Back to Journals » Research Reports in Clinical Cardiology » Volume 6
Periprocedural myocardial infarction enhances the predictive value of inflammatory biomarkers for patients with obstructive coronary artery disease after implantation of drug-eluting stent
Authors Jesika A, Hu Z, Kan J , Chen S
Received 26 November 2014
Accepted for publication 8 January 2015
Published 18 February 2015 Volume 2015:6 Pages 17—28
DOI https://doi.org/10.2147/RRCC.S78173
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Richard Kones
Anastasia Jesika,1 Zuo-Ying Hu,2 Jing Kan,3 Shao-Liang Chen2
1Nanjing Medical University, Nanjing, People’s Republic of China; 2Department of Cardiology, Nanjing First Hospital, Nanjing Medical University, Nanjing, People’s Republic of China; 3Nanjing Heart Center, Nanjing, People’s Republic of China
Objective: The present study aims to clarify the long-term clinical importance of interleukin (IL)-6 in predicting major adverse cardiac events (MACE) for an entire cohort of patients with coronary artery disease after implantation of a drug-eluting stent (DES), and its interplay with periprocedural myocardial infarction (PMI).
Background: The correlation of proinflammatory biomarkers with occurrence of clinical events, including PMI and mortality, is controversial.
Methods: IL-6 was measured in 1,991 patients at admission. The participants were then assigned to two groups: IL-6 level ≥9 pg/mL and IL-6 level <9 pg/mL. The primary endpoint was the occurrence of cardiac death or myocardial infarction (MI) at year 3 after indexed percutaneous coronary intervention (PCI) procedure.
Results: The in-hospital rate of the primary endpoint in the IL-6 level ≥9 pg/mL group was 9.1%, statistically significantly different to 6.3% in the IL-6 <9 pg/mL group (P=0.026), mainly driven by the increased rate of MI (9.1% vs 6.1%, P=0.025). Those differences in MI/death and MI was sustained through to the 3-year follow-up (10.9% vs 7.6%, P=0.017 and 10.1% vs 7.5%, P=0.049). At the 3-year follow-up after the assigned procedure, more frequent MI was also the main reason for increased composite MACE between the IL-6 ≥9 pg/mL and IL-6 <9 pg/mL groups (20.7% vs 15.8%, P=0.007). In the IL-6 ≥9 pg/mL group, PMI was strongly correlated with mortality at 1-year through to the 3-year (hazard ratio: 2.96, 95% confidence interval: 1.35–6.49, P=0.005) follow-up after PCI procedure.
Conclusion: Elevated preprocedural serum IL-6 level was correlated with death, MI, and MACE after implantation of the DES. PMI enhances the predictive value of IL-6 for post-DES events.
Keywords: major adverse cardiac events, coronary heart disease, IL-6
Introduction
Percutaneous coronary intervention (PCI) using drug-eluting stents (DES) is associated with reduced restenosis and requirement of revascularization for patients with obstructive coronary disease.1 However, pooled data pointed toward delayed arterial endothelialization by DES, leading to late and very late thrombosis.2,3 Our group reported increased inflammatory biomarkers,4 including interleukin (IL)-6 and C-reactive protein (CRP), after implantation of a DES, in line with results by others.5,6 Unfortunately, controversy in terms of the correlation of proinflammatory biomarkers with the occurrence of clinical events has existed for a long time,4–6 mainly driven by disparities in study design.
Chen et al4 previously reported that IL-6, rather than CRP, predicted mortality and morbidity after DES PCI for patients with unstable angina who were not on statin treatment. However, the predictive value of IL-6 for the clinical outcome in patients overall or patients with stable angina receiving DES was not clearly addressed. Furthermore, a pool of clinical studies confirmed the stronger relationship of periprocedural myocardial infarction (PMI) with mortality,7–10 and there was no significant correlation with IL-6 or CRP.4,9 Accordingly, the present prospective analysis aimed to elucidate the long-term clinical importance of IL-6 in predicting the major adverse cardiac events (MACE) for an entire cohort of patients with coronary artery disease, and its interplay with PMI.
Methods
Patient population
Between February 2009 and February 2012, all patients who were assigned to PCI at our center were screened in the current analysis. Inclusion criteria were: patients with infarction, unstable angina, stable angina, or silent ischemia who underwent successful DES implantation. Patients with cardiogenic shock, prior bare metal stent (BMS) implantation, balloon angioplasty without DES, and congenital heart disease were excluded from the analysis. The study protocol was approved by the ethics committee. Informal consent was gained from all patients.
IL-6 and highly sensitive CRP measurement
Five milliliters of peripheral venous blood was drawn from the patients at admission. Plasma was separated by centrifugation at 2,000 × g for 5 minutes at room temperature. The serum specimens were then placed in heparin-containing tubes and stored at −80°C until analysis. Determination of the serum IL-6 level was done with a IL-6 test kit from Abcam plc (Cambridge, UK), while highly sensitive (hs)-CRP level was assessed with a test kit from Santa Cruz Biotechnology, Inc. (Dallas, TX, USA; microplate reader model DENLEY DRAGON Wellscan MK3, Thermo Fisher Scientific, Waltham, MA, USA); analysis was done by software from the Ascent software for Multiskan.
PCI procedure
Coronary angiography and PCI with stent implantation were performed through a transradial or transfemoral approach. Transradial procedures were performed by using standard hydrophilic-coated sheaths and hemostasis achieved immediately after the procedure by transradial band. Transfemoral procedures were performed using standard hydrophilic-coated sheaths and hemostasis achieved 4–6 hours after the procedure (when the patient achieve an activated clotting time [ACT] <180 seconds), mainly by manual compression. The use of intravascular ultrasound (IVUS) or the selection of DES (sirolimus- or paclitaxel-eluting stents) was totally dependent upon the experienced interventional cardiologist. The procedural success was defined as a final residual stenosis ≤30% by visual estimation with a thrombolysis in myocardial infarction (TIMI) flow grade 3 of the target vessel without death or Q-wave myocardial infarction (MI) or emergency reintervention or emergency bypass at the time of hospitalization. In most cases of PCI, the size and the length of stent were based on visual estimation of the lesion by the experienced interventional cardiologist, but in the case of IVUS-guided PCI, the size and the length of stent were selected according to IVUS measurement. In all the cases of PCI, overlapping stents were used if the lesion could not be covered by a single stent. We implanted the stent according to standard minimum overlap area covered between two stents. Once the stent implantation done, we used high-pressure noncompliant balloon, the size and diameter of which varies according to the size and diameter of the stent.
Medication
All patients were given a loading dose of 300 mg of both aspirin and clopidogrel at admission. Patients were maintained on aspirin 100 mg and clopidogrel 75 mg once daily after the PCI procedure. All patients were recommended to take aspirin 100 mg daily indefinitely and clopidogrel 75 mg per day was prescribed for at least 12 months. Statin therapy was also started upon admission, 20–40 mg of atorvastatin or 10–20 mg of rosuvastatin, and continued throughout the course of follow-up unless the termination of the therapy became necessary.
Endpoints and definition
The primary endpoint was the occurrence of cardiac death or MI at year 3 after the indexed PCI procedure. Cardiac death was diagnosed as any unexplained death unless a non-cardiac cause was identified. MI was defined as the occurrence of new Q-waves on the electrocardiogram (ECG) or an elevation of creatine kinase-myocardial band (CK-MB) isoenzyme or troponin level of at least greater than three times the upper normal limit (UNL) in no fewer than two separated blood samples. PMI was defined as MI occurring within 48 hours of the procedure; the causes of PMI included side-branch occlusion, slow or no-reflow, distal embolization, thrombus, dissection, and other nonidentifiable mechanical causes. For patients presented with acute MI at admission, a rise of CK-MB at least 50% greater than the most recent preprocedural value was required for the diagnosis of PMI. Secondary endpoints used were target vessel revascularization (TVR), target lesion revascularization (TLR), stent thrombosis (ST), all-cause death, and a composite of MACE (including MI, cardiac death, TVR, or TLR). TVR was defined as repeat revascularization of the same vessel treated. TLR was defined as repeat intervention of the stented segment. ST was diagnosed according to the definitions by the Academic Research Consortium (ARC)11 and was classified as definite, probable, or possible. ST was also defined by timing: early (<30 days), late (30 days to 1 year), or very late (>1 year). Based on our previous classification for IL-6,4 two prespecified groups were defined as IL-6 level ≥9 pg/mL and IL-6 level <9 pg/mL.
Data collection and follow-up
The data collection process was carried out by independent researchers who were blinded to the study design. The clinical follow-up was performed with office visits or telephone contact scheduled at intervals of 1, 6, 12, 24, and 36 months after the PCI procedure. All patients were encouraged to have a follow-up coronary angiography at 12 months (±30 days) after the index procedure unless clinical reasons indicated an earlier scheduling. In-stent restenosis (ISR) was defined as stenosis of >50% of the vessel’s diameter within a previously stented segment. All of the data were collected and entered into a dedicated computer database by trained personnel of the Clinical Data Management Center.
Statistical analysis
Continuous variables were expressed as the means ± standard deviation (SD) and compared by use of the t-test or the Mann–Whitney U-test as indicated. Categorical variables were compared with the χ2 or Fisher’s exact test. Logarithmic transformation was performed to normalize the distribution of the biomarkers. Survival curves were generated from Kaplan–Meier estimates and compared by use of the log-rank test.
To adjust for the bias inherent of the different IL-6 level, we performed rigorous adjustment for significant differences in the baseline characteristics of patients, with propensity-score matching using the following algorithm: 1:1 optimal match with a ±0.02 (estimated logit within 0.25 SD of propensity score) caliper and no replacement.12,13 The propensity scores were estimated for the likelihood of patients to have IL-6 <9 pg/mL using a nonparsimonious logistic regression model that contained all the covariates listed in Tables 1 and 2. Model discrimination was measured by the c-statistic and calibration was assessed using the Hosmer–Lemeshow goodness-of-fit test. For further confirmation of balanced matching, we assessed the background covariates between the IL-6 <9 pg/mL and IL-6 ≥9 pg/mL groups in the matched cohort. Continuous variables were compared using the paired t-test or the Wilcoxon signed-rank test, as appropriate, and categorical variables were compared using McNemar’s test. Clinical outcomes in the matched population were analyzed with Cox proportional hazards regression stratified on matched pairs. Survival curves were also constructed with Kaplan–Meier estimates and compared by the Klein–Moeschberger test.
Binary logistic regression analysis was performed to find the determinants of IL-6 <9 pg/mL. A simple scatter-dot model was created to identify the correlation of IL-6 values with hs-CRP, and the coefficients with P-value were calculated by the bivariate correlation model. To determine whether similar outcomes of the IL-6 or hs-CRP levels were consistent with the various subgroups, we tested the impact of IL-6 <9 pg/mL or hs-CRP <26.87 mg/L on the incidence of 3-year cardiac death or MI in the multiple prespecified subgroups: age (<65 or ≥65 years), sex, diabetes mellitus, statin treatment before stenting, and acute coronary syndrome (ACS). Multivariate subgroup analysis was performed in the overall population and within the propensity-matched cohort, respectively. All analyses were conducted using Stata software (v12.0; StataCorp LP, College Station, TX, USA), and two-tailed P-values of 0.05 or less were considered statistically significant.
MedCalc (release 11.4.4; MedCalc Software, Mariakerke, Belgium) was used to create and compare the receiver operator characteristic (ROC) curve in order to examine the IL-6 and hs-CRP levels as predictors of 3-year cardiac death or MI.
Results
Patient population
A total of 2,108 patients were recruited into this study; of them, 117 patients were excluded (23 patients with cardiogenic shock, 74 patients with BMS implantation, and 20 patients underwent ballooning without stenting). This left a total of 1,991 patients (72.9% male) who were included in this study.
Baseline characteristics
The clinical demographic characteristics are shown in Table 1. Patients with IL-6 level ≥9 pg/mL (n=1,256, 63.1%) were characterized by a lower proportion of use of statins and diuretics therapy, higher serum concentration of low-density lipoprotein (LDL), and CK-MB isoenzyme, compared to patients with IL-6 level <9 pg/mL (n=735, 36.9%). IL-6 was strongly correlated with CRP (r=0.272, P<0.001, Figure 1A) even after propensity score matching (PSM; Table S1).
Angiographic and procedural features
Lesions and procedural characteristics were shown in Table 2. Compared to the IL-6 level <9 pg/mL group, patients in the IL-6 level ≥9 pg/mL group had more frequent left anterior descending (LAD) disease (64.5% vs 59.6%, P<0.029), but less frequent chronic total occlusion (CTO; 7.5% vs 12.2%, P<0.001), resulting in a higher rate of complete revascularization (63.5% vs 55.1%, P<0.001). However, these differences became nonsignificantly different after PSM as shown in Table S2.
Clinical outcome
Outcome measurements are shown in Table 3. The in-hospital rate of the primary endpoint (defined as MI or death) in the IL-6 level ≥9 pg/mL group was 9.1%, which was statistically significantly different to 6.3% in the IL-6 <9 pg/mL group (P=0.026), mainly driven by the increased rate of MI (9.1% vs 6.1%, P=0.025). These differences in MI/death and MI were sustained through the 3-year follow-up (10.9% vs 7.6%, P=0.017 and 10.1% vs 7.5%, P=0.049) between the two studied groups, even after PSM (12.5% vs 7.7%, P=0.003 and 11.9% vs 7.5%, P=0.006).
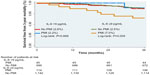
At the 3-year follow-up after the assigned procedure, more frequent MI was also the main reason for increased composite MACE between the IL-6 ≥9 pg/mL and IL-6 <9 pg/mL group before PSM (20.7% vs 15.8%, P=0.007) and after PSM (22.8% vs 15.8%, P=0.001, Tables 3 and S3). There were statistically nonsignificant differences in cardiac death, all-cause death, TLR, TVR, and ST between the two groups. Survival analysis demonstrated that MI/death-free rate at the 3-year follow-up was 12.5% in the IL-6 ≥9 pg/mL group, compared to 7.7% in the IL-6 <9 pg/mL group (P=0.003, Figure 2) after PSM.
Relationship of PMI with IL-6 and mortality
As the IL-6 ≥9 pg/mL group had higher serum concentrations of CRP and an increased rate of MI after PSM, we analyzed the relationship between PMI with inflammatory biomarkers and mortality (Table 4). Notably, in the IL-6 ≥9 pg/mL group, PMI was strongly correlated with mortality at 1-year through to the 3-year (hazard ratio: 2.96, 95% CI: 1.35–6.49, P=0.005) follow-up after PCI procedure.
Different models with input of either IL-6 or CRP or combination of IL-6 and CRP into conventional variables (shown in Tables 1 and 2) were studied (Table 5 and Figure 3). There were no statistically significant differences in mortality rates between patients with and without PMI in the IL-6 level <9 pg/mL group (Figure 4). In contrast, patients with PMI in the IL-6 level ≥9 pg/mL group had significantly higher mortality rates compared to patients without PMI at the 1-year (2.6% vs 0.3%, 95% CI: 2.05–50.25, P<0.001), 2-year (4.4% vs 1.2%, 95% CI: 1.32–10.16, P=0.008), and 3-year follow-ups (7.0% vs 2.5%, 95% CI: 1.35–6.49, P=0.005). Subgroup analysis showed that patients stratified by sex, diabetes, statin treatment, ACS, left ventricular ejection fraction, multivessel disease, and LAD disease had more favorable clinical status if IL-6 was <9 pg/mL (Figure 5).
Discussion
The main findings of the present study are: 1) elevated preprocedural IL-6 level was associated with an increased risk of death or MI even after PSM and 2) the presence of PMI enhances the predictive value of the serum IL-6 level.
PCI procedure using DES has been shown to inhibit inflammatory response and smooth cell migration and proliferation, reduce neointimal hyperplasia, and therefore minimize the occurrence of restenosis.14 However, the implantation of DES has been associated with delayed stent endothelialization, leading to late and very late thrombosis, even though they were successful in reducing the occurrence of stent restenosis.3 It has been reported that regardless of whether BMS or DES are used, increased concentrations of inflammatory cytokines can be detected immediately after the PCI procedure, suggesting that it is associated with the procedure. In accordance with that fact, several inflammatory biomarkers, including IL-6 and hs-CRP, have been proven to be associated with unfavorable outcomes in patients with coronary heart disease who underwent PCI.5,15,16 Some of the most devastating outcomes after PCI are MI and cardiac death. In a recent study by Su et al,17 serum IL-6 concentrations were shown to be clearly associated with all-cause and cardiovascular mortality independent of potential confounders in a large number of coronary artery disease patients with homogeneous status. Chen et al4 also reported that IL-6 can predict mortality and morbidity after DES implantation for a group of patients with unstable angina who were not on statin therapy. In this study, we observed the predictive value of serum IL-6 level for clinical outcome in patients overall. Our study found that high serum levels of IL-6 were associated with more frequent death and MI rates compared to low serum IL-6 levels throughout the duration of our study. A higher rate of MI in the group of patients with high IL-6 levels also resulted in additional value of IL-6 to predict MACE. Furthermore, we performed PSM to avoid the result being affected by treatment selection bias and potential confounding. Thus, in this study, high levels of serum IL-6 were associated with the risk of a composite MACE, because of the correlation with MI and death, in patients with obstructive coronary disease who received DES implantation.
As mentioned earlier, the group with elevated serum IL-6 levels had an increased rate of MI in this current study. PMI is one of the most common complications of PCI and can be induced by several angiographic mechanisms such as side-branch occlusion, slow flow or no-reflow (abrupt closure), distal embolization, and other mechanical causes.18,19 Moreover, pooled data from recent studies showed that individuals with PMI required stricter monitoring due to a greater disease burden and more unstable disease, thus having higher mortality rates.18,20,21 Circulating serum levels of IL-6 have also been associated with MI. Several studies have confirmed that the inflammation reaction in acute MI was accompanied with the production of cytokines, which lead to elevations in IL-6 levels.22–24 We performed further analysis of the relationship of PMI with inflammatory biomarkers and mortality. Our data showed that patients with both serum IL-6 level ≥9 pg/mL and PMI were clearly associated with a higher rate of mortality compared to the patients with serum IL-6 level <9 pg/mL, as well as patients with serum IL-6 level ≥9 pg/mL with no PMI (Figure 4). As one of the proinflammatory and immunoregulatory cytokines, IL-6 has been reported to induce the aggregation of platelets, proliferation of vascular smooth muscle cells, and production of fibrinogen by hepatocytes.22,25 Therefore, it has been widely accepted that chronic inflammation plays a large role in the development and prognosis of atherosclerosis. Increased levels of serum IL-6 combined with the occurrence of PMI, which in turn promotes more inflammatory response, resulted in higher rates of mortality in this study population, thus supporting the previously mentioned theory.
We also found a strong correlation between IL-6 and hs-CRP, which can be explained by the fact that IL-6 is the major stimulant for the production of acute-phase proteins, including hs-CRP, by hepatocytes.26 Our data indicates that IL-6 is the stronger discriminating marker despite the strong correlation with hs-CRP. Our evaluation showed that adding IL-6 to the raw model resulted in a higher increase of the prediction of mortality compared to adding hs-CRP. IL-6 also improved the prediction of mortality further when added to the model already including hs-CRP in the IL-6 <9 pg/mL group (Table 5). However, this was not the case with the IL-6 level ≥9 pg/mL group. There was no obvious increase of predictive value in adding IL-6 to both the raw model and the model already including hs-CRP. One of the possible explanations for this is the use of medications that may influenced the levels of inflammatory cytokines, including IL-6 and hs-CRP, in our study population. In this study, patients were given HMG-CoA reductase inhibitors (statins), which have been shown to suppress IL-6 production, leading to early progressive improvement in endothelial function and inhibition of inflammatory response.27 Generally, patients with more severe disease had higher serum IL-6 levels, and consequently received a higher dose of medication, which included HMG-CoA reductase inhibitors, among others. This might be another factor affecting the results from our data. Unfortunately, we could not collect all the data of different doses of medication given to the patients in this study, and so we were not able to further investigate this theory. The findings in this study showed that serum IL-6 is clearly associated with cardiac death or MI and also composite MACE after the implantation of DES. However, serum IL-6 should not be perceived as the cause of cardiac death or MI but rather as a biomarker in identifying high-risk patients in clinical settings. Future research is required to verify whether IL-6 can be one of the causative factors of cardiac death or MI.
Several limitations were present in our study. First, this is a retrospective cohort study; hence, there were various residual unmeasured confounders or selection bias, which cannot be completely removed and may affect the results in this study. Second, as mentioned earlier, we did not assess the impact of difference in statin medication doses on the patients’ clinical outcomes. Third limitation is the duration of antiplatelet therapy used, which has also been reported as one of the factors influencing ST. In this study, hospitalized patients were required to take aspirin and suggested to continue the therapy for life after being discharged from hospital, but our data lacks the numbers of patients who continued taking aspirin and patients who prematurely stopped taking aspirin after being discharged. Fourth, our study used CK-MB for the detection of PMI and we did not perform further comparisons with other biomarkers, such as cardiac troponin, for the clinical outcomes in this study population. Finally, we did not investigate the differences in outcomes of different stent types in both groups, so we could not assess the association of the stent types with the risk of clinical adverse events.
Conclusion
Elevated preprocedural serum IL-6 level was correlated with death, MI, and MACE after implantation of the DES. PMI enhances the predictive value of IL-6 for post-DES events.
Disclosure
The authors report no conflicts of interest in this work.
References
Park DW, Seung KB, Kim YH, et al. Long-term safety and efficacy of stenting versus coronary artery bypass grafting for unprotected left main coronary artery disease: 5-year results from the MAIN-COMPARE (Revascularization for Unprotected Left Main Coronary Artery Stenosis: Comparison of Percutaneous Coronary Angioplasty Versus Surgical Revascularization) registry. J Am Coll Cardiol. 2010;56(2):117–124. | |
Yeh RW, Chandra M, McCulloch CE, Go AS. Accounting for the mortality benefit of drug-eluting stents in percutaneous coronary intervention: a comparison of methods in a retrospective cohort study. BMC Med. 2011;9:78. | |
Nakazawa G, Finn AV, Joner M, et al. Delayed arterial healing and increased late stent thrombosis at culprit sites after drug-eluting stent placement for acute myocardial infarction patients: an autopsy study. Circulation. 2008;118(11):1138–1145. | |
Chen SL, Liu Y, Lin L, et al. Interleukin-6, but not C-reactive protein, predicts the occurrence of cardiovascular events after drug-eluting stent for unstable angina. J Interv Cardiol. 2014;27(2):142–154. | |
Hwang SJ, Park KW, Kwon DA, et al; Korea Stent Thrombosis Investigators. High plasma interleukin-6 is associated with drug-eluting stent thrombosis: possible role of inflammatory cytokines in the development of stent thrombosis from the Korea Stent Thrombosis Registry. Circ J. 2011;75(6):1350–1357. | |
Delhaye C, Maluenda G, Wakabayashi K, et al. Long-term prognostic value of preprocedural C-reactive protein after drug-eluting stent implantation. Am J Cardiol. 2010;105(6):826–832. | |
Patel VG, Michael TT, Mogabgab O, et al. Clinical, angiographic, and procedural predictors of periprocedural complications during chronic total occlusion percutaneous coronary intervention. J Invasive Cardiol. 2014;26(3):100–105. | |
Song PS, Song YB, Yang JH, et al. Periprocedural myocardial infarction is not associated with an increased risk of long-term cardiac mortality after coronary bifurcation stenting. Int J Cardiol. 2013;167(4):1251–1256. | |
Niccoli G, Sgueglia GA, Latib A, Crea F, Colombo A; CACTUS Study Group. Association of baseline C-reactive protein levels with periprocedural myocardial injury in patients undergoing percutaneous bifurcation intervention: a CACTUS study subanalysis. Catheter Cardiovasc Interv. 2014;83(1):E37–E44. | |
Lindsey JB, Kennedy KF, Stolker JM, et al. Prognostic implications of creatine kinase-MB elevation after percutaneous coronary intervention: results from the Evaluation of Drug-Eluting Stents and Ischemic Events (EVENT) registry. Circ Cardiovasc Interv. 2011;4(5):474–480. | |
Mauri L, Hsieh WH, Massaro JM, Ho KK, D’Agostino R, Cutlip DE. Stent thrombosis in randomized clinical trials of drug-eluting stents. N Engl J Med. 2007;356(10):1020–1029. | |
D’Agostino RB Jr.Propensity scores in cardiovascular research. Circulation. 2007;115(17):2340–2343. | |
Austin PC. Some methods of propensity-score matching had superior performance to others: results of an empirical investigation and Monte Carlo simulations. Biom J. 2009;51(1):171–184. | |
Abizaid A, Costa JR Jr. New drug-eluting stents: an overview on biodegradable and polymer-free next-generation stent systems. Circ Cardiovasc Interv. 2010;3(4):384–393. | |
Gao J, Liu Y, Cui RZ, et al. Relationship of interleukin-6-572C/G promoter polymorphism and serum levels to post-percutaneous coronary intervention restenosis. Chin Med J (Engl). 2013;126(6):1019–1025. | |
Kim BK, Kim JS, Oh C, et al. Impact of preprocedural high-sensitivity C-reactive protein levels on uncovered stent struts: an optical coherence tomography study after drug-eluting stent implantation. Clin Cardiol. 2011;34(2):97–101. | |
Su D, Li Z, Li X, et al. Association between serum interleukin-6 concentration and mortality in patients with coronary artery disease. Mediators Inflamm. 2013;2013:726178. | |
Zimarino M, Affinito V. The prognosis of periprocedural myocardial infarction after percutaneous coronary interventions. Cardiovasc Revasc Med. 2013;14(1):32–36. | |
Park DW, Kim YH, Yun SC, et al. Frequency, causes, predictors, and clinical significance of peri-procedural myocardial infarction following percutaneous coronary intervention. Eur Heart J. 2013;34(22):1662–1669. | |
Park DW, Kim YH, Yun SC, et al. Impact of the angiographic mechanisms underlying periprocedural myocardial infarction after drug-eluting stent implantation. Am J Cardiol. 2014;113(7):1105–1110. | |
Gili S, D’Ascenzo F, Moretti C, et al. Impact on prognosis of periprocedural myocardial infarction after percutaneous coronary intervention. J Interv Cardiol. 2014;27(5):482–490. | |
Sturk A, Hack CE, Aarden LA, Brouwer M, Koster RR, Sanders GT. Interleukin-6 release and the acute-phase reaction in patients with acute myocardial infarction: a pilot study. J Lab Clin Med. 1992;119(5):574–579. | |
Nossuli TO, Lakshminarayanan V, Baumgarten G, et al. A chronic mouse model of myocardial ischemia-reperfusion: essential in cytokine studies. Am J Physiol Heart Circ Physiol. 2000;278(4):H1049–H1055. | |
Ege T, Canbaz S, Yuksel V, Duran E. Effect of pericardial fluid pro-inflammatory cytokines on hemodynamic parameters. Cytokine. 2003;23(1–2):47–51. | |
Seino Y, Ikeda U, Ikeda M, et al. Interleukin 6 gene transcripts are expressed in human atherosclerotic lesions. Cytokine. 1994;6(1):87–91. | |
Heinrich PC, Castell JV, Andus T. Interleukin-6 and the acute phase response. Biochem J. 1990;265(3):621–636. | |
Nawawi H, Osman NS, Annuar R, Khalid BA, Yusoff K. Soluble intercellular adhesion molecule-1 and interleukin-6 levels reflect endothelial dysfunction in patients with primary hypercholesterolaemia treated with atorvastatin. Atherosclerosis. 2003;169(2):283–291. |
Supplementary materials
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.