Back to Journals » International Medical Case Reports Journal » Volume 7
Unexpected difficult airway with hypogonadotropic hypogonadism
Authors Yaman F, Arslan B, Yuvanç E, Büyükkoçak Ü
Received 28 January 2014
Accepted for publication 20 February 2014
Published 5 April 2014 Volume 2014:7 Pages 75—77
DOI https://doi.org/10.2147/IMCRJ.S61440
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Ferda Yaman,1 Bengi Arslan,2 Ercan Yuvanç,3 Ünase Büyükkoçak1
1Anesthesiology and Reanimation Department, 2Otorhinolaryngology Head and Neck Surgery Department, 3Urology Department, Faculty of Medicine, Kirikkale University, Kirikkale, Turkey
Background: A critical aspect of safe general anesthesia is providing adequate ventilation and oxygenation. Failed endotracheal intubation and inadequate ventilation with insufficient oxygenation may lead to serious complications, even death. Anesthesiologists rarely encounter unexpected difficult airway problems in daily routine. Management of an unexpectedly difficult airway consists of laryngeal mask ventilation, gum-elastic bougie and video laryngoscopy-assisted intubation. Gum-elastic bougie is the easiest and cheapest tool used in case of an unexpected difficult intubation occurring in the operating room.
Case: A 53-year-old male patient with hypogonadotropic hypogonadism presented as an unexpected difficult intubation after the induction of anesthesia. No pathological finding or predictor of difficult intubation was present. In addition, bag-mask ventilation was poor and inadequate. The patient was finally successfully intubated with a gum-elastic bougie.
Conclusion: A difficult airway has been described in patients with a variety of endocrine disorders, including pituitary diseases, but not with hypogonadism. There may be an unrevealed relationship between hypogonadism and difficult airway. Gum-elastic bougie is still the most attainable and effective tool in the operation room in this situation.
Keywords: airway management, intubation, hypogonadism
Introduction
Anesthesiologists are responsible for maintaining a patent airway in the anesthetized patient. Failed endotracheal intubation and inadequate ventilation with insufficient oxygenation may lead to serious complications, as even a few minutes of deoxygenation can result in catastrophic outcome like brain damage or even death.1 Anesthesiologists are occasionally faced and challenged with this significant problem in practice. A difficult airway has been described in patients with pituitary endocrine disorders such as acromegaly and dwarfism; however, airway problems with hypogonadism have not been well identified in the literature.2
Case
A 53-year-old married man (weight: 85 kg, height: 187 cm, body mass index: 24 kg/m²) presented with a history of nasal obstruction for two years. Otorhinolaryngologists planned a septoplasty operation under general anesthesia for him. He had not had any prior operation under general anesthesia, so he did not have any history of difficult intubation, and he did not have any chronic systemic disease. The patient was evaluated for obstructive sleep apnea syndrome (OSAS) with a comprehensive questionnaire on his sleeping habits and medical history; no complaints or predictors pertaining to OSAS were identified.
The patient’s preoperative airway assessment was normal, Mallampati class was II, thyromental distance was 7 cm, inter-incisor gap was 5 cm, and head extension was >35°. His physical examination was characterized by lack of secondary sexual characteristics and presence of fine facial wrinkles. Although, as previously indicated, the patient was married, he had had no children. He had consulted urologists, and primary infertility and erectile dysfunction had been diagnosed. His hormone profile was: testosterone 0.3 ng/mL (reference range 1.75–7.81), free testosterone 0.91 (reference range 4.5–42.0), prolactin 1.31 ng/mL (reference range 2.64–26.72), luteinizing hormone (LH) 0.33 mIU/mL (reference range 1.24–103.03). His thyroid hormone levels were normal. No other pathological finding was obtained as the result of magnetic resonance imaging of the pituitary gland. Thus, the patients was diagnosed with primary hypogonadotropic hypogonadism.
He was admitted to the operating theater, and following the induction of anesthesia with a dose of 5 mg/kg intravenous thiopental, bag-mask ventilation was barely sustained. Fentanyl (1–2 μgr/kg) and, as a muscle relaxant, rocuronium (0.6 mg/kg) were administered. While the patient’s head was in the sniffing position, direct laryngoscopy and intubation of the trachea were attempted three times with different sizes of Macintosh and Miller blades by an assistant professor of anesthesiology with 5 years’ experience. However, unfortunately, the intubation failed. The lungs were then ventilated with 100% oxygen via a face mask in order to avoid desaturation. Glottic visualization was assessed with Cook’s modification of the Cormack–Lehane classification; a grade of 3A (with direct laryngoscopy, only the epiglottis can be visualized; the epiglottis can be lifted using an introducer or bougie) was assigned.3 The patient was subsequently successfully intubated with a gum-elastic bougie.
After the operation, the patient was extubated successfully without any complication and then examined by otorhinolaryngologists via flexible laryngoscopy. The epiglottis was found to be in a slightly lower than normal position (Figure 1).
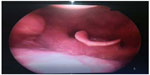  | Figure 1 Flexible laryngoscopic view of larynx. |
Discussion
The overall incidence of unexpected difficult intubation is estimated to be 1%–3%, while failed intubation incidence is 0.05%–0.35% in Europe.1 Difficult endotracheal intubation has been described in patients with pituitary diseases like acromegaly, Cushing’s disease, LH/follicle-stimulating hormone-secreting adenoma, thyroid-stimulating hormone-secreting adenoma, nonfunctional adenoma and prolactinoma.4 Difficult airway with dwarfism has also been described. However, difficult airway with a hypogonadotropic patient has not yet been clearly defined. In our case, the pituitary hormone profile was found to be abnormal. prolactin and LH levels were found to be lower than normal. Total and free testosterone levels were remarkably low. Further, magnetic resonance imaging of the pituitary gland did not reveal any adenoma or mass lesion.2
Pulsatile release of follicle stimulating hormone and LH in puberty instigates the development of the male larynx and secondary sexual characteristics. The growth of laryngeal cartilages and maturation of the male larynx is also facilitated by androgen. High-affinity androgen receptors have been found in the human larynx.5,6 In this case, the patient’s laryngeal development was compatible with his age and sex. Only the epiglottis was located in a slightly lower position than normal, partially leaning toward the laryngeal passage. The patient was infertile and lacked secondary sexual characteristics due to insufficient exposure to androgens. This may also have contributed to the lower position of the epiglottis.
The relationship between OSAS and difficult airway is widely discussed in the literature. The rate of difficult intubation has been found to be higher in OSAS patients than the normal, healthy population.7 Body mass index, Mallampati grading, Cormack–Lehane classification, sternomental distance, and thyromental distance evaluation might be predictive factors for difficult airway in OSAS patients. As such, anesthesiologists must be aware of this fact and be prepared for difficult intubation in OSAS patients.7 However, the rate of difficult intubation has not been found to be related to the severity of OSAS.8 No significant relationship between the apnea–hypopnea index and difficult intubation has been found.8 In our patient, no apnea and daytime sleepiness were present in his history. Only snoring was present, which might well have been associated with nasal septal deviation. His body mass index was 24 kg/m2, Mallampati class was II, thyromental distance was 7 cm, inter-incisor gap was 5 cm, and head extension was above 35°. These findings did not suggest any evidence of OSAS or difficult airway. Therefore, no further evaluations or tests were required.
The gold-standard diagnostic tool for OSAS is laboratory-based overnight polysomnography. This multiparameter test reveals the presence and severity of OSAS.9 In this case, as there was no clinical index of suspicion for OSAS and to keep costs down, polysomnography was not required by the otorhinolaryngologists.
Conclusion
There may be a relationship between hypogonadotropic hypogonadism and difficult airway without OSAS. Further clinical investigations are needed for the detection of such a correlation. Thus, anesthesiologists must take into account difficult airway in endocrinological disorders like hypogonadotropic hypogonadism and be prepared for difficult intubation.
Disclosure
The authors declare no conflicts of interest in this work.
References
Henderson JJ, Popat MT, Latto IP, Pearce AC; Difficult Airway Society. Difficult Airway Society guidelines for management of the unanticipated difficult intubation. Anaesthesia. 2004;59(7):675–694. | |
Manikandan S, Neema PK, Rathod RC. Airway problems caused by hypogonadism in male patients undergoing neurosurgery. Anesth Analg. 2005;101(6):1812–1815. | |
Cook TM. A new practical classification of laryngeal view. Anaesthesia. 2000;55(3):274–279. | |
Nemergut EC, Zuo Z. Airway management in patients with pituitary disease: a review of 746 patients. J Neurosurg Anesthesiol. 2006;18(1):73–77. | |
Beckford NS, Rood SR, Schaid D, Schanbacher B. Androgen stimulation and laryngeal development. Ann Otol Rhinol Laryngol. 1985;94(6 Pt 1):634–640. | |
Kahane JC. Growth of the human prepubertal and pubertal larynx. J Speech Hear Res. 1982;25(3):446–455. | |
Kurtipek O, Isik B, Arslan M, Unal Y, Kizil Y, Kemaloglu Y. A study to investigate the relationship between difficult intubation and prediction criterion of difficult intubation in patients with obstructive sleep apnea syndrome. J Res Med Sci. 2012;17(7):615–620. | |
Siyam MA, Benhamou D. Difficult endotracheal intubation in patients with sleep apnea syndrome. Anesth Analg. 2002;95(4):1098–1102. | |
McNicholas WT. Diagnosis of obstructive sleep apnea in adults. Proc Am Thorac Soc. 2008;5(2):154–160. |
 © 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
