Back to Journals » Clinical Epidemiology » Volume 7
Use of palivizumab is underestimated in the Swedish Prescribed Drug Register – implications for register-based drug studies
Authors Linder M , Byström C, Kieler H, Bergman G, Haerskjold A
Received 27 August 2014
Accepted for publication 3 October 2014
Published 29 December 2014 Volume 2015:7 Pages 45—51
DOI https://doi.org/10.2147/CLEP.S73337
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 5
Editor who approved publication: Professor Henrik Sørensen
Marie Linder,1 Camilla Byström,1 Helle Kieler,1 Gunnar Bergman,2 Ann Haerskjold3,4
1Centre for Pharmacoepidemiology, Department of Medicine, Karolinska Institutet, Solna, Stockholm, Sweden; 2Stockholm-Uppsala Department of Pediatric Cardiology, Astrid Lindgren Children's Hospital, Karolinska University Hospital and Department of Women's and Children's Health, Karolinska Institutet, Stockholm, Sweden; 3Child and Adolescent Clinic, Pediatric Department, 4Research Unit Women's and Children's Health, the Juliane Marie Centre for Women, Children and Reproduction, Copenhagen University Hospital, Rigshospitalet Hospital, Copenhagen, Denmark
Background: Register studies are a valuable tool, when monitoring the safety of drugs. The Swedish Prescribed Drug Register (PDR) was established in 2005 and keeps records of all prescribed drugs dispensed in community pharmacies. Drugs prescribed in-hospital are not registered on an individual level, which may hamper the validity of register-based studies on drugs potentially administered in-hospital.
Objective: The objective was to assess the ability of the PDR to identify children treated with the monoclonal antibody palivizumab, which is used for prophylaxis against respiratory syncytial virus (RSV) infection in children.
Methods: Palivizumab exposure as filled prescriptions recorded in the PDR was assessed by indication of treatment (preterm-born children, bronchopulmonary dysplasia, or hemodynamically significant heart disease) and presented as numbers and proportions. For a random sample of children with an indication for treatment and without record of palivizumab exposure in the drug register, numbers and proportions by indication of treatment as noted in medical records were presented. The extent of underreporting in the drug register was estimated by indication for treatment.
Results: Through the national health registers, 2,317 children were identified as being at risk for severe infection with RSV infection and 75% had no records indicating palivizumab exposure in the PDR. In a random sample of 176 children at high risk for RSV infection and with no records of palivizumab prescription fills in the PDR, 47% had been treated with palivizumab according to medical records. The PDR underestimated palivizumab treatment with 49% in children born preterm, 42% in children with bronchopulmonary dysplasia, and 23% in those with a hemodynamically significant heart disease.
Conclusion: Our findings underline the need of improving the information in the Swedish national registers concerning drugs administered in-hospital.
Keywords: validation, drug, respiratory syncytical virus, health register, medical records
Introduction
The introduction of new drugs requires extensive preclinical studies prior to approval. Clinical trials and postapproval follow-up studies are important tools in capturing effectiveness of a drug and long-term adverse effects. Register studies are particularly important for monitoring the safety of drugs after approval.1 The Nordic countries have a long tradition for register-based epidemiological research. Such research has been facilitated by the national health registers.2,3 The tracking of individual disease and prescription data over time is made feasible by linking individual information using a unique person identifier, the Central Personal Registration number. Since July 2005, the Swedish Prescribed Drug Register (PDR) has kept records of all prescribed drugs dispensed in Swedish community pharmacies, but the register only includes prescribed drugs picked up at pharmacies and not drugs administered in-hospital.4
In Sweden, the monoclonal antibody palivizumab (Synagis®) is approved for the prophylaxis against respiratory syncytial virus (RSV) infection in children born preterm, with bronchopulmonary dysplasia (BPD) or with hemodynamically significant heart disease (HSHD). Palivizumab is administered as monthly injections throughout the RSV season (November to March). The treatment is expensive, and the regulatory authorities have recommended a more restrictive approach than the approved indication (Table 1).5–7
  | Table 1 Approved indications and clinical recommendations for palivizumab prophylaxis |
Population-based databases on drug utilization are unique tools in pharmacoepidemiologic research, given that registrations are complete and valid. In an attempt to facilitate future assessments using register-based studies, the objective of this study is to assess the ability of the Swedish health registers to identify children treated with palivizumab as compared with information in medical records.
Materials and methods
Registration of palivizumab exposure as recorded in the PDR was assessed by indication for treatment. Missing information on treatment with palivizumab in the PDR concerning children at high risk for RSV infection was assessed through scrutinizing medical records for notification of treatment.
Data sources
The Central Personal Registration number was used to link the following registries: The Medical Birth Register (MBR), the National Patient Register (NPR), and the PDR. The PDR includes data on dispensed medication, including doses and date of dispensing on all prescriptions for Swedish inhabitants dispensed at Swedish community pharmacies. Drugs in the PDR are classified according to the Anatomical Therapeutic Chemical (ATC) classification system. Some counties in Sweden may register in-hospital administration as a procedure code together with the ATC code into NPR. However, at present no systematic nationwide recording of in-hospital treatment exists. The NPR includes information on all in-patient and out-patient contacts at hospitals, and diagnoses are recorded by means of the International Classification of Diseases. For the study period the 10th version was used.
Study population
Using the MBR, we identified a study population of 582,822 live-born infants born between July 1, 2005, and December 31, 2010. Based on the national recommendations (Table 1), we identified three cohorts of children recommended for palivizumab prophylaxis:
- Children born before gestational week 26 were identified using information from MBR.
- Children with an International Classification of Diseases, version 10 code of BPD were identified using information from MBR or NPR.
- Children with HSHD were selected based on an algorithm combining data on HSHD-specific hospitalizations and HSHD-specific prescribed medications adding criteria for age at hospitalization and repeated medication.
The algorithm to identify children with HSHD was developed by a specialist in pediatric cardiology (GB).
A detailed description of the algorithm is presented in the Supplementary material.
Among the children unexposed to palivizumab, we randomly selected a 10% sample of each of the high-risk groups for medical record review and included an equal fraction of children for each study year. All medical records were reviewed until the child’s second birthday or the first notification of palivizumab treatment.
Data collection
Medical records were reviewed, and the palivizumab exposure status was recorded using a standardized electronic questionnaire form. The medical records were reviewed by a trained research nurse (CB) and a specialist in pediatric cardiology (GB). Information concerning palivizumab exposure was only included if it was explicitly stated that the drug had been administered.
Ethical approval
The study was approved by the regional ethical board (Regionala etikprövningsnämnden, Karolinska Institutet, Stockholm), and the National Board of Health and Welfare conducted the standard confidentiality assessment for disclosure of personal data. In addition, we obtained approval from the executive directors in each pediatric clinic.
Results
Of the 582,822 live-born children, 2,317 (0.4%) were identified as being at high risk for RSV infection according to the Swedish recommendations. In total, 943 children were recorded with a prescription of palivizumab in the PDR. Eight children were included in the NPR with an ATC code for palivizumab, of which four were also recorded in the PDR. For all the children in the random sample, it was possible to obtain medical records from at least one hospital, but for 18% of the children, the information was not complete. Thus, in total, 82% of all relevant medical records were examined.
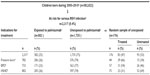
Table 2 shows the number and proportions of children who were exposed to palivizumab according to information in the PDR and in medical records. Of the 2,317 children with increased risk of severe RSV infection, 782 children (34%) were born before 26 weeks of gestation, 733 children (32%) had BPD, and 802 children (35%) had HSHD. Of the 176 randomly selected children who were unexposed to palivizumab according to the PDR, 83 (47%) had been exposed to palivizumab according to medical records. Of these, 66% were born preterm, 54% had BPD, and 31% had HSHD. Assuming that the children in the random sample are representative of the entire birth cohort, the true proportion of palivizumab exposure in the subgroups of high-risk children would be 75% for preterm, 65% for BPD, and 49% for children with HSHD. Studies based only on the information from the PDR would therefore underestimate palivizumab exposure by 49% in children born preterm, by 42% in children with BPD, and by 23% in children with HSHD.
Discussion
Our study shows the challenges when monitoring drugs potentially administered in-hospital by means of the Swedish national health registers. By identifying children, whom according to the national recommendations should have been given palivizumab prophylaxis, but were unexposed according to the PDR and assessing their treatment in medical records, we found the treatment being more prevalent than what emerges from the information in PDR. In addition, we found that a considerate proportion of children assessed as being at risk for RSV infection and fulfilling the criteria for treatment had not been treated. Reasons to refrain the treatment can be, eg, parents not giving consent, acute disease of the child, or child not born during the RSV season.
Of the total birth cohort of 582,822 children, 0.4% was assessed to have high risk of severe RSV infection with an indication for palivizumab prophylaxis in line with national recommendations. Only 25% of these children were treated with palivizumab according to the PDR. Our review of a random sample of medical records showed that among children who met the national recommendations for palivizumab prophylaxis, 66% of the preterm children, 54% of the children with BPD, and 31% of children with HSHD actually were exposed to palivizumab. The random sample shows that the true proportion of palivizumab-exposed children was underestimated by up to 49%.
Using data on palivizumab exposure obtained from the PDR when estimating palivizumab exposure in Sweden yields a gross underestimate of how commonly the prophylaxis is prescribed to Swedish children. The underestimation was related to reason for treatment and was most distinct among preterm-born children. That the register failed to identify a large proportion of preterm children, who according to the medical records had been treated with palivizumab, probably reflects the fact that these children most often and already from birth have very long hospitalization periods and frequent contacts with specialist clinics, which may give the treatment in-hospital. On doing the review of records, we identified at least one record for all children, but for 18% of the children, the information was not complete. The dropout indicates that the proportion treated with palivizumab without prescription may be slightly higher than that reported. The failure of the PDR to identify children treated with palivizumab is in line with findings from the USA.8 In that study, information in Medicaid claims data was compared with information on treatment as recorded in medical records, and the agreement between data sources was 66%. The reason for treatment was not evaluated.
Within the framework of the National Pharmaceuticals Strategy in Sweden, work is being done at this time on how to integrate individual data on ordered drugs into the PDR. The National Board of Health and Welfare has been commissioned by the government to investigate the prerequisites for integrating individual-level data for prescribed drugs into health records. The April 2013 report suggests that information on drugs administered in-hospital should be integrated in the PDR.9 In Sweden, all health care is administered by 21 separate counties. In some counties, it is already possible to register the prescribed drug administered in-hospital as a procedure code together with the ATC code for the drug. The information is transferred and entered into the NPR. However, in this study with a total birth cohort of over 500,000 children, there were only eight children who were registered in this way, and four of the children were also recorded in the PDR. A factor contributing to the significant underreporting may have been the fact that there is no specific code for palivizumab treatment in NPR, but both the ATC code and the procedure code must be recorded, and the code systems in several counties are not adjusted to ATC codes.
One of the goals of the PDR is to increase knowledge of drug use and safety. However, it is a major limitation of the register that drugs administered in-hospital are not recorded at an individual level. Palivizumab is a drug given to a vulnerable group of children for whom the effectiveness of drug and the risk of long-term adverse effects are discussed.10
Review of records is too resource intensive and time consuming, and the incomplete coverage of drugs in the Swedish quality registers makes them less suitable for studies on drug use and safety.11 We believe our example of underestimation of palivizumab exposure when relying on recording PDRs would apply to several other drugs, which for economical or practical reasons are partly administered in-hospital.12 The methods of monitoring these drugs administered in-hospital should therefore be facilitated.13 Prospectively collected data in the PDR should be a cost-efficient method of monitoring drug use and long-term effects. In order to obtain this, it is of crucial importance to complement the PDR data with information on an individual level for drugs administered in-hospital.
The result highlights an important limitation of the PDR when monitoring effectiveness and safety of a drug after approval. In our opinion, it is important to have the possibility of studying the use of drugs in an efficient manner, no matter how they are prescribed, and without additional work for those who take care of the patients.
Acknowledgment
We acknowledge Dr Lone Graff-Stensballe for initiating the project, from which this study emerges.
Disclosure
The study was commissioned by AbbVie. AbbVie was not involved in the implementation or the collection of data, nor did AbbVie participate in the compilation of data, analyses, interpretation of results, or approval of the manuscript. The authors report no other conflicts of interest in this work.
References
Directive 2001/83/EC of the European parliament and the council of 6th November 2001 on the community code relating to medical products for human use; 2014. Available from: http://ec.europa.eu/health/files/eudralex/vol-1/dir_2001_83_cons2009/2001_83_cons2009_en.pdf. Accessed August 28, 2014. | |
Frank L. Epidemiology. When an entire country is a cohort. Science. 2000;287:2398–2399. | |
Furu K, Wettermark B, Andersen M, Martikainen JE, Almarsdottir AB, Sorensen HT. The Nordic countries as a cohort for pharmacoepidemiological research. Basic Clin Pharmacol Toxicol. 2010;106:86–94. | |
Wettermark B, Hammar N, Fored CM, et al. The new Swedish Prescribed Drug Register – opportunities for pharmacoepidemiological research and experience from the first six months. Pharmacoepidemiol Drug Saf. 2007;16:726–735. | |
Lakemedelsverket Medical Products Agency. 2013 Available from: http://www.lakemedelsverket.se/malgrupp/Halso---sjukvard/Behandlings--rekommendationer/Behandlingsrekommendation---listan/RSV-infektioner/. Accessed September 23, 2013. | |
Ahlquest Rastad J. Handläggning av RSV infektioner (Management of RSV infections); 2014. Available from: http://lakemedelsverket.se/upload/halso-och sjukvard/behandlingsrekommendationer/rsv2000.pdf. Accessed July 1, 2014. | |
Naver L, Eriksson M, Ewald U, Linde A. Prophylaxis against RSV infection. Lakartidningen. 2002;99(3):170–171. | |
Jacobson VJ, Feaganes J, Wegner S. Reliability of Medicaid claims versus medical record data: in a cost analysis of palivizumab. Pharmacoeconomics. 2007;25:793–800. | |
Socialstyrelsen (National Board of Health and Welfare). 2013 ann. [cited October 10, 2013]. Uppfölning av revisitionsläkemedel-förutsättningar för integrering i hälsodataregisteret [Monitoring ordered drug-prerequisites for integration into national health registers]. 2014; Stockholm, Sweden. [Report]. | |
American Academy of Pediatrics Committee on Infectious Diseases, American Academy of Pediatrics Bronchiolitis Guidelines Committee. Updated guidance for palivizumab prophylaxis among infants and young children at increased risk of hospitalization for respiratory syncytial virus infection. Pediatrics. 2014;134(2):415–420. | |
Rapport frän SNS forskningsprogram, Hanna Gyllensten och Katarina Steen Carlsson. Nya läkemedel och läkemedels relaterad sjuklighet: Analysmöligheter i svenska registerdata [New drug and drug related morbidity; possibilities for assessment through register based data]; September 1, 2013; Stockholm [Report]. | |
Stephansson O, Granath F, Svensson T, Haglund B, Ekbom A, Kieler H. Drug use during pregnancy in Sweden – assessed by the Prescribed Drug Register and the Medical Birth Register. Clin Epidemiol. 2011;3:43–50. | |
Hansel TT, Kropshofer H, Singer T, Mitchell JA, George AJ. The safety and side effects of monoclonal antibodies. Nat Rev Drug Discov. 2010;9:325–338. |
Supplementary material
Algorithms to identify children with hemodynamic significant heart disease according to national Swedish recommendations for treatment with palivizumab. Information was obtained from the national health registers. Conditions were defined using a combination of codes from the International Classification of Diseases (ICD-10), Nordic Classification of Surgical Procedures, and recording of pharmacological treatment by the Anatomical Therapeutic Chemical Classification Systems.
- Infants below 6 months of age with a significant heart disease and Down syndrome or other chromosomal abnormality or known immunodeficiency or significant syndrome.
- Chromosomal abnormalities, not elsewhere classified (Q9)
- Congenital malformation syndromes due to known exogenous causes, not elsewhere classified (Q86)
- Other specified congenital malformation syndromes affecting multiple systems (Q87)
- Other congenital malformations, not elsewhere classified (Q89)
- Immunodeficiency with predominantly antibody defects (D80)
- Combined immunodeficiencies (D81)
- Immunodeficiency associated with other major defects (D82)
- Infants below 6 months of age with left-to-right shunt. Diagnoses, procedures and filling of prescriptions must appear before six months of age. Infants with surgery one month of age or younger are not included.
- Ventricular septal defect (Q210) AND diuretics (C03) OR agents acting on the renin–angiotensin system (C09) AND
- Closure of isolated congenital ventricular septal defect (FHB) OR
- Closure of multiple congenital ventricular septal defects (FHC) OR
- Banding operations on pulmonary artery (FBC)
- Atrial septal defect (Q211) AND diuretics (C03) OR agents acting on the renin–angiotensin system (C09) AND closure of isolated atrial septal defect (FFC)
- Atrioventricular septal defect (Q212) AND diuretics (C03) OR agents acting on the renin–angiotensin system (C09) AND
- Repair of complete atrioventricular septal defect (FHD) OR
- Operations for partial atrioventricular septal defect (FFD) OR
- Banding operations on pulmonary artery (FBC)
- Aortopulmonary septal defect (Q214) AND diuretics (C03) OR agents acting on the renin–angiotensin system (C09) AND closure of congenital fistula from aorta (FDD10, FDD13, FDD20)
- Patent ductus arteriosus (Q250) AND diuretics (C03) OR agents acting on the renin–angiotensin system (C09) AND closure of patent ductus arteriosus (FDE)
- Infants below twelve months of age with a univentricular heart or children where the primary pulmonary blood supply comes from a Glenn anastomosis. Diagnoses or procedures must appear before twelve months of age.
- Double inlet ventricle (Q204)
- Hypoplastic right heart syndrome (Q226)
- Hypoplastic left heart syndrome (Q234)
- Atresia of aorta (Q252)
- Discordant ventriculoarterial connection (Q203) AND discordant atrioventricular connection (Q205) AND pulmonary valve atresia (Q220) AND ventricular septal defect (Q210)
- Pulmonary valve atresia (Q220) AND malformation of coronary vessels (Q245)
- Ebstein’s anomaly (Q225) AND pulmonary valve atresia (Q220)
- Ebstein’s anomaly (Q225) AND congenital pulmonary valve stenosis (Q221)
- Congenital tricuspid stenosis (Q224) AND connection to pulmonary artery from superior vena cava (FAE)
- Congenital mitral stenosis (Q232) AND connection to pulmonary artery from superior vena cava (FAE)
- Aortopulmonary anastomosis in single ventricle conditions (FBL40)
- Surgery for hypoplastic left heart syndrome (FDA)
- Anastomosis to pulmonary artery from superior vena cava (FAE00)
- Bidirectional anastomosis between superior vena cava and pulmonary artery (FAE10)
- Infants below 12 months of age with structural heart disease and lung disease, and with surgical heart repair before 12 months of age. Diagnoses or procedures must appear before twelve months of age.
- Congenital malformations of the circulatory system (Q2)
- Congenital malformations of nose (Q30)
- Congenital malformations of larynx (Q31)
- Congenital malformations of trachea and bronchus (Q32)
- Congenital malformations of lung (Q33)
- Other congenital malformations of respiratory system (Q34)
- Cystic fibrosis (E84)
- Diseases of vocal cords and larynx, not elsewhere classified (J38)
- Chronic lower respiratory diseases except asthma (J40-J44, J47)
- Neonatal aspiration syndromes (P24)
- Interstitial emphysema and related conditions originating in the perinatal period (P25)
- Chronic respiratory disease originating in the perinatal period (P27)
- Other respiratory conditions originating in the perinatal period (P28), except for apnea (P283, P284)
- Surgery of heart or major thoracic vessels (FA, FB, FC, FD, FE, FF, FG, FH, FI, FJ, FK, FL, FM, FN, FO, FQ, FR, FS, FT, FU, FV, FY, FZ)
- Infants below 12 months of age with pulmonary hypertension and with former heart surgery. Diagnoses or procedures must appear before twelve months of age. Those recorded with pulmonary hypertension as a single diagnosis before two months of age are not included. Infants recorded with a surgical procedure must have at least one diagnosis recorded after the procedure.
- Pulmonary hypertension (I27) at two occasions or more
- Persistent pulmonary hypertension of the newborn (P293X*) at two occasions or more
- Surgery on heart or major thoracic vessels (FA, FB, FC, FD, FE, FF, FG, FH, FI, FJ, FK, FL, FM,FN, FO, FQ, FR, FS, FT, FU, FV, FY, FZ) followed by a diagnosis of pulmonary hypertension (I27 or P293X
- Infants below 12 months of age with a diagnosis of cardiomyopathy and heart failure, whom are on triple medication. Diagnoses, procedures or filling of prescriptions must appear before twelve months of age. Children with a heart transplant before two years of age are also included.
- Cardiomyopathy (I42) and heart failure (I50) with a combination of drugs from at least three drug classes (B01, C01-3, C07, C09, G04) during a three-month period.
- B01
- Iloprost (B01AC11)
- C01
- Cardiac glycosides (C01A)
- Adrenergic and dopaminergic agents (C01CA)
- Phosphodiesterase inhibitors (C01CE)
- Other cardiac stimulants (C01CX)
- C02
- Bosentan (C02KX01)
- C03
- High-ceiling diuretics (C03C)
- Potassium-sparing agents (C03D)
- Low-ceiling diuretics, thiazides (C03A)
- C07
- Beta blocking agents (C07A)
- C09
- Ace inhibitors, plain (C09A)
- Angiotensin II antagonists, plain (C09C)
- G04
- Sildenafil (G04BE03)
- Transplantation of heart (FQA)
- Transplantation of heart and lung (FQB)
- Heart transplant status (Z941)
- Lung transplant status (Z942)
- Heart and lungs transplant status (Z943)
AND
AND
*X denotes national subcode.
 © 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.