Back to Journals » Clinical Ophthalmology » Volume 8
Plasma homocysteine and genetic variants of homocysteine metabolism enzymes in patients from central Greece with primary open-angle glaucoma and pseudoexfoliation glaucoma
Authors Zacharaki F, Hadjigeorgiou G, Koliakos G, Morrison M, Tsezou A, Chatzoulis D, Almpanidou P, Topouridou K, Karabatsas C, Pefkianaki M, DeAngelis M, Tsironi EE
Received 26 March 2014
Accepted for publication 16 April 2014
Published 11 September 2014 Volume 2014:8 Pages 1819—1825
DOI https://doi.org/10.2147/OPTH.S64904
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Fani Zacharaki,1 Georgios M Hadjigeorgiou,2 Georgios G Koliakos,3 Margaux A Morrison,4 Aspasia Tsezou,5 Dimitrios Z Chatzoulis,1 Pavlina Almpanidou,1 Konstantina Topouridou,3 Constantinos H Karabatsas,1 Maria Pefkianaki,1 Margaret M DeAngelis,4 Evangelia E Tsironi1
1Department of Ophthalmology, 2Department of Neurology, Faculty of Medicine, University of Thessaly, Larissa, 3Department of Biochemistry, Medical School, Aristotles University of Thessaloniki, Thessaloniki, Greece; 4Department of Ophthalmology and Visual Sciences, John A Moran Eye Center, University of Utah, Salt Lake City, UT, USA; 5Department of Biology, Faculty of Medicine, University of Thessaly, Larissa, Greece
Background: The purpose of this study was to investigate plasma homocysteine levels and polymorphisms in genes encoding enzymes in the metabolic pathway of homocysteine in association with primary open-angle glaucoma (POAG) and pseudoexfoliation glaucoma (PXFG).
Methods: A total of 156 glaucoma patients (76 with POAG and 80 with PXFG) and 135 controls matched for age and sex were enrolled in this study. Plasma homocysteine levels were measured using a commercially available enzyme-linked immunosorbent assay kit. DNA was extracted from peripheral blood leukocytes and real-time polymerase chain reaction was performed for genotyping of the samples. Patients were genotyped using predesigned TaqMan® single nucleotide polymorphism genotyping assays for two exon variations (rs1801131, rs1801133) in the 5,10-methylenetetrahydrofolate reductase (MTHFR) gene and one intron variation (rs8006686) in the methylenetetrahydrofolate dehydrogenase (MTHFD1) gene.
Results: Homocysteine levels were slightly higher in the patient group (POAG and PXFG) compared with controls, but the difference did not reach statistical significance. The minor alleles of the MTHFR single nucleotide polymorphisms showed a protective effect for POAG and showed an increased risk for PXFG, but none of these associations reached statistical significance (P>0.05). The minor allele of MTHFD1 rs8006686 showed a trend for increased risk of both POAG and PXFG (P>0.05). No statistically significant interaction was seen between the genetic variants and homocysteine levels (P>0.05).
Conclusion: Our results show that neither the examined single nucleotide polymorphisms from genes involved in the pathway of homocysteine metabolism nor the measured homocysteine levels were associated with POAG or PXFG in our study cohort.
Keywords: homocysteine, glaucoma, polymorphisms
Introduction
The open angle glaucomas are chronic and progressive optic neuropathies, which have in common characteristic morphological changes at the optic nerve head and retinal nerve fiber layer in the absence of other ocular disease or congenital anomalies. Progressive retinal ganglion cell death and visual field loss are associated with these findings.1 Primary open-angle glaucoma (POAG) is the most common type of glaucoma. Intraocular pressure and other currently unknown factors contribute to the optic nerve damage. There is increasing evidence that anatomic or functional abnormalities of the optic nerve head vessels compromising the microcirculation and perfusion might play a role in the pathogenesis of the disease.2–4
Pseudoexfoliation is an age-related ocular clinical entity, and is strongly associated with development of glaucoma (pseudoexfoliation glaucoma [PXFG]).5 It is characterized by accumulation of fibrinous, flake-shaped material in ocular tissues, especially in the anterior chamber of the eye. Higher intraocular pressure and the presence of disc hemorrhages were reported to be independent risk factors for progression of PXFG.6 With the use of electron microscopy methods, several investigators have detected exfoliation material in the extraocular tissue as well, suggesting that exfoliation might be the ocular manifestation of a systemic disorder.7,8 A number of systemic vascular disorders, including stroke, acute myocardial infarction, and aneurysms of the abdominal aorta were found to be associated with ocular exfoliation.9,10
Hyperhomocysteinemia is a known risk factor for vascular disease, including brain and heart infarction,11,12 as well as retinal vascular occlusions.13–15 Based on the hypothesis that vascular dysfunction is one of the factors involved in the pathogenesis of glaucoma,2–4,16 homocysteine was studied in several POAG and PXFG cohorts. Increased serum and tear homocysteine levels were found to be present in patients with POAG.17,18 Elevated plasma homocysteine levels have also been found in patients with PXFG,19,20 and these findings were recently confirmed by two published meta-analyses.21,22 The genetic component of circulating homocysteine involves single nucleotide polymorphisms on five genes, ie, methylenetetrahydrofolate reductase (MTHFR), methionine synthase, methionine synthase reductase, methylenetetrahydrofolate dehydrogenase (MTHFD1), and cystathionine β-synthase, encoding enzymes within the pathway of homocysteine metabolism on chromosomes 1, 5, 14, and 21. Some of these single nucleotide polymorphisms have been studied in connection with glaucoma, but none has been shown to have a statistically significant correlation.23–26 Two of the genetic variants (rs1801133 and rs1801131) are located in two exons of the MTHFR gene on chromosome 1. rs1801133 is a C>T missense variation, leading to increased thermolability and reduced activity of the MTHFR enzyme and rs1801131 is an A>C missense variation on the same gene.27 rs8006686 is an intron T>C polymorphism of the MTHFD1 enzyme gene on chromosome 14. In a study by Fan et al the rs8006686 polymorphism showed a marginally significant association with PXFG, but this finding was not stable after correction for multiple comparisons.23
Materials and methods
This was a prospective, case-control association study that assessed plasma homocysteine levels and genetic variants of homocysteine metabolism enzymes in a cohort of Greek patients with either POAG or PXFG as compared with controls. In order to determine the impact of homocysteine on the pathogenesis of glaucoma, three single nucleotide polymorphisms from two genes involved in the pathway of homocysteine metabolism were genotyped and homocysteine levels were measured.
In total, 156 patients (76 with POAG and 80 with PXFG) from the glaucoma clinic at the University Hospital of Larissa, Greece, were enrolled in the study. The control group consisted of 135 individuals from the cataract clinic of the same hospital. All subjects were unrelated. The study was approved by the local ethics committee and carried out in accordance with the Declaration of Helsinki. All subjects were of Greek nationality and from the same geographic region (central Greece), and had signed their informed consent before entering the study.
All patients underwent a complete ophthalmological examination, including anterior and posterior segment evaluation. The corneal endothelium, iris, iris margins, and the anterior lens surface were evaluated for exfoliative material before and after dilation. Intraocular pressure was measured using a Goldmann applanation tonometer (Haag-Streit, Koeniz-Berne, Switzerland). Gonioscopy was performed to evaluate the depth of the anterior chamber angle and the presence of pseudoexfoliative material and/or hyperpigmentation. Dilated funduscopic examination was performed to evaluate the optic nerve for typical glaucomatous changes. Visual field examination was performed using the 24-2 setting of the Humphrey Field Analyzer automated perimeter and the Swedish Interactive Threshold Algorithm.
Inclusion criteria for POAG patients were intraocular pressure over 22 mmHg on at least two measurements, an open anterior chamber angle determined with gonioscopy, and visual field and optic nerve changes consistent with glaucoma. Presence of exfoliation material in the anterior chamber, together with glaucoma criteria, established the diagnosis of PXFG. Control subjects had no evidence of exfoliative material at the anterior lens capsule or pupillary margin, and had intraocular pressure of less than 22 mmHg. Control subjects had normal visual fields, an open anterior chamber angle, no evidence of glaucomatous changes in the optic disc, and no history of glaucoma or ocular hypertension in first-degree relatives. Subjects with pseudoexfoliation syndrome (with or without ocular hypertension) or ocular hypertension were excluded from the study. The nutritional status of both patients and controls was assessed using the Subjective Global Nutritional Assessment test, according to Detsky et al.28 Only subjects classified as “well nourished” were included.
Individuals with systemic conditions known to influence homocysteine levels or using medications or nutritional supplements that interfere with homocysteine metabolism, such as renal disease, B12 malabsorption, high alcohol intake, methotrexate, phenytoin, carbamazepine, or fibrate therapy were excluded.29–31 Individuals with a history of bilateral cataract extraction, previous intraocular inflammation, or major ocular disease were also excluded.
Fasting plasma homocysteine levels were determined using a commercially available homocysteine enzyme immunoassay kit (Axis®; Axis-Shield, Dundee, UK), following the manufacturer’s instructions. Homocysteine levels were measured in μmol/L.
Genomic DNA was extracted from peripheral blood leukocytes using a commercially available DNA extraction kit (Qiagen, Valencia, CA, USA) according to the manufacturer’s standard protocol. Genotyping was performed using real-time polymerase chain reaction predesigned TaqMan® single nucleotide polymorphism genotyping assays (Applied Biosystems, Foster City, CA, USA). Patients were genotyped for three single nucleotide polymorphisms, ie, two exon MTHFR variations, 1298A>C (rs1801131) and 677C>T, (rs1801133), and one intron MTHFD1 variation (rs8006686).
Deviation from Hardy–Weinberg equilibrium was tested on each single nucleotide polymorphism using the chi-squared test in the unaffected population. Single nucleotide polymorphisms were tested for association using the minor allele, as defined by the allele occurring less frequently in the control subjects. Allelic and covariate associations with glaucoma were performed in SAS (version 9.1; Cary, NC, USA) using logistic regression. Age and homocysteine levels were tested for association with glaucoma as continuous variables while sex was tested as dichotomous. Separate analyses were performed assuming additive, dominant, and recessive genetic models for allelic association. Tests for interaction between the genetic variants and homocysteine levels were performed by adding an interaction term to the logistic regression model including both variables. Linkage disequilibrium (r2) between single nucleotide polymorphisms on the same chromosome was determined using the Haploview program (http://www.broad.mit.edu/mpg/haploview/).
Results
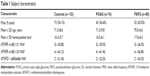
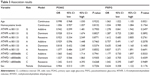
Data were available for 291 subjects. Of these, 76 had POAG and 80 had PXFG, and 135 were controls. Subject characteristics are shown in Table 1 and the genotype and allele frequencies in Table 2. All patients were Caucasian. The average age, proportion of males, and homocysteine levels were similar between the groups (Table 1) and showed no statistically significant differences (Table 3). Homocysteine levels were higher in patients as compared with controls, but were not significantly different, although there was a larger difference in homocysteine levels between PXFG and controls (1.1 μmol/L) than between POAG and controls (0.2 μmol/L). Increasing age was associated with an increased risk of PXFG (P=0.0021, Table 2). The two single nucleotide polymorphisms in the MTHFR gene (rs1801133 and rs1801131) and the one single nucleotide polymorphism in the MTHFD1 gene (rs8006686) were in Hardy–Weinberg equilibrium (data not shown). The single nucleotide polymorphisms in the MTHFR gene were not in high linkage disequilibrium among the controls (r2=0.34, Figure 1), and had identical linkage disequilibrium in each glaucoma subtype (data not shown). The minor alleles of the MTHFR single nucleotide polymorphisms were in a protective direction for POAG, whereas they showed an increased risk for PXFG, but none of these associations reached statistical significance (P>0.05, Table 2). The minor allele of MTHFD1, rs8006686, showed a trend of increased risk for both POAG and PXFG, but this was not statistically significant (P>0.05, Table 2). No statistically significant interaction was seen between the genetic variants and homocysteine levels (P>0.05, data not shown).
  | Figure 1 Linkage disequilibrium within MTHFR single nucleotide polymorphisms. |
Discussion
The association between plasma homocysteine levels and glaucoma remains inconsistent. In the present study, we did not find an association between single nucleotide polymorphisms 1298A>C (rs1801131) and 677C>T (rs1801133) in the MTHFR gene and one intron variation (rs8006686) in the MTHFD1 gene and POAG or PXFG. In addition, no significant difference in plasma homocysteine levels was observed between patients and controls. In accordance with our results, Turaçli et al found no significant association between homocysteine levels and pseudoexfoliation syndrome (PXFS) and PXFG in a cohort of Turkish patients.26 Interestingly, a recent study in a Pakistani population reported elevated homocysteine levels and a higher prevalence of the rs1801133 and rs1801131 polymorphisms in patients with primary angle-closure glaucoma, but not in those with POAG.25 On the other hand, a number of previous studies have reported that plasma homocysteine was elevated in patients with pseudoexfoliation with or without glaucoma. Two groups of investigators reported elevated plasma homocysteine levels in both POAG and PXFG patients when compared with controls.17,18,32,33 Similarly, plasma homocysteine levels were associated with PXFG and PXFS in a number of studies when compared with groups of patients with nonexfoliation or normal controls.19,34–37 The association between homocysteine levels and PXFG was confirmed by a very recent meta-analysis that included data from 14 studies (485 cases and 456 controls).22 Several other groups of investigators did not confirm the association between homocysteine and POAG.20,36,38,39 However, a meta-analysis by Xu et al reviewed the results of 12 studies investigating the relationship between homocysteine levels and POAG and concluded that POAG is associated with higher homocysteine levels.21
Regarding the genetic aspect of homocysteine metabolism, no study has found a significant association between single nucleotide polymorphisms in homocysteine metabolism genes and open-angle glaucoma,23–26 which is consistent with our results. However, it should be noted that most of the studies tested the rs1801133 polymorphism and only Fan et al included all 17 single nucleotide polymorphisms of the homocysteine metabolism genes.23
In addition to inherited disorders of the homocysteine metabolism enzymes, several known conditions can result in elevated homocysteine levels, including vitamin B6 and B12 or folic acid deficiency, renal disease, hypothyroidism, advanced age, and smoking. Different dietary habits or lifestyle due to cultural particularities might result in heterogeneous results among distinct ethnic groups. A detailed medical history was taken for both patients and controls, and the Subjective Global Nutritional Assessment test was used to minimize the potential impact of these factors on measured homocysteine values. However, no data were available for smoking status, weight, and physical activity levels, and this was one of the limitations of the study. Additionally, it would be reasonable to assume that variation in the laboratory methods used to determine plasma homocysteine levels might partly explain the inconsistent findings.39
Our study has all the limitations that apply to genetic association studies.40,41 The sample sizes required to predict association need to be far beyond what is currently available, and any single institution or entity alone would probably not be able to provide a reasonable number of patients. Collaborative studies with large cohorts of patients would be required to provide more power to detect significant relationships. Alternatively, consortia performing gene candidate or genome-wide association studies will be able to replicate the validity of the present findings.
Nevertheless, the present study fulfills the minimum requirements for an association study to be informative. These include controls matched for age and sex, a good scientific rationale, presence of Hardy–Weinberg equilibrium in genotypes, and a similar ethnic background.40 In our case, the study population constitutes a very homogeneous Caucasian cohort, as all subjects originate from the central part of our country. In addition, because our hospital is the only tertiary institution covering a rural and urban region with nearly one million inhabitants, and more severe patients are usually referred to us, we cannot exclude the possibility of selection bias.
Conclusion
Neither single nucleotide polymorphisms in the genes involved in the pathway of homocysteine metabolism nor measured homocysteine levels were shown to be associated with either POAG or PFXG in this study cohort.
Acknowledgments
This work was supported by an unrestricted grant from Research to Prevent Blindness, Inc, New York, NY, USA, to the Department of Ophthalmology and Visual Sciences, University of Utah, UT, USA, and a grant (code 2989) from the Research Committee, University of Thessaly, Greece.
Disclosure
The authors declare that they have no commercial interest in the subject of this paper or in entities discussed therein to disclose. These data have not been presented previously. The authors report no conflict of interest in this work.
References
European Glaucoma Society. Terminology and Guidelines for Glaucoma. 3rd ed. 2008. Available from: http://www.eugs.org/eng/EGS_guidelines.asp. Accessed May 27, 2014. | ||
Flammer J. The vascular concept in glaucoma. Surv Ophthalmol. 1994; 38 Suppl:S3–S6. | ||
Flammer J, Orgül S, Costa VP, et al. The impact of ocular blood flow in glaucoma. Prog Retin Eye Res. 2002;21:359–393. | ||
Hayreh SS. Blood flow in the optic nerve head and factors that may influence it. Prog Retin Eye Res. 2001;20:595–624. | ||
Mitchel P, Wang J, Hourihan F. The relationship between glaucoma and pseudoexfoliation. The Blue Mountains Eye Study. Arch Ophthalmol. 1999;117:1319–1324. | ||
Holló G, Quaranta L, Cvenkel B, et al. Risk factors associated with progression in exfoliative glaucoma patients. Ophthalmic Res. 2012;47: 208–213. | ||
Amari F, Umihira J, Nohara M, et al. Electron microscopic immunohistochemistry of ocular and extraocular pseudoexfoliative material. Exp Eye Res. 1997;65:51–56. | ||
Schlötzer-Schrehardt UM, Koca MR, Naumann GO, Volkholz H. Pseudoexfoliation syndrome. Ocular manifestation of a systemic disorder? Arch Ophthalmol. 1992;110:1952–1956. | ||
Mitchell P, Wang JJ, Smith W. Association of pseudoexfoliation syndrome with increased vascular risk. Am J Ophthalmol. 1997;124: 685–687. | ||
Shrum KR, Hattenhauer MG, Hodge D. Cardiovascular and cerebrovascular mortality associated with ocular pseudoexfoliation. Am J Ophthalmol. 2000;129:83–86. | ||
McQuillan BM, Beilby JP, Nidorf M, Thompson PL, Hung J. Hyperhomocysteinemia but not the C677T mutation of methylenetetrahydrofolate reductase is an independent risk determinant of carotid wall thickening. The Perth Carotid Ultrasound Disease Assessment Study. Circulation. 1999;99:2383–2388. | ||
Wald D, Law M, Morris JK. Homocysteine and cardiovascular disease: evidence on casualty from meta-analysis. BMJ. 2002;325:1202–1208. | ||
Pianka P, Almog Y, Man O, Goldstein M, Sela B, Loewenstein A. Hyperhomocysteinemia in patients with nonarteritic anterior ischemic optic neuropathy, central retinal artery occlusion and central retinal vein occlusion. Ophthalmology. 2000;107:1588–1592. | ||
Weger M, Stanger O, Deutschmann H, et al. Hyperhomocyst(e)inaemia, but not C677T mutation, as a risk factor for non-arteritic ischaemic neuropathy. Br J Ophthalmol. 2001;85:803–808. | ||
Cahlil MT, Stinnett SS, Fekrat S. Meta-analysis of plasma homocysteine, serum folate, serum vitamin B12, and thermolabile MTHFR genotype as risk factors for retinal vascular occlusive disease. Am J Ophthalmol. 2003;136:1136–1150. | ||
Flammer J, Haefliger IO, Orgul S, Resink T. Vascular dysregulation: a principal risk factor for glaucomatous damage? J Glaucoma. 1999;8: 212–219. | ||
Bleich S, Jünemann A, von Ahsen N, et al. Homocysteine and risk of open-angle glaucoma. J Neural Transm. 2002;109:1499–1504. | ||
Roedl JB, Bleich S, Reulbach U, et al. Homocysteine levels in aqueous humor and plasma of patients with primary open-angle glaucoma. J Neural Transm. 2007;114:445–450. | ||
Leibovitch I, Kurtz S, Shemesh G, et al. Hyperhomocystinemia in pseudoexfoliation glaucoma. J Glaucoma. 2003;12:36–39. | ||
Tranchina L, Centofanti M, Oddone F, et al. Levels of plasma homocysteine in pseudoexfoliation glaucoma. Graefes Arch Clin Exp Ophthalmol. 2011;249:443–448. | ||
Xu F, Zhao X, Zeng SM, Li L, Zhong HB, Li M. Homocysteine, B vitamins, methylene tetrahydrofolate reductase gene, and risk of primary open-angle glaucoma: a meta-analysis. Ophthalmology. 2012;119: 2493–2499. | ||
Xu F, Zhang L, Li M. Plasma homocysteine, serum folic acid, serum vitamin B12, serum vitamin B6, MTHFR and risk of pseudoexfoliation glaucoma: a meta-analysis. Graefes Arch Clin Exp Ophthalmol. 2012;250:1067–1074. | ||
Fan BJ, Chen T, Grosskreutz C, et al. Lack of association of polymorphisms in homocysteine metabolism genes with pseudoexfoliation syndrome and glaucoma. Mol Vis. 2008;14:2484–2491. | ||
Mossbock G, Weger M, Faschinger C, et al. Methylenetetrahydrofolate reductase (MTHFR) 677C>T polymorphism and open angle glaucoma. Mol Vis. 2006;12:356–359. | ||
Shazia M, Raheel Q, Farah A, Muhammad IK, Wajid AK, Asifa A. MTHFR gene C677T and A1298C polymorphisms and homocysteine levels in primary open angle and primary closed angle glaucoma. Mol Vis. 2009;15:2268–2278. | ||
Turaçli ME, Tekeli O, Özdemir F, Akar N. Methylenetetrahydrofolate reductase 677 C-T and homocysteine levels in Turkish patients with pseudoexfoliation. Clin Experiment Ophthalmol. 2005;33:505–508. | ||
Frosst P, Blom HJ, Milos R, et al. A candidate genetic risk factor for vascular disease: a common mutation in methylenetetrahydrofolate reductase. Nat Genet. 1995;10:111–113. | ||
Detsky AS, McLaughlin JR, Baker JP, et al. What is subjective global assessment of nutritional status? JPEN J Parenter Enteral Nutr. 1987; 11:8–13. | ||
Westphal S, Dierkes J, Luley C. Effects of fenofibrate and gemfibrozil on plasma homocysteine. Lancet. 2001;358:39–40. | ||
de Bree A, Verschuren WM, Blom HJ, Kromhout D. Lifestyle factors and plasma homocysteine concentrations in a general population sample. Am J Epidemiol. 2001;154:150–154. | ||
Brattstrom L, Lindgren A, Israelsson B, Anderson A, Hultberg B. Homocysteine and cysteine: determinants of plasma levels in middle-aged and elderly subjects. J Intern Med. 1994;236:633–641. | ||
Roedl JB, Bleich S, Reulbach U, et al. Vitamin deficiency and hyperhomocysteinemia in pseudoexfoliation glaucoma. J Neural Transm. 2007;114:571–575. | ||
Clement CI, Goldberg I, Healey PR, Graham SL. Plasma homocysteine, MTHFR gene mutation, and open-angle glaucoma. J Glaucoma. 2009;18:73–78. | ||
Vessani R, Ritch R, Liebmann J, Jofe M. Plasma homocysteine is elevates in patients with exfoliation syndrome. Am J Ophthalmol. 2003; 136:41–46. | ||
Puustjärvi T, Blomster H, Kontkanen M, Punnonen K, Teräsvirta M. Plasma and aqueous humour levels of homocysteine in exfoliation syndrome. Graefes Arch Clin Exp Ophthalmol. 2004;242:749–754. | ||
Altintaş Ö, Maral H, Yüksel N, Karabaş V, Dillioğlugil MÖ, Çağlar Y. Homocysteine and nitric oxide levels in plasma of patients with pseudoexfoliation syndrome, pseudoexfoliation glaucoma and primary open-angle glaucoma. Graefes Arch Clin Exp Ophthalmol. 2005;243: 677–683. | ||
Cumurcu T, Sahin S, Aydin E. Serum homocysteine, vitamin B12 and folic acid levels in different types of glaucoma. BMC Ophthalmol. 2006;6:6. | ||
Wang G, Medeiros FA, Barshop BA, Weinreb RN. Total plasma homocysteine and primary open-angle glaucoma. Am J Ophthalmol. 2004;137:401–406. | ||
Centers for Disease Control and Prevention. Assessment of laboratory tests for plasma homocysteine – selected laboratories, July–September 1998. MMWR Morb Mortal Wkly Rep. 1999;48:1013–1015. | ||
Cardon LR, Bell JI. Association study designs for complex diseases. Nat Rev Genet. 2001;2:91–99. | ||
Zintzaras E, Lau J. Trends in meta-analysis of genetic association studies. J Hum Genet. 2008;53:1–9. |
 © 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.