Back to Journals » Clinical Interventions in Aging » Volume 10
Repeated vertebral augmentation for new vertebral compression fractures of postvertebral augmentation patients: a nationwide cohort study
Authors Liang C, Wang H , Syu F, Wang K, Lu K, Liliang P
Received 9 January 2015
Accepted for publication 10 February 2015
Published 27 March 2015 Volume 2015:10 Pages 635—642
DOI https://doi.org/10.2147/CIA.S80668
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Zhi-Ying Wu
Cheng-Loong Liang,1 Hao-Kwan Wang,1 Fei-Kai Syu,2 Kuo-Wei Wang,1 Kang Lu,1 Po-Chou Liliang1
1Department of Neurosurgery, E-Da Hospital, I-Shou University, Kaohsiung City, Taiwan; 2Department of Pharmacy, China Medical University Hospital, Taichung City, Taiwan
Purpose: Postvertebral augmentation vertebral compression fractures are common; repeated vertebral augmentation is usually performed for prompt pain relief. This study aimed to evaluate the incidence and risk factors of repeat vertebral augmentation.
Methods: We performed a retrospective, nationwide, population-based longitudinal observation study, using the National Health Insurance Research Database (NHIRD) of Taiwan. All patients who received vertebral augmentation for vertebral compression fractures were evaluated. The collected data included patient characteristics (demographics, comorbidities, and medication exposure) and repeat vertebral augmentation. Kaplan–Meier and stratified Cox proportional hazard regressions were performed for analyses.
Results: The overall incidence of repeat vertebral augmentation was 11.3% during the follow-up until 2010. Patients with the following characteristics were at greater risk for repeat vertebral augmentation: female sex (AOR=1.24; 95% confidence interval [CI]: 1.10–2.36), advanced age (AOR=1.60; 95% CI: 1.32–2.08), diabetes mellitus (AOR=4.31; 95% CI: 4.05–5.88), cerebrovascular disease (AOR=4.09; 95% CI: 3.44–5.76), dementia (AOR=1.97; 95% CI: 1.69–2.33), blindness or low vision (AOR=3.72; 95% CI: 2.32–3.95), hypertension (AOR=2.58; 95% CI: 2.35–3.47), and hyperlipidemia (AOR=2.09; 95% CI: 1.67–2.22). Patients taking calcium/ vitamin D (AOR=2.98; 95% CI: 1.83–3.93), bisphosphonates (AOR=2.11; 95% CI: 1.26–2.61), or calcitonin (AOR=4.59; 95% CI: 3.40–5.77) were less likely to undergo repeat vertebral augmentation; however, those taking steroids (AOR=7.28; 95% CI: 6.32–8.08), acetaminophen (AOR=3.54; 95% CI: 2.75–4.83), or nonsteroidal anti-inflammatory drugs (NSAIDs) (AOR=6.14; 95% CI: 5.08–7.41) were more likely to undergo repeat vertebral augmentation.
Conclusion: We conclude that the incidence of repeat vertebral augmentation is rather high. An understanding of risk factors predicting repeat vertebral augmentation provides valuable basis to improve health care for geriatric populations.
Keywords: vertebroplasty, kyphoplasty, comorbidity, bisphosphonate, old age
Two Letters to the Editor have been recieved and published
İlhan et al
Wilson et al
Introduction
Osteoporotic vertebral compression fracture (VCF) with refractory pain is a crippling disorder frequently resulting in severe and prolonged back pain, lengthy hospitalization, physical decline, and increased risk of death.1,2 Bed rest, opioid analgesia, and external bracing have had limited success.3 Percutaneous vertebral augmentation was introduced as an alternative for acute VCFs refractory to conventional medical therapy.4–6 Although there is still debate over the effects of vertebral augmentation,7,8 it has gained acceptance as a minimally invasive method for pain relief.3–6 There has been a significant increase in the number of vertebral augmentation procedures performed in Taiwan in the past decade.9
A major concern after vertebral augmentation in patients with osteoporosis is the occurrence of new VCFs in the untreated vertebral bodies. Some authors believe that new VCFs after vertebral augmentation are caused by augmented stiffness of the treated vertebrae related to the amount of injected cement,10,11 load transfer,12–14 and cement leakage into the adjacent vertebral disc space.15 It also has been proposed that these new VCFs result from the natural course of osteoporosis.16–19 Some medications, such as corticosteroids, can disrupt skeletal architecture and result in an increase of VCFs.20,21
New VCFs are a potential late sequela of vertebral augmentation that can bring new back pain, induce disability, and decrease patient satisfaction after the procedure. The incidence of new VCFs has been reported as 12.2%–52%.18,19,22 Symptomatic VCFs are common post–vertebral augmentation; subsequent vertebral augmentation procedures are usually performed for prompt pain relief.
The present study used nationwide data to estimate the incidence of subsequent vertebral augmentation for new VCFs in patients with previous vertebral augmentation. In addition, this study provides insight into risk factors for repeat vertebral augmentation in patients with previous vertebral augmentation.
Materials and methods
Database
The National Health Insurance Research Database (NHIRD) included all claims data from Taiwan’s National Health Insurance program. This study was exempted from full review by the Institutional Review Board because the NHIRD consisted of deidentified secondary data released to the public for research purposes. There are approximately 23 million individuals in this registry.
Study sample
From January 1, 2004 to December 31, 2007, all patients undergoing vertebral augmentations were identified from the NHIRD for analysis. All subjects who suffered VCFs and underwent vertebral augmentation were individually identified and followed longitudinally until the end of the study period (December 31, 2010) or death. The follow-up for these patients was censored only at the occurrence of death or at the end of the study period.
Vertebral augmentation for VCF
Diagnosis at every admission was recorded in the NHIRD, according to the International Classification of Disease, 9th Revision Clinical Modification (ICD-9-CM). Any patient whose hospitalization discharge had the diagnostic code of VCF (805.xx) combined with procedures coded for vertebral augmentation (33126B, for the first vertebra, or 33127B, for any vertebra after the first level) was considered to have undergone vertebral augmentation during the hospitalization.
Subsequent vertebral augmentation for new VCF
New VCFs resulting in subsequent procedures were defined as rehospitalization for similar diagnostic and procedure codes. These patients were identified as having undergone subsequent vertebral augmentation procedures for new VCFs.
Exclusion criteria
We excluded patients who were rehospitalized without surgical procedures codes. Often these hospitalizations may have been due to comorbidities related to VCFs. Patients who had preexisting vertebral augmentations prior to 2004 were excluded. Vertebral augmentation for metastatic spine tumor (ICD-9-CM diagnosis code 198.5) or multiple myeloma (203.0) was excluded from analysis. Patients with multiple trauma (ICD-9-CM codes 484–487) and patients who died within the date of admission were excluded.
Covariates
Age, sex, and comorbidities were included for analysis. Comorbidities were identified by diagnostic codes between 3 months before and 3 months after the date of vertebral augmentation procedures. The ICD-9-CM diagnosis codes were as follows: 250.00–250.93 for diabetes mellitus (DM); 401.x-404.x for hypertension and its complications; 272.0, 272.1, 272.2, and 272.4 for hyperlipidemia; 362.34, and 430.x–438.x for cerebrovascular disease; 410.xx–414.xx for coronary heart disease; 410.x and 412.x for myocardial infarction; 440.x–447.x for peripheral vascular disease; 491.x–493.x for chronic respiratory disease; 711.xx, 712.xx, 713.x, 714.xx, 716.xx–719.xx for arthritis and other arthropathies; 580.x–588.x for chronic renal insufficiency; 290.x, 291.x, and 294.x for dementia; 369.xx for blindness and low vision; and 733.0x for osteoporosis.
Medication exposure
Medication exposure was described in terms of proportions of patients who received at least two prescriptions from the various medication classes recommended for osteoporosis and VCF-related problems during the time period 3 months prior to vertebral augmentation and follow-up (3 months after the augmentations). The medication classes examined in this study included: calcium/vitamin D, bisphosphonates, hormone replacement therapy, selective estrogen receptor modulators, calcitonin, corticosteroids, paracetamol, nonsteroidal anti-inflammatory drugs (NSAIDs), antidepressants, stimulants, antipsychotics, mood stabilizers, and anxiolytics.
Statistical analysis
Chi-square and independent t-tests were used to assess differences in age, sex, comorbidities, and medication exposure between patients who had had a repeat procedure and those who had not. The repeat-procedure-free rates were estimated by the Kaplan–Meier method. Stratified Cox proportional hazard regressions were performed to compare age, sex, comorbidities, and medication exposure between repeat-procedure and repeat-procedure-free groups. All statistical analyses were conducted using the SAS statistical package (SAS System for Windows, V.9.2; SAS Institute Inc, Cary, NC, USA). A value of P<0.05 was considered statistically significant.
Results
Incidence and basic characteristics
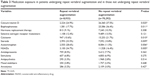
From January 1, 2004 to December 31, 2007, 79,225 patients aged 45 years or older underwent vertebral augmentation procedures using the aforementioned inclusion and exclusion criteria. Table 1 shows that the number of vertebral augmentations from 2004 to 2007 in Taiwan. Among the 79,225 patients, 8,933 (11.3%) underwent a subsequent vertebral augmentation during follow-up until 2010 (Figure 1). The average interval to a subsequent procedure was 32.76±18.48 months. Tables 2 and 3 list the baseline demographic characteristics, medication exposure, and comorbidities of the patients. Table 4 shows the results of univariate and multivariate analyses of the potential risk factors for a repeat vertebral augmentation.
  | Table 1 Total 79,225 patients undergoing first vertebral augmentation |
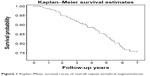  | Figure 1 Kaplan–Meier survival curve of overall repeat vertebral augmentations. |
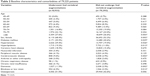  | Table 2 Baseline characteristics and comorbidities of 79,225 patients |
Influence of age and sex on subsequent vertebral augmentation
The incidence of repeat procedure varied with age and sex in this observation. The frequency with which patients underwent a second procedure was particularly high in patients ≥80 years of age (Table 2 and Figure 2). In other age groups, the frequency of a second procedure was about 8.0% to 10.9%. Among 42,802 female patients, 6,110 (14.3%) had repeat vertebral augmentation. Only 2,823 of 33,600 male patients (8.4%) had a repeat procedure. Thus, female patients had a higher frequency of repeat procedures, confirmed by multivariate Cox regression analysis showing that female patients were more likely to undergo repeat vertebral augmentations than were male patients (P=0.008; adjusted odds ratio [AOR]=1.24; 95% confidence interval [CI]: 1.10–2.36). Old age (≥80 years) was also a predisposing factor for repeat vertebral augmentation (P=0.011; AOR=1.60; 95% CI: 1.31–2.08).
  | Figure 2 The frequency with which patients underwent a second procedure was particularly high in patients ≥80 years of age. |
Comorbidities
Comorbidities in patients who underwent repeat vertebral augmentation and in those who did not are shown in Tables 2–4. Coronary heart disease, myocardial infarction, peripheral vascular disease, arthritis and other arthropathies, chronic respiratory disease, chronic renal insufficiency, and osteoporosis were similar between the two groups; however, DM (P=0.001; AOR=4.31; 95% CI: 4.05–5.88), cerebrovascular disease (P=0.003; AOR=4.09; 95% CI: 3.44–5.76), dementia (P=0.002; AOR=1.97; 95% CI: 1.69–2.33), blindness and low vision (P=0.002; AOR=3.72; 95% CI: 2.32–3.95), hypertension (P=0.009; AOR=2.58; 95% CI: 2.35–3.47), and hyperlipidemia (P=0.015; AOR=2.09; 95% CI: 1.67–2.22) were more common in those patients who underwent repeat vertebral augmentation.
Medication exposure
Medication exposure in patients who underwent repeat vertebral augmentation and in those who did not is shown in Tables 3 and 4. Among the medications used to treat or prevent osteoporosis, calcium/vitamin D (P=0.008; AOR=2.98; 95% CI: 1.83–3.93), bisphosphonates (P=0.016; AOR=2.11; 95% CI: 1.26–2.61), and calcitonin (P=0.017; AOR=4.59; 95% CI: 3.40–5.77) were associated with patients not having repeat vertebral augmentation; however, steroids (P=0.009; AOR=7.28; 95% CI: 6.32–8.08), acetaminophen (P=0.006; AOR=3.54; 95% CI: 2.75–4.83), and NSAIDs (P=0.005; AOR=6.14; 95% CI: 5.08–7.41) were associated with patients having repeat vertebral augmentation. Hormone replacement therapy and selective estrogen receptor modulators did not decrease the incidence of repeat vertebral augmentation.
Discussion
Vertebral augmentation is a minimally invasive method of pain relief for VCFs. There has been a significant increase in the number of vertebral augmentation procedures performed in recent years, as shown in Table 1. Overall, 11.3% of patients who had vertebral augmentation underwent a repeat vertebral augmentation because of symptomatic VCFs during the follow-up until the end of 2010. The rate of repeat vertebral augmentation was lower than the rate of reported subsequent VCFs (12.2%–52%).18–20 The authors did not identify subsequent VCFs because this was difficult to estimate in the database. It is likely that some patients with subsequent VCFs received conservative treatment only. Some VCFs can remain asymptomatic and are detected incidentally when a patient undergoes a radiograph for unrelated conditions;2 some authors believe that only one-third of patients with osteoporotic VCFs seek medical attention for back pain symptoms.2,3
Very elderly patients (≥80 years old) were more likely to undergo a repeat vertebral augmentation (15.2%) than were those patients in other age groups (8.0%–10.9%). This observation may have been due to osteoporosis, associated comorbidities, and propensity to fall,23 although this current study did not demonstrate osteoporosis as a risk factor of repeat vertebral augmentation. One possible reason is that many patients did not have bone mineral density (BMD) measurement. Osteoporosis is defined by the World Health Organization (WHO) as a BMD of 2.5 standard deviations or more below the mean peak bone mass (average of young, healthy adults) as measured by dual-energy X-ray absorptiometry. Osteoporosis is likely to have been underestimated in our population-based database. Our results also demonstrate female patients were more likely to have a repeat vertebral augmentation. This is supported by two cadaver studies.24,25
The present study demonstrates that patients with cerebrovascular disease had a higher incidence of repeat vertebral augmentation. The reasons for the association between repeat vertebral augmentation and cerebrovascular diseases are unclear. Similar to our results, patients with cerebrovascular disease have increased risk of hip fracture because of their high incidence of falls and loss of bone mass.26 Osteoporosis is a significant complication of cerebrovascular disease, and these patients may also have motor, sensory, and visual/perceptual deficits that predispose them to falls. Although both cerebrovascular diseases and osteoporosis are common health problems among the elderly, little attention has been paid in the literature to their correlation.27
DM has been shown to be significantly associated with vertebral fractures.28–31 Patients with DM are at greater risk of vertebral fractures, not only due to extraskeletal factors, such as predisposition to falls but also, because of alteration of bone quality and reduction of bone strength.28–31 Recent studies have found that patients with DM had an increased risk of vertebral fractures independent of BMD or complications of DM.30,31 Therefore, these patients have a higher incidence of repeat vertebral augmentation.
Dementia and blindness and low vision were also highly associated with repeat vertebral augmentation. Their association has rarely been reported. One possible explanation is susceptibility to falls in patients with dementia and low vision.32
Antiosteoporotic agents had significant efficacy in increasing lumbar spine BMD and reduction in the occurrence of any new vertebral fractures.33 This study demonstrates that patients who were prescribed calcium/vitamin D, bisphosphonates, and calcitonin had a lower rate of repeat vertebral augmentation; however, hormone replacement therapy and selective estrogen receptor modulators did not decrease the rate of repeat procedures in this study. The exact reason for this observation is unknown. We found that hormone replacement therapy and selective estrogen receptor modulators are used less frequently in Taiwan (Table 2), and we surmise that these treatments could not show a significant antiosteoporotic effect in our study.
Patients on corticosteroids therapy had a higher rate of repeat vertebral augmentation. Corticosteroid therapy is associated with increased risk of vertebral fracture. Others authors also reported that patients on corticosteroid therapy at the time of their initial vertebral augmentation were almost twice as likely to have symptomatic refractures than were patients not taking corticosteroids.21 Loss of trabecular bone in patients on corticosteroid therapy may contribute to increased risk of VCFs. NSAIDs and acetaminophen were also associated with a higher rate of repeat procedures in the present study. Some authors have reported that NSAIDs and acetaminophen were associated with a higher fracture rate.34–36 The increase in fracture risk may stem from changes in postural balance or an increased risk of accidents because of dizziness (a side effect of NSAIDs).34
This study has some limitations. We did not investigate the incidence of VCFs because the true rate of new VCFs is difficult to estimate. Some VCFs can remain asymptomatic,2,3 and not all patients with new VCFs seek medication or undergo vertebral augmentation. Patients who undergo repeat vertebral augmentations probably have severe and prolonged back pain without response to conservative treatment. Some risk factors for refracture cannot be evaluated in the present study. It is impossible to look into the details of each operative note to clarify the cement volume, procedure style (vertebroplasty vs kyphoplasty), mechanical factors (location of the fracture, restoration of vertebral body height, and sagittal balance), surgical complications, or how many and which levels were treated in each vertebral augmentation, in such a large database study. The NHIRD data does not include details of operative notes and radiographic reports. Likewise, the degree of osteoporosis affecting each patient was not included in the data; however, the present study is the first to demonstrate the actual repeat vertebral augmentation rate in a large cohort of patients (79,225). The study provides a different viewpoint for looking at risk factors for repeat vertebral augmentation. It can be helpful in the estimation and prevention of repeat vertebral augmentation.
Conclusion
A total of 11.3% of patients underwent repeat vertebral augmentation during the follow-up. Female sex, advanced age (≥80 years), cerebrovascular disease, DM, hypertension, hyperlipidemia, dementia, and low vision/blindness were characteristics associated with repeat vertebral augmentation. Calcium/vitamin D, bisphosphonates, and calcitonin were associated with a lower rate of repeat vertebral augmentation. Steroids, acetaminophen, and NSAIDs were associated with an increase in the rate of repeat vertebral augmentation. The authors identify high-risk patients, encourage the use of antiosteoporotic drugs for high-risk patients, and advocate fall prevention and avoidance of steroids and NSAIDs.
Disclosure
The authors report no conflicts of interest in this work.
References
Kado DM, Browner WS, Palermo L, Nevitt MC, Genant HK, Cummings SR. Vertebral fractures and mortality in older women: a prospective study. Study of Osteoporotic Fractures Research Group. Arch Intern Med. 1999;159(11):1215–1220. | ||
Center JR, Nguyen TV, Schneider D, Sambrook PN, Eisman JA. Mortality after all major types of osteoporotic fracture in men and women: an observational study. Lancet. 1999;353(9156):878–882. | ||
Klazen CA, Lohle PN, de Vries J, et al. Vertebroplasty versus conservative treatment in acute osteoporotic vertebral compression fractures (Vertos II): an open-label randomised trial. Lancet. 2010;376(9746):1085–1092. | ||
Tamayo-Orozco J, Arzac-Palumbo P, Peón-Vidales H, Mota-Bolfeta R, Fuentes F. Vertebral fracture associated with osteoporosis: patient management. Am J Med. 1997;103(2A):44S–48S; discussion 48S–50S. | ||
Voormolen MH, Lohle PN, Lampmann LE, et al. Prospective clinical follow-up after percutaneous vertebroplasty in patients with painful osteoporotic vertebral compression fractures. J Vasc Interv Radiol. 2006;17(8):1313–1320. | ||
Wang HK, Lu K, Liang CL, et al. Comparing clinical outcomes following percutaneous vertebroplasty with conservative therapy for acute osteoporotic vertebral compression fractures. Pain Med. 2010;11(11):1659–1665. | ||
Kallmes DF, Comstock BA, Heagerty PJ, et al. A randomized controlled trial of vertebroplasty for osteoporotic spine fractures. N Engl J Med. 2009;361(6):569–579. | ||
Buchbinder R, Osborne RH, Ebeling PR, et al. A randomized trial of vertebroplasty for painful osteoporotic vertebral fractures. N Engl J Med. 2009;361(6):557–568. | ||
Tsai YW, Hsiao FY, Wen YW, et al. Clinical outcomes of vertebroplasty or kyphoplasty for patients with vertebral compression fractures: a nationwide cohort study. J Am Med Dir Assoc. 2013;14(1):41–47. | ||
Liebschner MA, Rosenberg WS, Keaveny TM. Effects of bone cement volume and distribution on vertebral stiffness after vertebroplasty. Spine (Phila Pa 1976). 2001;26(14):1547–1554. | ||
Belkoff SM, Mathis JM, Jasper LE, Deramond H. The biomechanics of vertebroplasty. The effect of cement volume on mechanical behavior. Spine (Phila Pa 1976). 2001;26(14):1537–1541. | ||
Polikeit A, Nolte LP, Ferguson SJ. The effect of cement augmentation on the load transfer in an osteoporotic functional spinal unit: finite-element analysis. Spine (Phila Pa 1976). 2003;28(10):991–996. | ||
Baroud G, Nemes J, Heini P, Steffen T. Load shift of the intervertebral disc after a vertebroplasty: a finite-element study. Eur Spine J. 2003;12(4):421–426. | ||
Berlemann U, Ferguson SJ, Nolte LP, Heini PF. Adjacent vertebral failure after vertebroplasty. A biomechanical investigation. J Bone Joint Surg Br. 2002;84(5):748–752. | ||
Lin EP, Ekholm S, Hiwatashi A, Westesson PL. Vertebroplasty: cement leakage into the disc increases the risk of new fracture of adjacent vertebral body. AJNR Am J Neuroradiol. 2004;25(2):175–180. | ||
Grados F, Depriester C, Cayrolle G, Hardy N, Deramond H, Fardellone P. Long-term observations of vertebral osteoporotic fractures treated by percutaneous vertebroplasty. Rheumatology (Oxford). 2000;39(12):1410–1414. | ||
Pérez-Higueras A, Alvarez L, Rossi RE, Quiñones D, Al-Assir I. Percutaneous vertebroplasty: long-term clinical and radiological outcome. Neuroradiology. 2002;44(11):950–954. | ||
Uppin AA, Hirsch JA, Centenera LV, Pfiefer BA, Pazianos AG, Choi IS. Occurrence of new vertebral body fracture after percutaneous vertebroplasty in patients with osteoporosis. Radiology. 2003;226(1):119–124. | ||
Lu K, Liang CL, Hsieh CH, Tsai YD, Chen HJ, Liliang PC. Risk factors of subsequent vertebral compression fractures after vertebroplasty. Pain Med. 2012;13(3):376–382. | ||
Mandel S, Schilling J, Peterson E, Rao DS, Sanders W. A retrospective analysis of vertebral body fractures following epidural steroid injections. J Bone Joint Surg Am. 2013;95(11):961–964. | ||
Syed MI, Patel NA, Jan S, Shaikh A, Grunden B, Morar K. Symptomatic refractures after vertebroplasty in patients with steroid-induced osteoporosis. AJNR Am J Neuroradiol. 2006;27(9):1938–1943. | ||
Li YA, Lin CL, Chang MC, Liu CL, Chen TH, Lai SC. Subsequent vertebral fracture after vertebroplasty: incidence and analysis of risk factors. Spine (Phila Pa 1976). 2012;37(3):179–183. | ||
Yiannopoulou KG, Anastasiou IP, Ganetsos TK, Efthimiopoulos P, Papageorgiou SG. Prevalence of dementia in elderly patients with hip fracture. Hip Int. 2012;22(2):209–213. | ||
Nagaraja S, Awada HK, Dreher ML, Gupta S, Miller SW. Vertebroplasty increases compression of adjacent IVDs and vertebrae in osteoporotic spines. Spine J. 2013;13(12):1872–1880. | ||
Nagaraja S, Awada HK, Dreher ML, Bouck JT, Gupta S. Effects of vertebroplasty on endplate subsidence in elderly female spines. J Neurosurg Spine. Epub 2014 Dec 19. | ||
Ramnemark A, Nilsson M, Borssén B, Gustafson Y. Stroke, a major and increasing risk factor for femoral neck fracture. Stroke. 2000;31(7):1572–1577. | ||
Chen YC, Wu JC, Liu L, et al. Hospitalized osteoporotic vertebral fracture increases the risk of stroke: a population-based cohort study. J Bone Miner Res. 2013;28(3):516–523. | ||
Gonnelli S, Caffarelli C, Giordano N, Nuti R. The prevention of fragility fractures in diabetic patients. Aging Clin Exp Res. Epub 2014 Jul 25. | ||
Chung DJ, Choi HJ, Chung YS, Lim SK, Yang SO, Shin CS. The prevalence and risk factors of vertebral fractures in Korean patients with type 2 diabetes. J Bone Miner Metab. 2013;31(2):161–168. | ||
Kilpadi KL, Eldabaje R, Schmitz JE, et al. Type 2 diabetes is associated with vertebral fractures in a sample of clinic- and hospital-based Latinos. J Immigr Minor Health. 2014;16(3):440–449. | ||
Yamamoto M, Yamaguchi T, Yamauchi M, Kaji H, Sugimoto T. Diabetic patients have an increased risk of vertebral fractures independent of BMD or diabetic complications. J Bone Miner Res. 2009;24(4):702–709. | ||
Old JL, Calvert M. Vertebral compression fractures in the elderly. Am Fam Physician. 2004;69(1):111–116. | ||
Cheng MH, Chen JF, Fuh JL, Lee WL, Wang PH. Osteoporosis treatment in postmenopausal women with pre-existing fracture. Taiwan J Obstet Gynecol. 2012;51(2):153–166. | ||
Geusens P, Emans PJ, de Jong JJ, van den Bergh J. NSAIDs and fracture healing. Curr Opin Rheumatol. 2013;25(4):524–531. | ||
Vestergaard P, Rejnmark L, Mosekilde L. Fracture risk associated with use of nonsteroidal anti-inflammatory drugs, acetylsalicylic acid, and acetaminophen and the effects of rheumatoid arthritis and osteoarthritis. Calcif Tissue Int. 2006;79(2):84–94. | ||
Vestergaard P, Hermann P, Jensen JE, Eiken P, Mosekilde L. Effects of paracetamol, non-steroidal anti-inflammatory drugs, acetylsalicylic acid, and opioids on bone mineral density and risk of fracture: results of the Danish Osteoporosis Prevention Study (DOPS). Osteoporos Int. 2012;23(4):1255–1265. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.