Back to Journals » International Journal of General Medicine » Volume 13
18F-FDG PET–CT Diagnosis of Tuberculosis in Celiac Lymph Nodes
Authors Mao XB, Li N , Huang ZS, Ding CM, Bao WJ, Fan J, Li HL
Received 19 October 2020
Accepted for publication 12 November 2020
Published 2 December 2020 Volume 2020:13 Pages 1335—1339
DOI https://doi.org/10.2147/IJGM.S287115
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Xi Bao Mao, Nan Li, Zao Sheng Huang, Chen Min Ding, Wen Jun Bao, Jing Fan, Hai Long Li
Department of Nuclear Medicine, Changzhou Cancer Hospital, Soochow University, Changzhou 213032, People’s Republic of China
Correspondence: Xi Bao Mao
Department of Nuclear Medicine, Changzhou Cancer Hospital, Soochow University, Changzhou 213032, People’s Republic of China
Tel +86-139-6112-5162
Email [email protected]
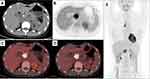
Abstract: The special location of abdominal tuberculosis makes it difficult for biopsy, while its clinical and imaging characteristics make it indistinguishable from tumors. Here, we report a female patient that was initially misdiagnosed with pancreatic cancer, but eventually correctly diagnosed with tuberculosis in the celiac lymph nodes using 18F-FDG PET–CT. She was 38 years old. Her main complaint was “deep abdominal pain and discomfort for nearly a month”, accompanied by nausea and vomiting. Diagnosis of pancreatic tumors or enlarged lymph nodes was initially made based on CT scan results. Abdominal MRI revealed enlarged lymph nodes. 18F-FDG PET–CT imaging revealed a soft-tissue mass about 2.8 cm in diameter in the hepatic hilar area with a maximum standardized uptake value (SUVmax) of 9.4, and delayed imaging measured the SUVmax at 12. Enhanced CT showed no vascular envelopment in the mass. Based on these results, the patient was diagnosed with tuberculosis in the celiac lymph nodes. Her tuberculin test was strongly positive. After 5 months of antituberculosis treatment, the mass had reduced to about 1.5 cm in diameter and SUVmax reduced to 8.1, as demonstrated by 18F-FDG PET–CT imaging. Abdominal lymph-node tuberculosis is easy to misdiagnose, but timely 18F-FDG PET–CT imaging combined with tuberculin testing may reduce misdiagnosis and mistreatment.
Keywords: 18F-FDG PET/CT imaging, lymph-node tuberculosis, differential diagnosis
Introduction
Tuberculosis is one of the ten-leading causes of death and the main cause of death caused by a single source of infection (Mycobacterium tuberculosis),1 so its early and accurate diagnosis and treatment are very important. Early diagnosis of abdominal tuberculosis’ is relatively difficult, because of the difficulty in performing biopsy, due to its special location and the difficulty to distinguish from tumors. 18F-FDG PET–CT imaging can provide a more reliable clinical basis for diagnosis by simultaneously obtaining information on the anatomy and functional metabolism of the lesion and revealing multiple lesions throughout the body.2–4 Yamamoto et al reported that tuberculin testing combined with 18F-FDG PET–CT tumor imaging may be used for the diagnosis of tuberculous peritonitis.5
Lymph-node tuberculosis does not necessarily show increased uptake of FDG. Only active tuberculosis contains a large number of cells with strong glucose metabolism, which thus show significantly increased FDG uptake. The central necrotic area usually has defective FDG distribution, which leads to similar initial and delayed imaging results as malignant tumors. This indicates that the activity of tuberculosis lesions is related to FDG uptake, which may make it difficult to distinguish lymph-node tuberculosis from malignant tumors and sarcoidosis by 18F-FDG PET–CT imaging.6 We report here a female patient that was initially misdiagnosed with pancreatic cancer, but was eventually correctly diagnosed with abdominal lymph-node tuberculosis using 18F-FDG PET–CT imaging along with tuberculin testing. The lesion had significantly reduced after 5 months of antituberculosis treatment.
Case Presentation
The patient was a 38-year-old woman. Her main complaint was “deep abdominal pain and discomfort for nearly a month”, accompanied by nausea and vomiting. After anti-infection treatment, abdominal CT revealed space-occupying lesions on the anterior edge of the inferior vena cava, which were diagnosed as a pancreatic tumor or enlarged lymph node. Ten days later, abdominal MRI showed abnormal signals at the hepatic hilum and near the celiac trunk, which led to the diagnosis of enlarged lymph nodes. The overall initial diagnosis was proposed as “pancreatic space-occupying lesions”.
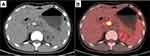
The patient’s clinical signs, blood routine, biochemical examinations, and duodenoscopy were all normal, and no abnormalities were observed in serum tumor markers AFP, CEA, CYFRA21-1, SCC, NSE, HE4, CA125, CA19-9, CA15-3, CA50, CA242, or CA72-4. Since the patient refused a biopsy of the tumor, 18F-FDG PET–CT was performed in order to understand the nature of the tumor and the condition of the systemic lymph nodes. As shown on 18F-FDG PET–CT (Figure 1), a soft-tissue mass about 2.8 cm in diameter was present in the hilar area, with punctate high-density shadows, unclear borders, and abnormal concentration of imaging agent. The maximum standardized uptake value (SUVmax) was 9.4 on initial imaging, but had became 12 2 hours later ony delayed imaging. Enhanced CT (Figure 2) revealed no vascular envelopment in the mass. Based on these results, the patient was diagnosed with tuberculosis of celiac lymph nodes. This diagnosis was confirmed by the strong positive result from the tuberculin test. Five months after antituberculosis treatment, the patient’s clinical symptoms had disappeared. Follow-up checking using 18F-FDG PET–CT imaging (Figure 3) showed that the mass had become smaller with a diameter of about 1.5 cm, along with increased internal punctate high-density shadow and SUVmax reduced to 8.1. These follow-up findings demonstrated effective antituberculosis treatment and led to continued treatment for the patient.
Discussion
Although laboratory tests indicated that this patient was infected with tuberculosis, clinical manifestations of tuberculosis-related symptoms were not typical, which led to the initial diagnosis of pancreatic tumor. 18F-FDG PET–CT imaging demonstrated high radiometabolic activity of the lesion. Combined with enhanced CT, no tumor vascular envelopment or invasion were observed. These results indicated a nontumor imaging sign and led to the diagnosis of celiac lymph-node tuberculosis. Further tuberculin testing showed strong positive reactivity, further confirming the diagnosis. This diagnosis method avoids invasive biopsy or laparotomy, and as a result reduces both the pain of patients and the risk of spreading of tuberculosis.
The combination of 18F-FDG PET–CT imaging and tuberculin testing alone is insufficient for diagnosis when lymph-node tuberculosis is in the inactive stage. It must be accompanied by contrast-enhanced ultrasound, ultrasound-guided needle biopsy, laparotomy, or laparoscopy.7–9 It has also been reported that PET–CT imaging using other positron-labeling agents labeled with 68Ga may detect more lesions than 18F-FDG PET–CT imaging, due to the former’s lower background uptake.10
18F-FDG PET–CT imaging is of great value in evaluating the state of tuberculosis, especially in evaluating the efficacy of midterm treatment,11,12 and in the diagnosis of recurrence of tuberculosis after treatment.13 Follow-up examination at 5 months using 18F-FDG PET–CT imaging revealed that the lesion had significantly reduced in size, with decreased intake of imaging agent, demonstrating effective antituberculosis treatment. At present, the patient is still undergoing antituberculosis treatment. As she refused to have biopsies taken during the whole process, the method described by Sánchez-Montalvá et al14 was used to observe lesion size and glucose metabolism with 18F-FDG PET–CT to further confirm the clinical diagnosis and evaluate the efficacy of treatment.
Conclusion
For abdominal lymph-node tuberculosis with atypical clinical symptoms, 18F-FDG PET–CT imaging combined with tuberculin testing can provide a basis for clinical diagnosis, curative effect evaluation, and recurrence evaluation, and reduce both misdiagnosis and missed diagnosis, when puncture biopsy is not an option.
Abbreviations
18F-FDG, 18F-fluorodeoxyglucose; PET, positron emission tomography; CT, computed tomography; MRI, magnetic resonance imaging; SUVmax, maximum standardized uptake value; AFP, α-fetoprotein; CEA, carcinoma embryonic antigen; CYFRA21-1, cytokeratin 19 fragment; SCC, squamous-cell carcinoma; NSE, neuron-specific enolase; CA, cancer antigen.
Data-Sharing Statement
The data sets used and/or analyzed during this study can be obtained from Xi Bao Mao (email [email protected]) as reasonably required.
Ethics and Consent
The study was approved by the ethics committees of Changzhou Cancer Hospital, Soochow University. Information revealing the subject’s identity was avoided. Written and signed informed consent was obtained from the patient to publish the case.
Funding
There is no funding to report.
Disclosure
The authors report no conflicts of interest for this work.
References
1. World Health Organization. Global tuberculosis report 2019. France: WHO/CDS/TB; 2019.
2. Hu YJ, Zhao XM, Zhang JY, Han J, Dai M. Value of 18F-FDG PET/CT radiomic features to distinguish solitary lung adenocarcinoma from tuberculosis. Eur J Nucl Med Mol Imaging. 2020. doi:10.1007/s00259-020-04924-6
3. Wang Q, Chen E, Cai Y, Zhang X, Li Q, Zhang X. A case report: systemic lymph node tuberculosis mimicking lymphoma on 18F-FDG PET/CT. Medicine (Baltim). 2016;95(9):e2912. doi:10.1097/MD.0000000000002912
4. Jin XN, Huo L, Wang T, Liu Y, Li F. Hepatosplenic tuberculosis on pretherapy and posttherapy FDG PET/CT. Clin Nucl Med. 2020;45(2):174–176. doi:10.1097/RLU.0000000000002858
5. Yamamoto S, Nishida T, Tsutsui S, et al. 18F-fluorodeoxyglucose-positron emission tomography (FDG-PET) was useful tool for detecting tuberculous peritonitis: report of a case. Nihon Shokakibyo Gakkai Zasshi. 2008;105(10):1515–1522.
6. Treglia G, Annunziata S, Sobic-Saranovic D, Bertagna F, Caldarella C, Giovanella L. The role of 18F-FDG-PET and PET/CT in patients with sarcoidosis: an updated evidence-based review. Acad Radiol. 2014;21(5):675–684. doi:10.1016/j.acra.2014.01.008
7. Cao BS, Wang FH, Liu L, et al. Abdominal tuberculous lymphadenopathy: contrast-enhanced ultrasonography imaging appearance with pathologic correlation. J Clin Ultra Med. 2015;17(12):820–822.
8. Yang YN, Liu J, Zhu HH. Analysis of misdiagnosed cases of pancreatic and peripancreatic lymph nodes tuberculosis. Clin Misdiagn Misther. 2016;29(6):1–3.
9. He XD, Liu Q. A case report of peritoneal tuberculosis diagnosed by laparoscopy and review of the literature. Yiyao Qianyan. 2017;7(30):208–209.
10. Hao B, Wu XR, Pan YZ, et al. 18F-FDG and 68Ga-DOTA-FAPI-04 PET/CT in the evaluation of tuberculous lesions. Eur J Nucl Med Mol Imaging. 2020. doi:10.1007/s00259-020-04941-5
11. Shimizu Y, Hashizume Y. PET/CT for monitoring the therapeutic response in a patient with abdominal lymph node tuberculosis after colon cancer resection. Kekkaku. 2012;87(11):707–712.
12. Sood A, Mittal BR, Modi M, et al. 18F-FDG PET/CT in tuberculosis: can interim PET/CT predict the clinical outcome of the patients? Clin Nucl Med. 2020;45(4):276–282. doi:10.1097/RLU.0000000000002968
13. Lawal IO, Fourie BP, Mathebula M, et al. 18F-FDG PET/CT as a noninvasive biomarker for assessing adequacy of treatment and predicting relapse in patients treated for pulmonary tuberculosis. J Nucl Med. 2020;61(3):412–417. doi:10.2967/jnumed.119.233783
14. Sánchez-Montalvá A, Barios M, Salvador F, et al. Usefulness of FDG PET/CT in the management of tuberculosis. PLoS One. 2019;14(8):e0221516. doi:10.1371/journal.pone.0221516
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.