Back to Journals » Neuropsychiatric Disease and Treatment » Volume 12
5-HTR1A and 5-HTR2A genetic polymorphisms and SSRI antidepressant response in depressive Chinese patients
Authors Dong Z, Li X, He L, He G, Yu T, Sun X
Received 1 August 2015
Accepted for publication 5 February 2016
Published 4 July 2016 Volume 2016:12 Pages 1623—1629
DOI https://doi.org/10.2147/NDT.S93562
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Wai Kwong Tang
Zai-Quan Dong,1,* Xi-Rong Li,2,* Lin He,3,4 Guang He,3,4 Tao Yu,3,4 Xue-Li Sun1
1Psychological Center, West China Hospital, Sichuan University, Chengdu, Sichuan, 2Mental Health Center, First Affiliated Hospital, Chongqing Medical University, Chongqing, 3Bio-X Institutes, Key Laboratory for the Genetics of Developmental and Neuropsychiatric Disorders (Ministry of Education), Shanghai Jiao Tong University, 4Shanghai Key Laboratory of Psychotic Disorders, Shanghai Mental Health Center, Shanghai Jiao Tong University School of Medicine, Shanghai, People’s Republic of China
*These authors contributed equally to this work
Objective: Genetic variabilities within the serotoninergic system may predict response or remission to antidepressant drugs. Several serotonin receptor (5-HTR) gene polymorphisms have been associated with susceptibility to psychiatric diseases. In this study, we analyzed the correlation between 5-HTR1A and 5-HTR2A polymorphisms and response or remission to selective serotonin reuptake inhibitors (SSRIs) drugs.
Methods: Two hundred and ninety patients who met the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition criteria for major depressive disorder were involved in this study. SSRIs (fluoxetine, paroxetine, citalopram, or sertraline) were selected randomly for treatment. The Hamilton Rating Scale for Depression was used to evaluate the antidepressant effect. To assess 5-HTR gene variabilities, two single-nucleotide polymorphisms in 5-HTR1A (rs1364043 and rs10042486) and three in 5-HTR2A (rs6311, rs6313, and rs17289304) were genotyped by matrix-assisted laser desorption/ionization time-of-flight mass spectrometry using the Sequenom MassARRAY Analyzer 4 system.
Results: There were 220 responders and 70 nonresponders (120 remissioners and 170 nonremissioners) after 6 weeks of treatment. We found no association between any of the five 5-HTR1A and 5-HTR2A gene polymorphisms and antidepressant drug response or remission (P>0.05). It is worth mentioning that TT genotype frequency of rs10042486 was significantly different from the CT genotype frequency between responders and nonresponders, although the significance was not maintained after correcting for multiple testing.
Conclusion: Thus, 5-HTR1A and 5-HTR2A gene polymorphisms may not play an important role in antidepressant drug response or remission.
Keywords: genetic association, major depressive disorder, SSRIs
Introduction
Major depressive disorder (MDD) has a significant impact on social health, bringing considerable direct and indirect costs to society. Many pharmacological antidepressant treatments with proven efficacy have been available for years; yet, not all depressed patients benefit from specific efficacious antidepressants. Even with optimal quality-controlled conditions, only about two-thirds of patients show symptomatic improvement in the first round of treatment, while only 50% show full remission (no or only minimal residual symptoms) within 12 weeks; also, for two-thirds of patients, up to four treatment trials are needed to achieve full remission.1 Response and remission to medication is highly variable, and there are several potential explanations for the variability of drug-response rates, including symptom heterogeneity, environmental, social, and genetic factors.
Pharmacogenetic studies provide the opportunity for identifying robust predictors of individual responses to antidepressants, potentially allowing personalized treatment for a given patient.
Candidate genes for pharmacogenetic studies include those involved in drug metabolism (eg, tryptophan hydroxylase 1 and cytochrome P450), drug targets (eg, serotonin transporter and serotonin 2A receptor), and potential disease mechanisms (eg, FK506 binding protein 5 and brain-derived neurotrophic factor).
Plenty of evidence suggests that both serotonin 1A and 2A receptors (5-HTR1A and 5-HTR2A, respectively) play an important role in the etiology of depression and clinical effects of antidepressants. Significantly impaired 5-HTR1A function has been reported to increase the risk of major depression,2 while animal model showed increased regional 5-HTR1A receptor expression after chronic electroconvulsive shock.3 Furthermore, in postmortem studies from depressed patients, those who underwent long-term antidepressant treatment showed increased serotonergic neurotransmission mediated by 5-HTR1A.4 In humans, the role of 5-HTR1A in the antidepressant response is now well established.5 Similarly, 5-HTR2A antagonists are effective antidepressants in humans.6 In animal models of depression, 5-HTR2A may also mediate some antidepressant effects.7
In this study, we examined the involvement of 5-HTR2A (rs17289304, rs6311, and rs6313) and 5-HTR1A (rs10042486 and rs1364043) genes in the antidepressant effect of selective serotonin reuptake inhibitors (SSRIs). All the single-nucleotide polymorphisms (SNPs) we selected were reported to be associated with antidepressant response in published papers including genome-wide association studies.8–10 Most of them were tagSNPs from the HapMap and functional SNPs in the regulatory regions. Ultimately, the study of personalized medicine may lead to the use of genetic testing for guiding antidepressant use in clinical practice.
Methods
Subjects
A total of 290 depressed patients (18–55 years old) fulfilling the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition criteria for MDD and with a minimum Hamilton Depression Rating Scale (HAMD) score of 18 were recruited from April 2005 to September 2006. Diagnosis was confirmed by psychiatric examination performed by board-certified and experienced psychiatrists. Patients were new cases or had not taken any antidepressant treatment at least 2 weeks before recruitment and with no history of electroconvulsive therapy. Patients with other axis I psychiatric disorders (including schizophrenia, rapid cycling bipolar disorder, dementia, generalized anxiety disorder, obsessive–compulsive disorder, and substance abuse), axis II disorders (including personality disorders), major medical/neurological disorders, abnormal laboratory baseline values, and pregnancy were excluded.
All participants were of unrelated Chinese Han origin, and shared similar geographic and sociodemographic data. The Institutional Ethics Committee of Sichuan University approved this study and written informed consent was obtained from each participant.
Treatment
All patients received treatment for a 6-week period with SSRIs. Among the participants, 59.31% (172 out of the 290) were new cases for antidepressant treatment. Patients were randomly selected for treatment with fluoxetine, paroxetine, citalopram, or sertraline (paroxetine 20–40 mg once a day [qd], fluoxetine 10–40 mg qd, citalopram 20–40 mg qd, or sertraline 50–150 mg qd). Other psychotropic medications were not permitted during the study, except for benzodiazepine prescribed occasionally with a minimum dosage at bedtime for insomnia.
Data collection
On study enrollment, 5 mL of peripheral venous blood was collected from each participant for genotyping. Patients’ conditions were assessed by trained psychiatrists blinded to genotypes and who were responsible for providing a detailed objective protocol for each patient. A 17-item HAMD was used to evaluate treatment efficacy at baseline and 1, 2, 4, and 6 weeks following treatment initiation. Clinical response was defined as >50% decrease in total HAMD score on treatment completion, and clinical remission as a final HAMD score <8.11
In total, eleven patients were excluded due to absent blood samples or genotyping failure. Another three patients did not complete the study due to intolerable adverse effects. Overall, a cohort of 290 patients was included in the final analysis.
DNA extraction and genotyping
Genomic DNA was extracted from venous blood leukocytes using standard phenol–chloroform method. Considering potential function and frequency, five SNPs in 5-HTR genes were selected from Single Nucleotide Polymorphism Database (http://www.ncbi.nlm.nih.gov) or previous literature. Of these five SNPs, rs1364043 and rs10042486 are located downstream and upstream, respectively, of 5-HTR1A, rs17289304 and rs6311 lie upstream of 5-HTR2A, and rs6313 is in the 3′ untranslated region of 5-HTR2A. Genotyping of all SNPs was performed by matrix-assisted laser desorption/ionization time-of-flight mass spectrometer using MassARRAY® Analyzer 4 platform (Sequenom, San Diego, CA, USA). All primers were designed by the accompanying software Spectrodesigner. The polymerase chain reactions (PCRs) were carried out in a total volume of 5 μL, with 10 ng genomic DNA using the cycling conditions recommended by the manufacturer. Multiplexing and homogeneous mass-extension processes were used to produce primer extension products. Detailed information on the primers and polymerase chain reaction conditions are available on request. Genotype determination was performed by researchers blinded to the clinical outcomes of antidepressant treatment.
Statistical analysis
Hardy–Weinberg equilibrium was calculated using χ2 tests, and linkage disequilibrium (LD) analysis was performed using SHEsis software (Shanghai Jiao Tong University, Shanghai, People’s Republic of China).12 LD of all pairs of SNPs within each gene was estimated with D′ as the standardized measurement. Haplotype construction was initially performed on HaploView (Broad Institute of MIT and Harvard, USA) and further analysis was carried out on SHEsis. Comparisons of genotype/allele and haplotype frequencies between responders and nonresponders, and remissioners and nonremissioners were performed for each polymorphism using χ2 or Fisher’s tests. P-values were corrected for allelic and genotype association analysis using Bonferroni correction. Probability of a type I error was set at a maximum level of 0.05. All analyses were performed using SPSS Version 17.0 (SPSS Inc., Chicago, IL, USA).
Results
Characteristics of study subjects
The clinical and demographic characteristics of the 290 patients (220 responders and 70 nonresponders, and 120 remissioners and 170 nonremissioners) included in this study are summarized in Table 1. There were no significant differences in HAMD-17 baseline, age, sex, marriage status, family history, and body mass index between responders and nonresponders or between remissioners and nonremissioners.
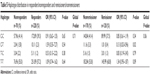
5-HTR genotype and allele frequencies
Genotype distributions in the total cohort were in Hardy–Weinberg equilibrium (Table 2). Genotype and allele frequencies of the five SNPs (rs6311, rs6313, rs1364043, rs10042486, and rs17289304) are summarized in Table 3. For rs10042486, there was a significant difference in genotype frequency between responders and nonresponders (P=0.012), although the difference was no longer significant after correcting for multiple testing. Allele frequencies of rs10042486 in responders were not significantly different from nonresponders (P>0.05). Genotype and allele frequencies of the other polymorphisms in responders or remissioners were not significantly different from those in nonresponders or nonremissioners (P>0.05).
  | Table 2 Hardy–Weinberg equilibrium analysis |
Pairwise LD among the five markers is presented in Table 4. Haplotype analysis was performed and the estimated haplotype frequencies are summarized in Table 5. Haplotypes were rejected if the estimated haplotype frequencies were <3% in both groups. The results showed that rs6311 and rs6313 polymorphisms displayed LD (D′=0.94) in subjects. However, no haplotype was associated with antidepressant response or remission.
  | Table 5 Haplotype distribution in responders/nonresponders and remissioners/nonremissioners |
Discussion
SSRIs are a widely prescribed medication and currently one of the preferred treatments for major depression.13,14 However, not all patients benefit from use of these drugs. Many studies have shown that ~40% of patients respond partially, or not at all, to antidepressants.15,16 In this study, we found a 76% response rate and 42% remission rate at 6 weeks of treatment with SSRIs, similar to previous studies.17
Reduced expression of 5-HTR gene is considered a hypothetical risk factor that may explain some of the differences in clinical response to drugs targeting this receptor. In the present study, we found no correlation between rs10042486 in 5-HTR1A and treatment response to SSRIs in patients with MDD. Many other studies in this field have reported inconsistent results. In Kato et al’s18 study, an association between rs10042486 and treatment response in Japanese subjects with major depression was found. The same association was also observed in schizophrenia, as Crisafulli et al19 reported that rs10042486 was associated with schizophrenia and clinical improvement on Positive and Negative Syndrome Scale total scores as well as Positive and Negative Syndrome Scale positive and negative scores. However, Zhao et al20 reported the opposite conclusion in a Chinese cohort, and Villafuerte et al21 also found no association between rs10042486 and response to citalopram in the Sequenced Treatment Alternatives to Relieve Depression (STAR*D) study.
Little attention has been paid to rs1364043. We did not find any association between rs1364043 and either SSRI treatment response or remission. However, in the STAR*D study, Villafuerte et al21 reported that individuals homozygous for the G allele of rs1364043, and a haplotype containing this allele, showed a better response over time to citalopram. Kato et al’s study also observed significant association between improved response to antidepressants and rs1364043 T/T genotype carriers in 137 Japanese major depression subjects.18
Genetic variation in 5-HTR2A has been widely implicated in a variety of neuropsychiatric disorders,22 although it has not been convincingly demonstrated that it affects antidepressant treatment outcome. Our study did not find any association between 5-HTR2A (rs17289304, rs6311, and rs6313) and treatment outcome. Linkage analysis identified LD between rs6311 and rs6313, but the haplotype was not associated with treatment outcome. This is consistent with another Chinese study conducted by Li et al.23 Similarly, Andre et al24 found no significant interaction between 5-HT2A gene SNPs (rs6311, rs6313, and rs7997012) and SSRI treatment response. The STAR*D research by McMahon et al25 also found that neither rs6311 nor rs6313 showed significant association with treatment response or remission. Viikki et al26 reported that either rs7997012 or rs6311 within 5-HTR2A was not significantly associated with Montgomery–Asberg Depression Scale score change, but interaction between the SNPs and sex could explain 14% of the variance in Montgomery–Asberg Depression Scale score change, prompting the suggestion that rs6311 may not independently influence treatment outcome, but play a role by interacting with other factors. However, the association between rs6311 in 5-HT2A receptor and response to SSRIs has been reported in Asian and Caucasian people.8,27,28 Many factors may contribute to these inconsistent results in the same candidate gene (eg, sample size, definition of response or remission, and antidepressant choice). In our study, only SSRIs were used, in order to minimize the influence of drug variety. In addition, many of these studies were performed on a small sample size within a short-term follow-up period, which may cause possible false-negative or -positive results. Ethnic differences may also play an important role in generating inconsistent results. For example, Drago et al29 reviewed studies focusing on rs10042486 polymorphism in 5-HTR1A gene and found that the allele prevalence in different populations showed extreme variations (eg, C=0.517 in Caucasian, 0.133 in Han Chinese, 0.125 in Japanese, and 0.271 in sub-Saharan African).
There are several limitations in our study. We did not measure plasma levels of the medications, although these effects are probably minor as there is no identified correlation between plasma SSRI concentration and clinical response.30,31 Other limitations include small sample size and short follow-up periods. Moreover, as we did not use a control group, a placebo effect may reinforce the study limitations.
In conclusion, we found no association between 5-HTR1A and 5-HTR2A polymorphisms and SSRI therapeutic response in Chinese Han MDD patients. However, in view of the importance of 5-HTR in the mechanism of SSRIs’ antidepressant action, further studies with large sample size should be performed to explore the association between SNPs in 5-HTR genes and antidepressant effects.
Acknowledgments
We appreciate the contribution of the participants in this study, as well as that of the psychiatrists who helped with diagnosis. This work was supported by the 973 Program (2010CB529600), the Shanghai Key Laboratory of Psychotic Disorders (13dz2260500).
Disclosure
The authors report no conflicts of interest in this work.
References
Trivedi MH, Daly EJ. Measurement-based care for refractory depression: a clinical decision support model for clinical research and practice. Drug Alcohol Depend. 2007;88(Suppl 2):S61–S71. | ||
Lemonde S, Turecki G, Bakish D, et al. Impaired repression at a 5-hydroxytryptamine 1A receptor gene polymorphism associated with major depression and suicide. J Neurosci. 2003;23(25):8788–8799. | ||
Gur E, Dremencov E, Garcia F, Van de Kar LD, Lerer B, Newman ME. Functional effects of chronic electroconvulsive shock on serotonergic 5-HT (1A) and 5-HT(1B) receptor activity in rat hippocampus and hypothalamus. Brain Res. 2002;952(1):52–60. | ||
Blier P, de Montigny C. Current advances and trends in the treatment of depression. Trends Pharmacol Sci. 1994;15(7):220–226. | ||
Cryan JF, Leonard BE. 5-HT1A and beyond: the role of serotonin and its receptors in depression and the antidepressant response. Hum Psychopharmacol. 2000;15(2):113–135. | ||
Leysen JE. 5-HT2 receptors. Curr Drug Targets CNS Neurol Disord. 2004;3(1):11–26. | ||
Skrebuhhova T, Allikmets L, Matto V. Effects of anxiogenic drugs in rat forced swimming test. Methods Find Exp Clin Pharmacol. 1999;21(3):173–178. | ||
Kato M, Fukuda T, Wakeno M, et al. Effects of the serotonin type 2A, 3A and 3B receptor and the serotonin transporter genes on paroxetine and fluvoxamine efficacy and adverse drug reactions in depressed Japanese patients. Neuropsychobiology. 2006;53(4):186–195. | ||
Kato M, Fukuda T, Wakeno M, et al. 5-HT1A gene polymorphisms contributed to antidepressant response in major depression. Nihon Shinkei Seishin Yakurigaku Zasshi. 2009;29(1):23–31. | ||
Lin JY, Jiang MY, Kan ZM, Chu Y. Influence of 5-HTR2A genetic polymorphisms on the efficacy of antidepressants in the treatment of major depressive disorder: a meta-analysis. J Affect Disord. 2014;168:430–438. | ||
Keller MB. Past, present, and future directions for defining optimal treatment outcome in depression. JAMA. 2003;289(23):3152–3160. | ||
Shi YY, He L. SHEsis, a powerful software platform for analyses of linkage disequilibrium, haplotype construction, and genetic association at polymorphism loci. Cell Res. 2005;15(2):97–98. | ||
Stahl SM. Mechanism of action of serotonin selective reuptake inhibitors. Serotonin receptors and pathways mediate therapeutic effects and side effects. J Affect Disord. 1998;51(3):215–235. | ||
Neal DJ. SSRIs: where now, where next? In: Stanford SC, editor. Selective Serotonin Reuptake Inhibitors (SSRIs) Past, Present and Future. Georgetown: Landres Company; 1999:187–218. | ||
Spigset O, Mårtensson B. Fortnightly review: drug treatment of depression. BMJ. 1999;318(7192):1188–1191. | ||
Quitkin FM, Rabkin JG, Gerald J, Davis JM, Klein DF. Validity of clinical trials of antidepressants. Am J Psychiatry. 2000;157(3):327–337. | ||
Thase ME, Haight BR, Richard N, et al. Remission rates following antidepressant therapy with bupropion or selective serotonin reuptake inhibitors: a meta-analysis of original data from 7 randomized controlled trials. J Clin Psychiatry. 2005;66(8):974–981. | ||
Kato M, Fukuda T, Wakeno M, et al. Effect of 5-HT1A gene polymorphisms on antidepressant response in major depressive disorder. Am J Med Genet B Neuropsychiatr Genet. 2009;150B(1):115–123. | ||
Crisafulli C, Chiesa A, Han C, et al. Case-control association study for 10 genes in patients with schizophrenia: influence of 5HTR1A variation rs10042486 on schizophrenia and response to antipsychotics. Eur Arch Psychiatry Clin Neurosci. 2012;262(3):199–205. | ||
Zhao X, Jin Q, Wu L, Huang Y, Li J, Zhu G. Sertraline (Zoloft) response in major depressive disorder is not associated with three 5-HT1A receptor gene polymorphisms (rs6295, rs10042486, or rs1364043) in Chinese-Han patients. Psychiatr Genet. 2012;22(5):261–262. | ||
Villafuerte SM, Vallabhaneni K, Sliwerska E, McMahon FJ, Young EA, Burmeister M. SSRI response in depression may be influenced by SNPs in HTR1B and HTR1A. Psychiatr Genet. 2009;19(6):281–291. | ||
Norton N, Owen MJ. HTR2A: association and expression studies in neuropsychiatric genetics. Ann Med. 2005;37(2):121–129. | ||
Li HF, Yu X, Yang K, et al. The relationship between single nucleotide polymorphisms in 5-HT2A signal transduction-related genes and the response efficacy to selective serotonin reuptake inhibitor treatments in Chinese patients with major depressive disorder. Genet Test Mol Biomarkers. 2012;16(7):667–671. | ||
Andre K, Kampman O, Setälä-Soikkeli E, et al. Temperament profiles, 5-HT2A genotype, and response to treatment with SSRIs in major depression. J Neural Transm. 2010;117(12):1431–1434. | ||
McMahon FJ, Buervenich S, Charney D, et al. Variation in the gene encoding the serotonin 2A receptor is associated with outcome of antidepressant treatment. Am J Hum Genet. 2006;78(5):804–814. | ||
Viikki M, Huuhka K, Leinonen E, et al. Interaction between two HTR2A polymorphisms and gender is associated with treatment response in MDD. Neurosci Lett. 2011;501(5):20–24. | ||
Choi MJ, Kang RH, Ham BJ, Jeong HY, Lee MS. Serotonin receptor 2A gene polymorphism(-143A/G) and short-term treatment response to citalopram. Neuropsychobiology. 2005;52(3):155–162. | ||
Kishi T, Yoshimura R, Kitajima T, et al. HTR2A is associated with SSRI response in major depressive disorder in a Japanese cohort. Neuromolecular Med. 2010;12(3):237–242. | ||
Drago A, Ronchi DD, Serretti A. 5-HT1A gene variants and psychiatric disorders: a review of current literature and selection of SNPs for future studies. Int J Neuropsychopharmacol. 2007;11(5):701–721. | ||
Kasper S, Dötsch M, Kick H, Vieira A, Möller HJ. Plasma concentrations of fluvoxamine and maprotiline in major depression: Implications on therapeutic efficacy and side effects. Eur Neuropsychopharmacol. 1993;3(1):13–21. | ||
Saito S, Takahashi N, Ishihara R, et al. Association study between vesicle-associated membrane protein 2 gene polymorphisms and fluvoxamine response in Japanese major depressive patients. Neuropsychobiology. 2006;54(4):226–230. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



