Back to Journals » International Medical Case Reports Journal » Volume 10
A B-cell lymphoma case that is unclassifiable, and intermediate between diffuse large B-cell lymphoma and Burkitt lymphoma of lacrimal gland
Authors Yunoki T , Murakami J, Imagawa Y, Nakajima T, Hayashi A
Received 24 September 2016
Accepted for publication 3 December 2016
Published 1 February 2017 Volume 2017:10 Pages 31—33
DOI https://doi.org/10.2147/IMCRJ.S123128
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Tatsuya Yunoki,1 Jun Murakami,2 Yukihiro Imagawa,3 Takahiko Nakajima,4 Atsushi Hayashi1
1Department of Ophthalmology, 2Department of Gastroenterology, Graduate School of Medicine and Pharmaceutical Sciences, University of Toyama, Toyama, 3Department of Ophthalmology, Osaka Kaisei Hospital, Osaka, 4Department of Diagnostic Pathology, Graduate School of Medicine and Pharmaceutical Sciences, University of Toyama, Toyama, Japan
Abstract: A 60-year-old woman presented with acute eyelid swelling and a subcutaneous hemorrhage in the right eye. Magnetic resonance imaging showed a spherical tumor of the lacrimal gland. The tumor was removed by the Kroenlein method. We diagnosed as a B-cell lymphoma that is unclassifiable, and intermediate between diffuse large B-cell lymphoma (DLBCL) and Burkitt lymphoma (BL) (intermediate DLBCL/BL) based on its immunohistopathological examination and c-MYC/IgH rearrangement. We administered six cycles of dose-adjusted-EPOCH-R (etoposide, prednisone, vincristine, cyclophosphamide, doxorubicin hydrochloride, and rituximab) therapy, and remission of the lymphoma was obtained. This is the first case of an intermediate DLBCL/BL of a lacrimal gland.
Keywords: diffuse large B-cell lymphoma, Burkitt lymphoma, c-MYC gene, fluorescence in situ hybridization
Introduction
According to the 2008 World Health Organization Classification of Tumors of Haematopoietic and Lymphoid Tissues, the morphological and genetic features of diffuse large B-cell lymphoma (DLBCL) overlap with those of Burkitt lymphoma (BL).1 Intermediate DLBCL/BL, a B-cell non-Hodgkin lymphoma, is highly aggressive.2 It has a high malignancy grade, and as it is a very rare lymphoma subtype in adults, standard treatment has not yet been established. A previous study has reported that intermediate DLBCL/BL has poor outcomes, with a median overall survival of only 9 months and a 5-year overall survival rate of 30%.2 The rapid progression of an aggressive orbital lymphoma can cause optic nerve disorders and sometimes a life-threatening crisis. Thus, early diagnosis and appropriate treatment of this condition are crucial.3,4
In this case report, we describe a case of intermediate DLBCL/BL of the lacrimal gland that presented with subcutaneous hemorrhage and orbital hematoma. To the best of our knowledge, this is the first report of an intermediate DLBCL/BL of the lacrimal gland.
Case report
Patient characteristics and clinical examination
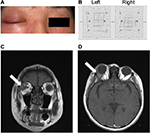
The patient was a 60-year-old Japanese woman who presented with acute eyelid swelling and a subcutaneous hemorrhage in the right eye. She has no history of acute eye trauma. At the time of the first medical examination, the best-corrected visual acuity of both eyes was 1.2, and no abnormality was detected on slit lamp microscopy and fundoscopy. It was difficult for the patient to open her right eye because of eyelid swelling and subcutaneous hemorrhage (Figure 1A). The Hess chart results indicated an ocular motility disorder (Figure 1B). Magnetic resonance imaging revealed a spherical tumor of the lacrimal gland (Figure 1C and D). There was no tumor involvement of the temporalis fossa or the skin of the eyelid. Furthermore, hemorrhage occurred within and around the tumor, probably owing to intratumoral bleeding. The patient did not have a history of autoimmune diseases such as Sjögren’s syndrome, which could underlie the development of malignant lymphoma. Written informed consent was obtained from the patient for publication of this case report and accompanying images.
Immunohistochemistry and gene profiling
Under general anesthesia, the patient underwent surgical removal of the tumor using the Kroenlein method, and we attempted to extract as much of the tumor mass as possible. Hematoxylin and eosin (H&E) staining of the tumor sample revealed a starry sky pattern, and immunohistochemical analysis revealed that the tissue was positive for leukocyte common antigen, CD20, CD10, and Bcl-6 staining; and negative for Bcl-2, CD3, and MUM1 staining, with a MiB1 labeling index of 90–95% (Figure 2). A fluorescence in situ hybridization (FISH) examination revealed reciprocal translocation (81.5%) of the c-MYC gene and the immunoglobulin gene (IgH), and IgH/Bcl-2 fusion and Bcl-6 split signal were negative. G-banding was not performed, but the t(8; 14) translocation was detected by FISH-based visualization of the c-MYC/IgH rearrangement. This rearrangement is very rare in cases of DLBCL.
Diagnosis and treatment
This case could have been diagnosed as BL on the basis of its immunoprofile and the c-MYC/IgH rearrangement. However, because the lymphoma was composed of proliferating cells with medium to large pleomorphic nucleoli, we defined it as an intermediate DLBCL/BL of the lacrimal gland according to the 2008 WHO Classification of Tumors of Haematopoietic and Lymphoid Tissues.1 Positron emission tomography/computed tomography images showed intense fluorine-18 deoxyglucose uptake in the porta hepatis, in addition to that in the orbit. We administered six cycles of dose-adjusted-EPOCH-R (etoposide, prednisone, vincristine, cyclophosphamide, doxorubicin hydrochloride, and rituximab) therapy, which resulted in remission of the lymphoma. We followed the patient’s progress carefully, and no visual function problems have been observed at 6 months after the completion of chemotherapy.
Discussion
In the current case, on the basis of the morphology of the lymphoma cells and the presence of c-MYC/IgH rearrangement by FISH, we concluded that this was not a case of either BL or DLBCL, but a case of intermediate DLBCL/BL in an otherwise healthy adult Japanese woman.
It is very rare for an orbital lymphoma that is an intermediate DLBCL/BL and a subcutaneous and orbital hematoma to present clinically with rapid eyelid swelling. Clinicians must consider the possibility of an orbital intermediate DLBCL/BL when these symptoms are observed. Early treatment and appropriate management are crucial to maintain the patient’s visual function and to improve the likelihood of survival. The rapid progression of an aggressive orbital lymphoma results in various clinical symptoms such as painful proptosis and vision loss.3 If an orbital lymphoma, such as BL and intermediate DLBCL/BL, is suspected, the diagnosis must be confirmed as soon as possible by using methods such as tissue biopsy.
Acknowledgment
This study was supported in part by a Grant-in-Aid for Young Scientists (B) (16K20309) from the Japan Society for the Promotion of Science.
Disclosure
The authors report no conflicts of interest in this work.
References
Kluin PM, Harris NL, Stein H, et al. B-cell lymphoma, unclassifiable, with features intermediate between diffuse large B-cell lymphoma and Burkitt lymphoma. In: WHO Classification of Tumors of Haematopoietic and Lymphoid Tissues. Lyon, IARC Press; 2008:265–266. | ||
Perry AM, Crockett D, Dave BJ et al. B-cell lymphoma, unclassifiable, with features intermediate between diffuse large B-cell lymphoma and Burkitt lymphoma: study of 39 cases. Br J Haematol. 2013;162(1):40–49. | ||
Alexander C, George C, Tinatin J, Maia S, Maia M, Mitrofanis P. Orbital Burkitt lymphoma: a case presentation. BMC Ophthalmol. 2014;14:109. | ||
Giuliari GP, Sadaka A, Cortez MA, Paniagua A. Orbital Burkitt’s lymphoma: an aggressive presentation. Case Rep Ophthalmol Med. 2012;2012:354043. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.