Back to Journals » Advances in Medical Education and Practice » Volume 5
Surgical teaching program for our senior medical students: room for improvement
Authors Burgess A , Wright C, Qasabian R, O'Mara D, Mellis C
Received 30 June 2014
Accepted for publication 8 August 2014
Published 10 October 2014 Volume 2014:5 Pages 369—375
DOI https://doi.org/10.2147/AMEP.S63373
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 6
Editor who approved publication: Dr Md Anwarul Azim Majumder
Annette Burgess,1 Caroline Wright,1 Raffi Qasabian,1 Deborah O'Mara,2 Craig Mellis1
1Central Clinical School, Sydney Medical School, University of Sydney, Sydney, NSW, Australia; 2Assessment Unit, Sydney Medical School, University of Sydney, Sydney, NSW, Australia
Background: To ensure the quality of surgical teaching within our graduate entry medical program, a distinctive surgical teaching program has been developed at Sydney Medical School-Central. Spanning 2 years, the program includes lectures, small group surgical clinical tutorials, and formal student surgical grand rounds presentations, plus clinical placements and attendance in operating theaters. We sought to evaluate the effectiveness of the program.
Methods: In 2013, at the completion of year 4, all graduating students (n=54) were asked to complete an open and closed-ended questionnaire regarding their experience of the surgical program.
Results: A total of 44/54 (81%) students completed the questionnaire. Students reported a high level of engagement with their experience in clinical tutorials, and a moderate level of engagement in surgical lectures. Students found the clinical attachment to be the least useful method of teaching, with the surgical grand rounds presentation also eliciting a poor response from students.
Conclusion: While both large group lectures and small group learner-centered teaching methods were highly valued by students, changes are needed to enhance clinical attachments for students in surgical wards. The benefits of students being made to feel part of a team during their surgical clinical attachments, along with adequate inpatient contact and formative feedback, should not be underestimated.
Keywords: surgery teaching, curriculum, medical program
Introduction
The design of education and training models within undergraduate medical education is a critical issue that has received substantial attention in the medical education literature.1 Increased demands on university and hospital teaching staff, limited resources, and reduced patient availability are issues that have contributed to this discussion. Additionally, with the substantial and ever increasing body of medical and surgical knowledge available, there has been a general trend to reduce the overall curricula content within medical education,2 and in particular, a reduction in surgical teaching within the undergraduate medical curriculum.
In recent years, the demands of the health care system have placed increased strains on clinicians’ commitments to teaching.3 Often, there is an imbalance between the service and education goals of the teaching hospitals, and an inadequate focus on developing the teaching skills of clinicians.4 The provision of small group interactive learning is restricted by faculty availability, and sometimes students can go through clinical attachments without being directly observed taking a history or examining a patient.3,5
The changing disease profiles and subsequent changing nature of health care provision in developed countries has contributed to a reassessment of clinical setting needs for medical student teaching.6 There has been a trend toward a reduction in the quantity of surgical teaching within undergraduate medical curricula, with an increased emphasis on community-based teaching.2,6
To safeguard the volume of surgical teaching, and in an effort to increase the quality of surgical teaching for students, a distinctive surgical teaching program was developed by a senior academic surgeon to complement the surgical content of the existing faculty-wide curriculum. The surgical teaching program was implemented at Sydney Medical School-Central, during stage 3 (years 3 and 4) of a 4-year graduate entry medical degree. The program includes four key components: surgical lectures, clinical tutorials, student grand rounds presentations, and clinical placements. While these components are not unique to this program, their structured delivery is more typical of “older style” undergraduate surgical teaching, but aim to involve both didactic and Socratic teaching methods.
Surgical lectures
In addition to the ten standard Sydney Medical School core surgical curriculum lectures that take place over a 2-year period in years 3 and 4 of the medical program, two further surgical lectures are given each week over an 8-week period during the first term (for a total of 16 lectures) of year 3 (ie, term A, mid-January to mid-March).
Small group surgical clinical tutorials
Surgical small group tutorials (on average 6–8 students) take place throughout years 3 and 4. Each student attends a total of 16 small group tutorials with senior surgeons. The topics for discussion are based on the surgical lecture program content and the same subjects are discussed in years 3 and 4. However, in year 3, the primary focus is on pathophysiology and anatomy, whereas in year 4, emphasis is placed on the clinical management of different surgical conditions.
Long case presentations at surgical rounds
Each stage 3 student is required to present a formal 20-minute long case presentation to their peers. These weekly presentations are chaired by two senior surgeons. Ten minutes is then allowed for questioning and discussion. The case presentation is centered on a patient clerked by the student during their general surgical attachment. The student is expected to attend their patient’s operation and follow them up postoperatively. Students are encouraged to present common surgical conditions rather than unusual and rare clinical conditions, as these presentations are essentially a teaching forum for both the presenter and their student peers. Presentations are in a slideshow format and illustrations, deidentified X-rays, pathology, and operation photographs are included. Each student presenting receives a written formative assessment from their surgical supervisors, which is closely aligned with the long case clinical examination marking system.
Clinical placement and operating theaters
During either year 3 or year 4 of the medical program, each student is attached to a surgical unit for 8 weeks. This comprises 4 weeks in a so-called “general surgery unit” at the hospital, ie, either upper gastrointestinal surgery, colorectal surgery, vascular surgery, melanoma and surgical oncology, breast surgery, transplant surgery, or cardiothoracic surgery. In addition, each student attends 4 weeks in a “specialty” surgery unit, comprising a 2-week placement in ear, nose and throat surgery, and a 2-week placement in ophthalmology. During these surgical placements, students are expected to attend the operating theater.
This study aimed to evaluate students’ experience of our current surgical teaching program for the purpose of improving the quality of curriculum delivery in surgery.
Materials and methods
All students (n=54) were required to take part in the surgical program. At the completion of year 4, all graduating students (n=54) were asked to complete a questionnaire regarding their experience of the surgical program. The questionnaire consisted of six closed questions, relating to each of the four surgical program components, with responses ranging from “strongly disagree” (1) to “strongly agree” (5) on a five-point Likert scale. The questionnaire also included two open-ended questions, aimed at eliciting responses from students regarding the “most useful” and “least useful” aspects of the experience.
The survey questions were based on the aims of the surgical program, which are to develop students’ surgical knowledge and understanding, prepare students for their written and clinical examinations, and to prepare students to work as medical interns. The questions were designed to provide effective feedback on student experiences in the environment.7 Descriptive statistics were used to analyze the data.8 Ethics approval was obtained from The University of Sydney human research ethics committee.
Results
A total of 44/54 (81%) of all graduating year 4 students completed the questionnaire. Of the 44 respondents, 37 provided information regarding their age and sex. Fourteen of these 37 students were female and 23 students were male, with ages ranging from 24 to 35 years, a standard deviation of 3.5, and a mean age of 27.4 years.
Survey responses
Closed item responses
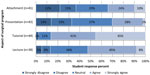
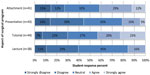
Results of the survey responses are shown in Figure 1 (question 1), Figure 2 (question 2), Figure 3 (question 3), Figure 4 (question 4), Figure 5 (question 5), and Figure 6 (question 6). Students reported a high level of engagement with their experience in clinical tutorials, and a moderate level of engagement in surgical lectures. Students found the clinical attachment to be the least useful method of teaching, with the surgical grand rounds also eliciting a relatively poor response from students.
  | Figure 1 Student response to question 1: [This aspect of the surgical program] provided a helpful method of teaching (n=44). |
  | Figure 2 Student response to question 2: [This aspect of the surgical program] improved my knowledge base of surgery (n=44). |
  | Figure 3 Student response to question 3: [This aspect of the surgical program] improved my understanding of surgery (n=44). |
  | Figure 4 Student response to question 4: [This aspect of the surgical program] was useful in preparation of my long case clinical examination (n=44). |
  | Figure 5 Student response to question 5: [This aspect of the surgical program] was useful in preparation for my written examinations (n=44). |
  | Figure 6 Student response to question 6: [This aspect of the surgical program] improved my competence in surgical clinical skills (n=44). |
Free-text feedback
Comments regarding the most useful and least useful aspects of each of the surgical program components are presented in Table 1. In summary, the most valuable aspect of the surgical program for students was the presence of surgical specialists, and their ability to provide a clinical context, hence increasing relevance to learning. Students reported that being made to feel part of a surgical team on wards increased their learning opportunities. Students thought that the surgical curriculum was well covered within the lectures and case presentations, and requested that the lectures be recorded. Students reported being least engaged when the surgical team was not inclusive in their activities, the medical team was too specialized, or when there were too many students attached to one team.
Discussion
Our results demonstrate that the surveyed students favored clinical tutorials and surgical lectures, and least favored clinical attachment (including operating theater exposure) and surgical rounds student presentations. Five attributes that may be key to a good surgical teaching program were identified: relevant course content; reinforcement of material (covered in lectures, then again in small group tutorials); interaction with senior surgeons (to establish clinical relevance); small group experience; and feeling part of a team. Each of these attributes is discussed below.
Content of teaching material
Students felt that the content delivered throughout the surgical program, particularly in the surgical lectures, was relevant and helpful, with essential components of the curriculum linked to assessment and covered in engaging ways. Conversely, students did not find highly specialized clinical attachments useful to their learning. Sixteen percent of students found the teams too specialized, and wanted exposure to more general surgical problems. This is likely due to the fact that more common surgical problems would be better aligned with assessment criteria. Additionally, motivation to learn is reduced once students feel that learning is too complex, such that competence may not be readily achieved.9
Timing of delivery of material
The intent of the lectures is to provide a core knowledge base to prepare students for their clinical attachments and tutorials, but timing of the lectures is important. Students expressed difficulty in recalling the information at examination time, with three quarters of the students sitting the written examination more than 8 months after delivery of the lectures, the remainder, 20 months after. The introduction of modern vertically integrated medical programs has made coordination and timely delivery of lectures difficult. It is also clear that lectures should be recorded for subsequent revision.
Contact with surgical specialist (and clinical context/relevance)
In both the grand rounds and clinical tutorials, students valued the presence of senior surgical staff. Knowledge and understanding is more readily developed when explained within the relevant clinical context,10 and the experience that senior surgeons can offer is invaluable.
Equally, it seems that the limited contact with senior surgeons during clinical attachments may have contributed to reduced student satisfaction. The demands of modern health care systems have unfortunately placed increased strains on clinicians’ commitments to teaching.3 Active learning for senior students demands that clinical skills be developed through supervised provision of patient care, until a high level of proficiency is attained.1 However, with the increase in focus on patient safety and quality of care, and limited availability of clinical supervisors, students may be spending more time as passive observers, rather than active participants. Ideally, formal structured teaching on the wards by senior surgical consultants would assist in improving the students’ experience.
Small group learning
Undoubtedly the most favored method of teaching by students was the surgical clinical tutorials. Students value small group teaching and learning, and Socratic teaching methods. Principles of small group learning provide frequent opportunities for feedback from experienced teachers.11 Empirical evidence suggests that active learning pedagogies that engage students provide both cognitive and metacognitive benefits, including a deeper understanding of knowledge and greater knowledge retention.12,13
Feeling part of a team
It is important that students feel part of a team when they are allocated to surgical clinical attachments. However, as is commonly reported in large teaching hospitals, 18% of students commented that they were not made to feel part of the team. Medical education can be viewed as a process of socialization, which helps to redefine the task of clinical teachers.14 It is important that medical, nursing, and allied health staff are inclusive of medical students, as it reinforces their identity as valuable team members with worthwhile contributions to offer.15 Socialization can also assist in the development of professional attributes.16 It should be acknowledged, however, that it is hard for clinicians to develop sufficient rapport with students when students spend such a short time attached to a clinical unit, and have competing course requirements, including additional non-surgical lectures, tutorials, and problem-based learning.
Future directions
We plan to investigate whether this specific surgical teaching program has had positive outcomes on students’ knowledge acquisition and retention, and performance in assessment tasks. It has not been possible to conduct a valid comparison with other clinical schools in Sydney Medical School to date due to the process of allocating students to schools having an inbuilt academic bias. However, from the year 3 intake in 2013, a valid comparative analysis will be afforded through random allocation of students to clinical schools.
The quality of the teaching program may be improved by involvement of greater numbers of senior surgeons, and with additional formal, ward-based, small group teaching activities to help socialize students into the surgical setting. Student perception and educational benefits of the surgical presentations may be increased by implementing a peer review system.
Limitations
The survey was distributed at the completion of the 2-year surgical program. Therefore, it is possible that student perception had changed within this period of time.
Conclusion
In order to overcome the obstacles of reduced surgical teaching, an innovative surgical program was developed, including small group, learner-centered teaching methods, with opportunities to apply and integrate surgical knowledge. Students felt satisfied with the additional opportunities provided, with repetition being welcomed, particularly in preparation for their examinations. However, we found that improvements are needed in clinical attachments to hospital wards for students. The importance of socialization to the surgical profession should not be underestimated, along with adequate inpatient contact, with formative feedback to guide improvement in knowledge and skills.3
Acknowledgment
The authors would like to acknowledge Professor George Ramsey-Stewart, clinical academic surgeon, who initially developed the program in 2000 in response to students’ concerns that the current program was not providing the prerequisite knowledge required for internship. This was achieved in consultation with the senior surgeons of the relevant surgical units.
Author contributions
AB, study concept and design, analysis and interpretation of data, drafting of manuscript; CW, analysis and interpretation of data, critical revision of manuscript for important intellectual content; RQ, analysis and interpretation of data, critical revision of manuscript for important intellectual content; DO, analysis and interpretation of data, critical revision of manuscript for important intellectual content; and CM, analysis and interpretation of data, critical revision of manuscript for important intellectual content. All authors read and approved the final manuscript.
Disclosure
The authors report no conflicts of interest in this work.
References
Cooke M, Irby D, Sullivan W, Ludmere KM. American medical education 100 years after the Flexner report. N Engl J Med. 2006;355:1339–1344. | |
Argha RA, Papanikitas BM, Baum C, Benjamin D. The teaching of surgery in the undergraduate curriculum reforms and results. Int J Surg. 2005;3:87–92. | |
Mehta N. Just imagine: new paradigms for medical education. Acad Med. 2013;88:1418–1423. | |
Ottolini MC, Cuzzi S, Tender J, et al. Decreasing variability in faculty ratings of student case presentations: a faculty development intervention focusing on reflective practice. Teach Learn Med. 2007;19:239–243. | |
Howley LD, Wilson WG. Direct observation of students during clerkship rotations: a multiyear descriptive study. Acad Med. 2004;79:276–280. | |
Thistlethwaite JE, Kidd MR, Hudson JN. General practice: a leading provider of medical student education in the 21st century? Med J Aust. 2007;187:124–128. | |
Brookfield S. Becoming a Critically Reflective Teacher. San Francisco, CA, USA: Jossey-Bass; 1995. | |
Creswell J. Educational Research: Planning, Conducting and Evaluating Quantitative and Qualitative Research. Upper Saddle River, NJ, USA: Merrill; 2002. | |
Ryan RM, Deci E. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am Psychol. 2000;55:68–78. | |
Bransford J, Brown A, Cocking R. How People Learn: Brain, Mind, Experience and School. Washington, DC, USA: National Academy Press; 1999. | |
O’Malley KJ, Moran BJ, Haidet P, et al. Validation of an observation instrument for measuring student engagement in health professions settings. Eval Health Prof. 2003;26:86–103. | |
Graffam B. Active learning in medical education: strategies for beginning implementation. Med Teach. 2007;29:38–42. | |
Biggs J. Teaching for Quality Learning at University. 2nd ed. Berkshire, UK: Open University Press; 2003. | |
Dornan T, Bundy C. What can experience add to early medical education? Consensus survey. BMJ. 2004;329:1–6. | |
Schumacher DJ, Englander R, Carraccio C. Developing the master learning: applying learning theory to the learner, the teacher, and the learning environment. Acad Med. 2013;88:1635–1645. | |
Sinclair S. Marking Doctors: An Institutional Apprenticeship. Oxford, UK: Berg; 1997. |
 © 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

