedure is more complex,117,119 and the financial requirements of patients are higher,127 all of which limit the application of CDA in the clinic. Some scholars believe that postoperative complications of CDA, such as heterotopic ossification (HO), osteolysis, and aseptic loosening caused by abrasion, spontaneous fusion, and postoperative hematoma, are also one of the factors limiting its wide application.125,128 Since Food and Drug Administration (FDA) approved CDA in 2007, the growth rate of CDA has reached a steady-state, about twice that of ACDF.129 In a recent investigation by Comron Saifi et al, in the United States alone, approximately 132,000 ACDFs are performed each year compared to only 1600 CDAs, with a ratio of 81:1.51 Junbo He et al analyzed the top 100 cited publications on anterior cervical surgery and found that 80% of the publications were related to ACDF.117 As a representative of minimally invasive spine surgeries (MISS), endoscopic spine surgery is expected to become the mainstream direction of spine surgery due to its characteristics of fewer complications and minor tissue damage.130 However, the immaturity of the technique and the long learning cycle deter most spinal surgeons. ACDF is still the gold standard procedure for CDDD.11,130,131
Concerning research trends, CDA and artificial disc have been the research hotspots in recent years (Figure 6). Despite advances in artificial discs in the material, design, and manufacturing technology, wear remains the most influential factor in prosthesis implantation success.132 Aseptic loosening propagated by implant wear is the primary reason for implant failure and reoperation. Meanwhile, debris from wear induces an inflammatory response at the surgical level, leading to pain in the area surrounding the prosthesis.124 Researchers argued that disc neovascularization is the cornerstone of new-onset pain, and more investigations into this factor should be increased over the next five years.133
As a bibliometric to analyze the top 100 cited articles, our study has the following limitations: firstly, all the articles were published between 2008 to 2019. Like other bibliometric studies, “cumulative effect” is inevitable in our study, which means the earlier articles may have more citations. In contrast, the high-quality articles published recently may not be included due to the low citation.134,135 Secondly, we only retrieved English publications from the WOS, which might have omitted high-impact articles from other databases or languages. Finally, citation numbers may not be the sole standard to measure the quality and influence of an article. Other factors should be taken into account comprehensively in the future.
Conclusion
This bibliometric study identified the top 100 cited publications in ACDF, demonstrated the significance of ACDF in spine surgery, and identified the most prominent authors, institutions, countries, and journals. Generally, as the birthplace of ACDF, the United States is the country with the most thorough research in the world and has made outstanding contributions to the development of ACDF. CDA, as an alternative procedure for ACDF, has many limitations and needs further research for improvement. Endoscopic spine surgery is limited in clinical due to its immaturity and long learning period. Therefore, ACDF is still the gold treatment for cervical disc degeneration disease, the emergence of new procedures has not affected its position. As the first bibliometric analysis of ACDF, our study is expected to provide effective guidance for surgeons and researchers to familiarize the most influential publications in this field.
Data Sharing Statement
Research data supporting this publication are available from the Web of Science at located at www.webofknowledge.com.
Ethical Approval
The authors confirmed that no ethical approval is required.
Device Status/Drug Statement
The manuscript submitted does not contain information about medical device(s)/drug(s).
Funding
This research was supported in part by the Natural Science Foundation of Zhejiang Province under grant number LQ19H160014.
Disclosure
The authors have no competing interests to declare that are relevant to the content of this article.
References
1. Medici A, Meccariello L, Falzarano G. Non-operative vs. percutaneous stabilization in Magerl’s A1 or A2 thoracolumbar spine fracture in adults: is it really advantageous for a good alignment of the spine? Preliminary data from a prospective study. Eur Spine J. 2014;(S6):677–683. doi:10.1007/s00586-014-3557-7
2. Cervera-Irimia J, Gonzalez-Miranda A, Riquelme-Garcia O, et al.. Scoliosis induced by costotransversectomy in minipigs model. Med Glas. 2019;16. doi:10.17392/1015-19
3. Cervera Irimia J, Tome-Bermejo F, Pinera-Parrilla AR, et al. Spinal fusion achieves similar two-year improvement in HRQoL as total Hip and total knee replacement. A prospective, multicentric and observational study. SICOT J. 2019;5:26. doi:10.1051/sicotj/2019027
4. Song KJ, Choi BY. Current concepts of anterior cervical discectomy and fusion: a review of literature. Asian Spine J. 2014;8:531–539. doi:10.4184/asj.2014.8.4.531
5. Zadegan SA, Abedi A, Jazayeri SB, et al. Demineralized bone matrix in anterior cervical discectomy and fusion: a systematic review. Eur Spine J. 2017;26:958–974. doi:10.1007/s00586-016-4858-9
6. Zou S, Gao J, Xu B, et al. Anterior cervical discectomy and fusion (ACDF) versus cervical disc arthroplasty (CDA) for two contiguous levels cervical disc degenerative disease: a meta-analysis of randomized controlled trials. Eur Spine J. 2017;26:985–997. doi:10.1007/s00586-016-4655-5
7. Karasin B, Grzelak M. Anterior Cervical Discectomy and Fusion: a Surgical Intervention for Treating Cervical Disc Disease. AORN J. 2021;113:237–251. doi:10.1002/aorn.13329
8. Fujibayashi S, Neo M, Nakamura T. Stand-alone interbody cage versus anterior cervical plate for treatment of cervical disc herniation: sequential changes in cage subsidence. J Clin Neurosci. 2008;15:1017–1022. doi:10.1016/j.jocn.2007.05.011
9. Lee YS, Kim YB, Park SW. Risk factors for postoperative subsidence of single-level anterior cervical discectomy and fusion: the significance of the preoperative cervical alignment. Spine. 2014;39:1280–1287. doi:10.1097/BRS.0000000000000400
10. Noh SH, Kim KH, Park JY, et al. Anterior cervical discectomy and fusion vs posterior laminoplasty for the treatment of myelopathy due to two-level localized ossification of the posterior longitudinal ligament. Medicine. 2020;99(33):e20955. doi:10.1097/md.0000000000020955
11. Mazas S, Benzakour A, Castelain J-E, et al. Cervical disc herniation: which surgery?. Int Orthop. 2019;43(4):761–766. doi:10.1007/s00264-018-4221-3
12. Parihar VS, Yadav N, Ratre S, et al. Endoscopic Anterior Approach for Cervical Disc Disease (Disc Preserving Surgery). World Neurosurg. 2018;115:e599–e609. doi:10.1016/j.wneu.2018.04.107
13. Murrey D, Janssen M, Delamarter R, et al. Results of the prospective, randomized, controlled multicenter Food and Drug Administration investigational device exemption study of the ProDisc-C total disc replacement versus anterior discectomy and fusion for the treatment of 1-level symptomatic cervical disc disease. Spine J. 2009;9:275–286. doi:10.1016/j.spinee.2008.05.006
14. Sasso RC, Anderson PA, Riew KD, et al. Results of cervical arthroplasty compared with anterior discectomy and fusion: four-year clinical outcomes in a prospective, randomized controlled trial. J Bone Joint Surg Am. 2011;93:1684–1692. doi:10.2106/JBJS.J.00476
15. Parker SL, Godil SS, Shau DN, et al. Assessment of the minimum clinically important difference in pain, disability, and quality of life after anterior cervical discectomy and fusion: clinical article. J Neurosurg Spine. 2013;18:154–160. doi:10.3171/2012.10.SPINE12312
16. Buttermann GR. Prospective nonrandomized comparison of an allograft with bone morphogenic protein versus an iliac-crest autograft in anterior cervical discectomy and fusion. Spine J. 2008;8:426–435. doi:10.1016/j.spinee.2006.12.006
17. Zigler JE, Delamarter R, Murrey D, et al. ProDisc-C and anterior cervical discectomy and fusion as surgical treatment for single-level cervical symptomatic degenerative disc disease: five-year results of a Food and Drug Administration study. LWW. 2013. doi:10.1097/BRS.0b013e318278eb38
18. Kim SW, Limson MA, Kim SB, et al. Comparison of radiographic changes after ACDF versus Bryan disc arthroplasty in single and bi-level cases. Eur Spine J. 2009;18:218–231. doi:10.1007/s00586-008-0854-z
19. Davis RJ, Nunley PD, Kim KD, et al. Two-level total disc replacement with Mobi-C cervical artificial disc versus anterior discectomy and fusion: a prospective, randomized, controlled multicenter clinical trial with 4-year follow-up results. J Neurosurg Spine. 2015;22:15–25. doi:10.3171/2014.7.SPINE13953
20. Davis RJ, Kim KD, Hisey MS, et al. Cervical total disc replacement with the Mobi-C cervical artificial disc compared with anterior discectomy and fusion for treatment of 2-level symptomatic degenerative disc disease: a prospective, randomized, controlled multicenter clinical trial: clinical article. J Neurosurg Spine. 2013;19:532–545. doi:10.3171/2013.6.SPINE12527
21. Phillips FM, Geisler FH, Gilder KM, et al. Long-term outcomes of the US FDA IDE prospective, randomized controlled clinical trial comparing PCM cervical disc arthroplasty with anterior cervical discectomy and fusion. LWW. 2015. doi:10.1097/BRS.0000000000000869
22. Veeravagu A, Cole T, Jiang B, et al. Revision rates and complication incidence in single- and multilevel anterior cervical discectomy and fusion procedures: an administrative database study. Spine J. 2014;14:1125–1131. doi:10.1016/j.spinee.2013.07.474
23. Niu CC, Liao JC, Chen WJ, et al. Outcomes of interbody fusion cages used in 1 and 2-levels anterior cervical discectomy and fusion: titanium cages versus polyetheretherketone (PEEK) cages. J Spinal Disord Tech. 2010;23:310–316. doi:10.1097/BSD.0b013e3181af3a84
24. Phillips FM, Lee JY, Geisler FH, et al. A prospective, randomized, controlled clinical investigation comparing PCM cervical disc arthroplasty with anterior cervical discectomy and fusion: 2-year results from the US FDA IDE clinical trial. LWW. 2013. doi:10.1097/BRS.0b013e318296232f
25. Coric D, Kim PK, Clemente JD, et al. Prospective randomized study of cervical arthroplasty and anterior cervical discectomy and fusion with long-term follow-up: results in 74 patients from a single site. J Neurosurg Spine. 2013;18:36–42. doi:10.3171/2012.9.SPINE12555
26. Tumialan LM, Pan J, Rodts GE, et al. The safety and efficacy of anterior cervical discectomy and fusion with polyetheretherketone spacer and recombinant human bone morphogenetic protein-2: a review of 200 patients. J Neurosurg Spine. 2008;8:529–535. doi:10.3171/SPI/2008/8/6/529
27. McAfee PC, Cappuccino A, Cunningham BW, et al. Lower incidence of dysphagia with cervical arthroplasty compared with ACDF in a prospective randomized clinical trial. J Spinal Disord Tech. 2010;23:1–8. doi:10.1097/BSD.0b013e31819e2ab8
28. Janssen ME, Zigler JE, Spivak JM, et al. ProDisc-C Total Disc Replacement Versus Anterior Cervical Discectomy and Fusion for Single-Level Symptomatic Cervical Disc Disease: seven-Year Follow-up of the Prospective Randomized U.S. Food and Drug Administration Investigational Device Exemption Study. J Bone Joint Surg Am. 2015;97:1738–1747. doi:10.2106/JBJS.N.01186
29. Gao Y, Liu M, Li T, et al. A meta-analysis comparing the results of cervical disc arthroplasty with anterior cervical discectomy and fusion (ACDF) for the treatment of symptomatic cervical disc disease. J Bone Joint Surg Am. 2013;95:555–561. doi:10.2106/JBJS.K.00599
30. Shriver MF, Lewis DJ, Kshettry VR, et al. Pseudoarthrosis rates in anterior cervical discectomy and fusion: a meta-analysis. Spine J. 2015;15:2016–2027. doi:10.1016/j.spinee.2015.05.010
31. Chau AM, Mobbs RJ. Bone graft substitutes in anterior cervical discectomy and fusion. Eur Spine J. 2009;18:449–464. doi:10.1007/s00586-008-0878-4
32. McGirt MJ, Godil SS, Asher AL, et al. Quality analysis of anterior cervical discectomy and fusion in the outpatient versus inpatient setting: analysis of 7288 patients from the NSQIP database. Neurosurg Focus. 2015;39:E9. doi:10.3171/2015.9.FOCUS15335
33. Cabraja M, Oezdemir S, Koeppen D, et al. Anterior cervical discectomy and fusion: comparison of titanium and polyetheretherketone cages. BMC Musculoskelet Disord. 2012;13:172. doi:10.1186/1471-2474-13-172
34. Jagannathan J, Shaffrey CI, Oskouian RJ, et al. Radiographic and clinical outcomes following single-level anterior cervical discectomy and allograft fusion without plate placement or cervical collar. J Neurosurg Spine. 2008;8:420–428. doi:10.3171/SPI/2008/8/5/420
35. Adamson T, Godil SS, Mehrlich M, et al. Anterior cervical discectomy and fusion in the outpatient ambulatory surgery setting compared with the inpatient hospital setting: analysis of 1000 consecutive cases. J Neurosurg Spine. 2016;24:878–884. doi:10.3171/2015.8.SPINE14284
36. Song KJ, Lee KB, Song JH. Efficacy of multilevel anterior cervical discectomy and fusion versus corpectomy and fusion for multilevel cervical spondylotic myelopathy: a minimum 5-year follow-up study. Eur Spine J. 2012;21:1551–1557. doi:10.1007/s00586-012-2296-x
37. van Eck CF, Regan C, Donaldson WF, et al. The revision rate and occurrence of adjacent segment disease after anterior cervical discectomy and fusion: a study of 672 consecutive patients. Spine. 2014;39:2143–2147. doi:10.1097/BRS.0000000000000636
38. Radcliff K, Coric D, Albert T. Five-year clinical results of cervical total disc replacement compared with anterior discectomy and fusion for treatment of 2-level symptomatic degenerative disc disease: a prospective, randomized, controlled, multicenter investigational device exemption clinical trial. J Neurosurg Spine. 2016;25:213–224. doi:10.3171/2015.12.SPINE15824
39. Liao JC, Niu CC, Chen WJ, et al. Polyetheretherketone (PEEK) cage filled with cancellous allograft in anterior cervical discectomy and fusion. Int Orthop. 2008;32:643–648. doi:10.1007/s00264-007-0378-x
40. Anderson PA, Subach BR, Riew KD. Predictors of outcome after anterior cervical discectomy and fusion: a multivariate analysis. Spine. 2009;34:161–166. doi:10.1097/BRS.0b013e31819286ea
41. Anakwenze OA, Auerbach JD, Milby AH, et al. Sagittal cervical alignment after cervical disc arthroplasty and anterior cervical discectomy and fusion: results of a prospective, randomized, controlled trial. LWW. 2009. doi:10.1097/BRS.0b013e3181b03fe6
42. Lied B, Roenning PA, Sundseth J, et al. Anterior cervical discectomy with fusion in patients with cervical disc degeneration: a prospective outcome study of 258 patients (181 fused with autologous bone graft and 77 fused with a PEEK cage). BMC Surg. 2010;10:10. doi:10.1186/1471-2482-10-10
43. Gornet MF, Burkus JK, Shaffrey ME, et al. Cervical disc arthroplasty with PRESTIGE LP disc versus anterior cervical discectomy and fusion: a prospective, multicenter investigational device exemption study. J Neurosurg Spine. 2015;23:558–573. doi:10.3171/2015.1.SPINE14589
44. Nassr A, Lee JY, Bashir RS, et al. Does incorrect level needle localization during anterior cervical discectomy and fusion lead to accelerated disc degeneration?. Spine. 2009;34:189–192. doi:10.1097/BRS.0b013e3181913872
45. Uribe JS, Sangala JR, Duckworth EA, et al. Comparison between anterior cervical discectomy fusion and cervical corpectomy fusion using titanium cages for reconstruction: analysis of outcome and long-term follow-up. Eur Spine J. 2009;18:654–662. doi:10.1007/s00586-009-0897-9
46. Park Y, Maeda T, Cho W, et al. Comparison of anterior cervical fusion after two-level discectomy or single-level corpectomy: sagittal alignment, cervical lordosis, graft collapse, and adjacent-level ossification. Spine J. 2010;10:193–199. doi:10.1016/j.spinee.2009.09.006
47. Kelly MP, Mok JM, Frisch RF, et al. Adjacent segment motion after anterior cervical discectomy and fusion versus Prodisc-c cervical total disk arthroplasty: analysis from a randomized, controlled trial. LWW. 2011. doi:10.1097/BRS.0b013e3181ec5c7d
48. Hofstetter CP, Kesavabhotla K, Boockvar JA. Zero-profile Anchored Spacer Reduces Rate of Dysphagia Compared With ACDF With Anterior Plating. J Spinal Disord Tech. 2015;28:E284–90. doi:10.1097/BSD.0b013e31828873ed
49. Gruskay JA, Fu M, Basques BA, et al. Factors Affecting Length of Stay and Complications After Elective Anterior Cervical Discectomy and Fusion: a Study of 2164 Patients From The American College of Surgeons National Surgical Quality Improvement Project Database (ACS NSQIP). Clin Spine Surgery. 2016;29:E34–42. doi:10.1097/BSD.0000000000000080
50. Garringer SM, Sasso RC. Safety of anterior cervical discectomy and fusion performed as outpatient surgery. J Spinal Disord Tech. 2010;23:439–443. doi:10.1097/BSD.0b013e3181bd0419
51. Saifi C, Fein AW, Cazzulino A, et al. Trends in resource utilization and rate of cervical disc arthroplasty and anterior cervical discectomy and fusion throughout the United States from 2006 to 2013. Spine J. 2018;18:1022–1029. doi:10.1016/j.spinee.2017.10.072
52. Sasso RC, Best NM, Metcalf NH, et al. Motion analysis of bryan cervical disc arthroplasty versus anterior discectomy and fusion: results from a prospective, randomized, multicenter, clinical trial. J Spinal Disord Tech. 2008;21:393–399. doi:10.1097/BSD.0b013e318150d121
53. Hu Y, Lv G, Ren S, et al. Mid- to Long-Term Outcomes of Cervical Disc Arthroplasty versus Anterior Cervical Discectomy and Fusion for Treatment of Symptomatic Cervical Disc Disease: a Systematic Review and Meta-Analysis of Eight Prospective Randomized Controlled Trials. PLoS One. 2016;11:e0149312. doi:10.1371/journal.pone.0149312
54. Liu JT, Briner RP, Friedman JA. Comparison of inpatient vs. outpatient anterior cervical discectomy and fusion: a retrospective case series. BMC Surg. 2009;9:3. doi:10.1186/1471-2482-9-3
55. Miller LE, Block JE. Safety and effectiveness of bone allografts in anterior cervical discectomy and fusion surgery. Spine. 2011;36:2045–2050. doi:10.1097/BRS.0b013e3181ff37eb
56. Chung JY, Kim SK, Jung ST, et al. Clinical adjacent-segment pathology after anterior cervical discectomy and fusion: results after a minimum of 10-year follow-up. Spine J. 2014;14:2290–2298. doi:10.1016/j.spinee.2014.01.027
57. Ren C, Song Y, Xue Y, et al. Mid- to long-term outcomes after cervical disc arthroplasty compared with anterior discectomy and fusion: a systematic review and meta-analysis of randomized controlled trials. Eur Spine J. 2014;23:1115–1123. doi:10.1007/s00586-014-3220-3
58. Gornet MF, Lanman TH, Burkus JK, et al. Cervical disc arthroplasty with the Prestige LP disc versus anterior cervical discectomy and fusion, at 2 levels: results of a prospective, multicenter randomized controlled clinical trial at 24 months. J Neurosurg Spine. 2017;26:653–667. doi:10.3171/2016.10.SPINE16264
59. Buerba RA, Giles E, Webb ML, et al. Increased risk of complications after anterior cervical discectomy and fusion in the elderly: an analysis of 6253 patients in the American College of Surgeons National Surgical Quality Improvement Program database. Spine. 2014;39:2062–2069. doi:10.1097/BRS.0000000000000606
60. Jiang SD, Jiang LS, Dai LY. Anterior cervical discectomy and fusion versus anterior cervical corpectomy and fusion for multilevel cervical spondylosis: a systematic review. Arch Orthop Trauma Surg. 2012;132:155–161. doi:10.1007/s00402-011-1402-6
61. Lied B, Sundseth J, Helseth E. Immediate (0-6 h), early (6-72 h) and late (>72 h) complications after anterior cervical discectomy with fusion for cervical disc degeneration; discharge six hours after operation is feasible. Acta Neurochir. 2008;150:111–118. doi:10.1007/s00701-007-1472-y
62. Lee SH, Kim KT, Suk KS, et al. Effect of retropharyngeal steroid on prevertebral soft tissue swelling following anterior cervical discectomy and fusion: a prospective, randomized study. Spine. 2011;36:2286–2292. doi:10.1097/BRS.0b013e318237e5d0
63. Singh K, Phillips FM, Park DK, et al. Factors affecting reoperations after anterior cervical discectomy and fusion within and outside of a Federal Drug Administration investigational device exemption cervical disc replacement trial. Spine J. 2012;12:372–378. doi:10.1016/j.spinee.2012.02.005
64. Qureshi SA, McAnany S, Goz V, et al. Cost-effectiveness analysis: comparing single-level cervical disc replacement and single-level anterior cervical discectomy and fusion: clinical article. J Neurosurg Spine. 2013;19:546–554. doi:10.3171/2013.8.SPINE12623
65. Carrier CS, Bono CM, Lebl DR. Evidence-based analysis of adjacent segment degeneration and disease after ACDF: a systematic review. Spine J. 2013;13:1370–1378. doi:10.1016/j.spinee.2013.05.050
66. Miao J, Shen Y, Kuang Y, et al. Early follow-up outcomes of a new zero-profile implant used in anterior cervical discectomy and fusion. J Spinal Disord Tech. 2013;26:E193–7. doi:10.1097/BSD.0b013e31827a2812
67. Lu DC, Tumialan LM, Chou D. Multilevel anterior cervical discectomy and fusion with and without rhBMP-2: a comparison of dysphagia rates and outcomes in 150 patients. J Neurosurg Spine. 2013;18:43–49. doi:10.3171/2012.10.SPINE10231
68. Chang SW, Kakarla UK, Maughan PH, et al. Four-level anterior cervical discectomy and fusion with plate fixation: radiographic and clinical results. Neurosurgery. 2010;66:639–646. doi:10.1227/01.NEU.0000367449.60796.94
69. Jeyamohan SB, Kenning TJ, Petronis KA, et al. Effect of steroid use in anterior cervical discectomy and fusion: a randomized controlled trial. J Neurosurg Spine. 2015;23:137–143. doi:10.3171/2014.12.SPINE14477
70. Chong E, Pelletier MH, Mobbs RJ, et al. The design evolution of interbody cages in anterior cervical discectomy and fusion: a systematic review. BMC Musculoskelet Disord. 2015;16:99. doi:10.1186/s12891-015-0546-x
71. Tumialan LM, Ponton RP, Gluf WM. Management of unilateral cervical radiculopathy in the military: the cost effectiveness of posterior cervical foraminotomy compared with anterior cervical discectomy and fusion. Neurosurg Focus. 2010;28:E17. doi:10.3171/2010.1.FOCUS09305
72. Trahan J, Abramova MV, Richter EO, et al. Feasibility of anterior cervical discectomy and fusion as an outpatient procedure. World Neurosurg. 2011;75:145–148. doi:10.1016/j.wneu.2010.09.015
73. Njoku I, Alimi M, Leng LZ, et al. Anterior cervical discectomy and fusion with a zero-profile integrated plate and spacer device: a clinical and radiological study: clinical article. J Neurosurg Spine. 2014;21:529–537. doi:10.3171/2014.6.SPINE12951
74. Wang Z, Jiang W, Li X, et al. The application of zero-profile anchored spacer in anterior cervical discectomy and fusion. Eur Spine J. 2015;24:148–154. doi:10.1007/s00586-014-3628-9
75. Buttermann GR. Anterior Cervical Discectomy and Fusion Outcomes over 10 Years: a Prospective Study. Spine. 2018;43:207–214. doi:10.1097/BRS.0000000000002273
76. Bhadra AK, Raman AS, Casey AT, et al. Single-level cervical radiculopathy: clinical outcome and cost-effectiveness of four techniques of anterior cervical discectomy and fusion and disc arthroplasty. Eur Spine J. 2009;18:232–237. doi:10.1007/s00586-008-0866-8
77. Anderson PA, Sasso RC, Hipp J, et al. Kinematics of the cervical adjacent segments after disc arthroplasty compared with anterior discectomy and fusion: a systematic review and meta-analysis. Spine. 2012;37:S85–95. doi:10.1097/BRS.0b013e31826d6628
78. Carreon LY, Anderson PA, Traynelis VC, et al. Cost-effectiveness of single-level anterior cervical discectomy and fusion five years after surgery. Spine. 2013;38:471–475. doi:10.1097/BRS.0b013e318273aee2
79. Bydon M, Xu R, Macki M, et al. Adjacent segment disease after anterior cervical discectomy and fusion in a large series. Neurosurgery. 2014;74:139–146. doi:10.1227/NEU.0000000000000204
80. Barbagallo GM, Romano D, Certo F, et al. Zero-P: a new zero-profile cage-plate device for single and multilevel ACDF. A single institution series with four years maximum follow-up and review of the literature on zero-profile devices. Eur Spine J. 2013;22 Suppl 6:S868–78. doi:10.1007/s00586-013-3005-0
81. Auffinger BM, Lall RR, Dahdaleh NS, et al. Measuring surgical outcomes in cervical spondylotic myelopathy patients undergoing anterior cervical discectomy and fusion: assessment of minimum clinically important difference. PLoS One. 2013;8:e67408. doi:10.1371/journal.pone.0067408
82. Findlay C, Ayis S, Demetriades AK. Total disc replacement versus anterior cervical discectomy and fusion: a systematic review with meta-analysis of data from a total of 3160 patients across 14 randomized controlled trials with both short- and medium- to long-term outcomes. Bone Joint J. 2018;100-B:991–1001. doi:10.1302/0301-620X.100B8.BJJ-2018-0120.R1
83. Lied B, Ronning PA, Halvorsen CM, et al. Outpatient anterior cervical discectomy and fusion for cervical disk disease: a prospective consecutive series of 96 patients. Acta Neurol Scand. 2013;127:31–37. doi:10.1111/j.1600-0404.2012.01674.x
84. Jackson RJ, Davis RJ, Hoffman GA, et al. Subsequent surgery rates after cervical total disc replacement using a Mobi-C Cervical Disc Prosthesis versus anterior cervical discectomy and fusion: a prospective randomized clinical trial with 5-year follow-up. J Neurosurg Spine. 2016;24:734–745. doi:10.3171/2015.8.SPINE15219
85. Karikari IO, Jain D, Owens TR, et al. Impact of subsidence on clinical outcomes and radiographic fusion rates in anterior cervical discectomy and fusion: a systematic review. J Spinal Disord Tech. 2014;27:1–10. doi:10.1097/BSD.0b013e31825bd26d
86. Gao F, Mao T, Sun W, et al. An Updated Meta-Analysis Comparing Artificial Cervical Disc Arthroplasty (CDA) Versus Anterior Cervical Discectomy and Fusion (ACDF) for the Treatment of Cervical Degenerative Disc Disease (CDDD). Spine. 2015;40:1816–1823. doi:10.1097/BRS.0000000000001138
87. Martin CT, Pugely AJ, Gao Y, et al. Thirty-Day Morbidity After Single-Level Anterior Cervical Discectomy and Fusion: identification of Risk Factors and Emphasis on the Safety of Outpatient Procedures. J Bone Joint Surg Am. 2014;96:1288–1294. doi:10.2106/JBJS.M.00767
88. Nunley PD, Jawahar A, Kerr EJ 3rd, et al. Choice of plate may affect outcomes for single versus multilevel ACDF: results of a prospective randomized single-blind trial. Spine J. 2009;9:121–127. doi:10.1016/j.spinee.2007.11.009
89. Song KJ, Taghavi CE, Hsu MS, et al. Plate augmentation in anterior cervical discectomy and fusion with cage for degenerative cervical spinal disorders. Eur Spine J. 2010;19:1677–1683. doi:10.1007/s00586-010-1283-3
90. Lee CH, Hyun SJ, Kim MJ, et al. Comparative analysis of 3 different construct systems for single-level anterior cervical discectomy and fusion: stand-alone cage, iliac graft plus plate augmentation, and cage plus plating. J Spinal Disord Tech. 2013;26:112–118. doi:10.1097/BSD.0b013e318274148e
91. Di Capua J, Somani S, Kim JS, et al. Predictors for Patient Discharge Destination After Elective Anterior Cervical Discectomy and Fusion. Spine. 2017;42:1538–1544. doi:10.1097/BRS.0000000000002140
92. Karhade AV, Ogink PT, Thio Q, et al. Machine learning for prediction of sustained opioid prescription after anterior cervical discectomy and fusion. Spine J. 2019;19:976–983. doi:10.1016/j.spinee.2019.01.009
93. Liu T, Yang HL, Xu YZ, et al. ACDF with the PCB cage-plate system versus laminoplasty for multilevel cervical spondylotic myelopathy. J Spinal Disord Tech. 2011;24:213–220. doi:10.1097/BSD.0b013e3181e9f294
94. Hauerberg J, Kosteljanetz M, Bøge-Rasmussen T, et al. Anterior cervical discectomy with or without fusion with ray titanium cage: a prospective randomized clinical study. LWW. 2008. doi:10.1097/BRS.0b013e3181657dac
95. Xu R, Bydon M, Macki M, et al. Adjacent segment disease after anterior cervical discectomy and fusion: clinical outcomes after first repeat surgery versus second repeat surgery. Spine. 2014;39:120–126. doi:10.1097/BRS.0000000000000074
96. Yang H, Chen D, Wang X, et al. Zero-profile integrated plate and spacer device reduces rate of adjacent-level ossification development and dysphagia compared to ACDF with plating and cage system. Arch Orthop Trauma Surg. 2015;135:781–787. doi:10.1007/s00402-015-2212-z
97. Zhong ZM, Zhu SY, Zhuang JS, et al. Reoperation After Cervical Disc Arthroplasty Versus Anterior Cervical Discectomy and Fusion: a Meta-analysis. Clin Orthop Relat Res. 2016;474:1307–1316. doi:10.1007/s11999-016-4707-5
98. Shiban E, Gapon K, Wostrack M, et al. Clinical and radiological outcome after anterior cervical discectomy and fusion with stand-alone empty polyetheretherketone (PEEK) cages. Acta Neurochir. 2016;158:349–355. doi:10.1007/s00701-015-2630-2
99. Phan K, Kim JS, Lee NJ, et al. Relationship Between ASA Scores and 30-Day Readmissions in Patients Undergoing Anterior Cervical Discectomy and Fusion. Spine. 2017;42:85–91. doi:10.1097/BRS.0000000000001680
100. Ying Z, Wen Y, Xinwei W, et al. Anterior cervical discectomy and fusion for unstable traumatic spondylolisthesis of the axis. Spine. 2008;33(3):255–258. doi:10.1097/BRS.0b013e31816233d0
101. Sugawara T, Itoh Y, Hirano Y, et al. Long term outcome and adjacent disc degeneration after anterior cervical discectomy and fusion with titanium cylindrical cages. Acta Neurochir. 2009;151(4):303–309. doi:10.1007/s00701-009-0217-5
102. Burkhardt J-K, Mannion AF, Marbacher S, et al. A comparative effectiveness study of patient-rated and radiographic outcome after 2 types of decompression with fusion for spondylotic myelopathy: anterior cervical discectomy versus corpectomy. Neurosurg Focus. 2013;35(1):E4. doi:10.3171/2013.3.FOCUS1396
103. Kang L, Lin D, Ding Z, et al. Artificial disk replacement combined with midlevel ACDF versus multilevel fusion for cervical disk disease involving 3 levels. Orthopedics. 2013;36(1):e88–94. doi:10.3928/01477447-20121217-24
104. Lubelski D, Healy AT, Silverstein MP, et al. Reoperation rates after anterior cervical discectomy and fusion versus posterior cervical foraminotomy: a propensity-matched analysis. Spine J. 2015;15(6):1277–1283. doi:10.1016/j.spinee.2015.02.026
105. Radcliff K, Zigler J, Zigler J. Costs of cervical disc replacement versus anterior cervical discectomy and fusion for treatment of single-level cervical disc disease: an analysis of the Blue Health Intelligence database for acute and long-term costs and complications. Spine. 2015;40(8):521–529. doi:10.1097/BRS.0000000000000822
106. McClelland III S, Oren JH, Protopsaltis TS, et al.. Outpatient anterior cervical discectomy and fusion: a meta-analysis. Int J Med. 2016;34:166–168. doi:10.1016/j.jocn.2016.06.012
107. Oliver JD, Goncalves S, Kerezoudis P, et al. Comparison of Outcomes for Anterior Cervical Discectomy and Fusion With and Without Anterior Plate Fixation: a Systematic Review and Meta-Analysis. Spine. 2018;43(7):E413–E22. doi:10.1097/BRS.0000000000002441
108. Purger DA, Pendharkar AV, Ho AL, et al. Outpatient vs Inpatient Anterior Cervical Discectomy and Fusion: a Population-Level Analysis of Outcomes and Cost. Neurosurgery. 2018;82(4):454–464. doi:10.1093/neuros/nyx215
109. Zhu Y, Zhang B, Liu H, et al. Cervical Disc Arthroplasty Versus Anterior Cervical Discectomy and Fusion for Incidence of Symptomatic Adjacent Segment Disease: a Meta-Analysis of Prospective Randomized Controlled Trials. Spine. 2016;41(19):1493–1502. doi:10.1097/BRS.0000000000001537
110. Liu Y, Wang H, Li X, et al. Comparison of a zero-profile anchored spacer (ROI-C) and the polyetheretherketone (PEEK) cages with an anterior plate in anterior cervical discectomy and fusion for multilevel cervical spondylotic myelopathy. Eur Spine J. 2016;25(6):1881–1890. doi:10.1007/s00586-016-4500-x
111. Fountas KN, Kapsalaki EZ, Nikolakakos LG, et al. Anterior cervical discectomy and fusion associated complications. Spine. 2007;32(21):2310–2317. doi:10.1097/BRS.0b013e318154c57e
112. Portnoy HD. Anterior cervical discectomy and fusion. Surg Neurol. 2001;56:178–180. doi:10.1016/S0090-3019(01)00554-7
113. Smith GW, Robinson RA. The treatment of certain cervical-spine disorders by anterior removal of the intervertebral disc and interbody fusion. J Bone Joint Surg Am. 1958;40-A:607–624.
114. Zhuang L, Wang L, Xu D, et al. Association between excessive smartphone use and cervical disc degeneration in young patients suffering from chronic neck pain. J Orthopaedic Sci. 2021;26:110–115. doi:10.1016/j.jos.2020.02.009
115. Fraser JF, Hartl R. Anterior approaches to fusion of the cervical spine: a metaanalysis of fusion rates. J Neurosurg Spine. 2007;6:298–303. doi:10.3171/spi.2007.6.4.2
116. Sugawara T. Anterior Cervical Spine Surgery for Degenerative Disease: a Review. Neurol Med Chir (Tokyo). 2015;55:540–546. doi:10.2176/nmc.ra.2014-0403
117. He J, Wu T, Ding C, et al. Bibliometric and visualized analysis of the top 100 most-cited articles on anterior cervical surgery. EFORT Open Rev. 2021;6:1203–1213. doi:10.1302/2058-5241.6.210074
118. Perez-Roman RJ, Luther EM, McCarthy D, et al. National Trends and Correlates of Dysphagia After Anterior Cervical Discectomy and Fusion Surgery. Neurospine. 2021;18:147–154. doi:10.14245/ns.2040452.226
119. Ostrov PB, Reddy AK, Ryoo JS, et al. Anterior Cervical Discectomy and Fusion Versus Cervical Disc Arthroplasty: a Comparison of National Trends and Outcomes. World Neurosurg. 2022;160:e96–e110. doi:10.1016/j.wneu.2021.12.099
120. Quadri SA, Capua J, Ramakrishnan V, et al. A rare case of pharyngeal perforation and expectoration of an entire anterior cervical fixation construct. J Neurosurg Spine. 2017;26:560–566. doi:10.3171/2016.10.SPINE16560
121. Hua W, Zhi J, Wang B, et al. Biomechanical evaluation of adjacent segment degeneration after one- or two-level anterior cervical discectomy and fusion versus cervical disc arthroplasty: a finite element analysis. Comput Methods Programs Biomed. 2020;189:105352. doi:10.1016/j.cmpb.2020.105352
122. Mummaneni PV, Burkus JK, Haid RW, et al. Clinical and radiographic analysis of cervical disc arthroplasty compared with allograft fusion: a randomized controlled clinical trial. J Neurosurg Spine. 2007;6:198–209. doi:10.3171/spi.2007.6.3.198
123. Fernstrom U. Arthroplasty with intercorporal endoprothesis in herniated disc and in painful disc. Acta Chir Scand Suppl. 1966;357:154–159.
124. Othman YA, Verma R, Qureshi SA. Artificial disc replacement in spine surgery. Ann Transl Med. 2019;7:S170. doi:10.21037/atm.2019.08.26
125. Shin JJ, Kim KR, Son DW, et al. Cervical disc arthroplasty: what we know in 2020 and a literature review. J Orthop Surg. 2021;29:23094990211006934. doi:10.1177/23094990211006934
126. Dmitriev AE, Cunningham BW, Hu N, et al. Adjacent level intradiscal pressure and segmental kinematics following a cervical total disc arthroplasty: an in vitro human cadaveric model. Spine. 2005;30:1165–1172. doi:10.1097/01.brs.0000162441.23824.95
127. Goz V, Martin BI, Donnally CJ 3rd, et al. Potential Selection Bias in Observational Studies Comparing Cervical Disc Arthroplasty to Anterior Cervical Discectomy and Fusion. Spine. 2020;45:960–967. doi:10.1097/BRS.0000000000003427
128. Joaquim AF, Lee NJ, Lehman RA, et al. Osteolysis after cervical disc arthroplasty. Eur Spine J. 2020;29:2723–2733. doi:10.1007/s00586-020-06578-2
129. Lu Y, McAnany SJ, Hecht AC, et al. Utilization trends of cervical artificial disc replacement after FDA approval compared with anterior cervical fusion: adoption of new technology. Spine. 2014;39:249–255. doi:10.1097/BRS.0000000000000113
130. Ahn Y. The Current State of Cervical Endoscopic Spine Surgery: an Updated Literature Review and Technical Considerations. Expert Rev Med Devices. 2020;17:1285–1292. doi:10.1080/17434440.2020.1853523
131. Wu TK, Liu H, Ning N, et al. Cervical disc arthroplasty for the treatment of adjacent segment disease: a systematic review of clinical evidence. Clin Neurol Neurosurg. 2017;162:1–11. doi:10.1016/j.clineuro.2017.08.019
132. Veruva SY, Steinbeck MJ, Toth J, et al. Which design and biomaterial factors affect clinical wear performance of total disc replacements? A systematic review. Clin Orthopaedics Related Res. 2014;472:3759–3769. doi:10.1007/s11999-014-3751-2
133. Werner JH, Rosenberg JH, Keeley KL, et al. Immunobiology of periprosthetic inflammation and pain following ultra-high-molecular-weight-polyethylene wear debris in the lumbar spine. Expert Rev Clin Immunol. 2018;14:695–706. doi:10.1080/1744666X.2018.1511428
134. Xie L, Chen Z, Wang H, et al. Bibliometric and Visualized Analysis of Scientific Publications on Atlantoaxial Spine Surgery Based on Web of Science and VOSviewer. World Neurosurg. 2020;137:435–42 e4. doi:10.1016/j.wneu.2020.01.171
135. Zhang Y, Wumaier M, He D, et al. The 100 top-cited articles on spinal deformity: a bibliometric analysis. Spine. 2020;45:275–283. doi:10.1097/BRS.0000000000003247
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

