Back to Journals » Patient Preference and Adherence » Volume 9
Patient–provider communication, self-reported medication adherence, and race in a postmyocardial infarction population
Authors Zullig L, Shaw R, Shah B, Peterson E, Lindquist J, Crowley M, Grambow S, Bosworth H
Received 4 October 2014
Accepted for publication 16 December 2014
Published 19 February 2015 Volume 2015:9 Pages 311—318
DOI https://doi.org/10.2147/PPA.S75393
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Leah L Zullig,1,2 Ryan J Shaw,1,3 Bimal R Shah,4,5 Eric D Peterson,4,5 Jennifer H Lindquist,1 Matthew J Crowley,1,2 Steven C Grambow,6 Hayden B Bosworth1–3,7
1Center for Health Services Research in Primary Care, Durham Veterans Affairs Medical Center, Durham, NC, USA; 2Division of General Internal Medicine, Duke University, Durham, NC, USA, 3School of Nursing, Duke University, Durham, NC, USA, 4Division of Cardiology, Department of Medicine, Duke University, Durham, NC, USA; 5Duke Clinical Research Institute, Duke University Durham, NC, USA; 6Department of Biostatistics and Bioinformatics, Duke University, Durham, NC, USA, 7Department of Psychiatry and Behavioral Sciences, Duke University, Durham, NC, USA
Objectives: Our objectives were to: 1) describe patient-reported communication with their provider and explore differences in perceptions of racially diverse adherent versus nonadherent patients; and 2) examine whether the association between unanswered questions and patient-reported medication nonadherence varied as a function of patients’ race.
Methods: We conducted a cross-sectional analysis of baseline in-person survey data from a trial designed to improve postmyocardial infarction management of cardiovascular disease risk factors.
Results: Overall, 298 patients (74%) reported never leaving their doctor’s office with unanswered questions. Among those who were adherent and nonadherent with their medications, 183 (79%) and 115 (67%) patients, respectively, never left their doctor’s office with unanswered questions. In multivariable logistic regression, although the simple effects of the interaction term were different for patients of nonminority race (odds ratio [OR]: 2.16; 95% confidence interval [CI]: 1.19–3.92) and those of minority race (OR: 1.19; 95% CI: 0.54–2.66), the overall interaction effect was not statistically significant (P=0.24).
Conclusion: The quality of patient–provider communication is critical for cardiovascular disease medication adherence. In this study, however, having unanswered questions did not impact medication adherence differently as a function of patients’ race. Nevertheless, there were racial differences in medication adherence that may need to be addressed to ensure optimal adherence and health outcomes. Effort should be made to provide training opportunities for both patients and their providers to ensure strong communication skills and to address potential differences in medication adherence in patients of diverse backgrounds.
Keywords: acute myocardial infarction, hypertension, health policy and outcome research, communication
Introduction
Medication nonadherence is a common and expensive problem in the United States. Only 50% of patients report taking medications for cardiovascular disease (CVD) as prescribed.1 Patients may be particularly susceptible to medication nonadherence during the period following a myocardial infarction (MI). During this time, patients often require multiple medications to lower their future cardiac risk requiring intensive self-management, which may place them at increased risk for medication nonadherence.2
Although there is no clear risk profile, many factors influence medication nonadherence including both patient- and provider-driven factors.3 Patient–provider interactions appear to be a major determinant of medication nonadherence, particularly as it pertains to CVD risk factor reduction. Poor physician communication alone has been associated with an up to 19% higher risk of medication nonadherence.4–6 Conversely, high-quality communication may improve adherence. Providing tailored information, patient satisfaction with the communication received, and beliefs about medication are connected and can lead to improved medication adherence.7 Part of patient-reported communication quality may be based on the communication style used during the clinical encounter – instrumental (ie, explicit, direct) or affective (ie, implicit, indirect). An affective communication style, including social talk, rapport building, and asking questions, may be associated with identifying more psychosocial and behavioral problems such as medication adherence.8 Tailored communication matching patients’ preferred typology of communication may improve perceived barriers to medication adherence.9
Physician communication behaviors may have a varying effect on patient trust, depending on the patient’s race,10 and patients of minority race are more likely to be nonadherent with their medications.11,12 Race may have a stronger association with patient–provider rapport building and the quality of patient–physician communication than do certain clinical factors, such as blood pressure (BP) control.13 Moreover, racial concordance between a patient and provider has been associated with adherence to CVD medications.14 Elderly African Americans reported that they followed physician instructions on how to take medications less frequently than did elderly white patients, even after adjusting for potentially confounding differences such as health literacy and other sociodemographic characteristics.11
Racial differences in expectations of medical interactions and in medication adherence are known.10–12 Compared to white patients, those of African American race have reported lower levels of trust of physicians and fewer informational encounters.15 Collins et al16 demonstrated that while both white and African American patients wanted more informational clarity about cardiac testing, African American patients valued building trust with their providers to a higher degree than their white counterparts.
While patient–provider communication and CVD-related medication nonadherence are associated,17 it is not known whether a previous history of MI impacts this relationship, nor is it known whether a patient’s race may influence communication quality among post-MI patients. We considered this issue in the context of the Expectancy Violations theoretical framework.18 This theoretical framework depicts communication as an exchange of information that encompasses relational content. Those communicating have expectations for their informational exchange. When there is inconsistency in expectations and what occurs in the interaction, there may be dissatisfaction with the communication and resulting negative outcomes.18,19 For example, in the context of adherence to an exercise program, when patients’ expectations were violated, there was a greater degree of nonadherence.20 Conversely, meeting patients’ expectations has been associated with increased adherence.19,21 We were interested in patients’ expectations of their doctors in medical interactions, specifically the expectations that doctors address all of a patient’s concerns and answer their questions, and how that affected medication adherence.
Because post-MI patients are at an especially high risk for future cardiovascular morbidity and mortality, and race has been found to be a significant moderator of patient/provider communication,22–24 a better understanding of the impact of patient–provider communication on medication nonadherence in the post-MI period is essential. Thus, the objective of our analysis was twofold. First, we aimed to describe patient-reported aspects of communication with their provider(s) and differences in perceptions of racially diverse adherent versus nonadherent patients. Second, we sought to examine whether the association between leaving a provider’s office with unanswered questions and medication nonadherence varied as a function of patients’ race. Given the briefness of the items, if associated, the issue of unanswered questions could be used as a screening measure for potential poor quality communication.
Methods
Data source
Data were obtained from a trial to improve post-MI management called the Secondary Prevention Risk Interventions via Telemedicine and Tailored Patient Education (SPRITE) study (clinicaltrials.gov resistry number: NCT00901277). The methods of the SPRITE study have been previously described in detail.25 In brief, SPRITE is a three-arm randomized controlled trial using the following two electronic self-management tools: HealthVault, a Web-based communication tool created by Microsoft Corporation (Redmond, WA, USA), with Heart360, the American Heart Association’s (Dallas, TX, USA) Web-based heart health tracker; and a portable electronic BP cuff. To be eligible for the study, patients had to have a current hypertension diagnosis (by the International Classification of Diseases 9 diagnosis code or elevated BP on two consecutive clinic visits) and a history of MI within the 3 years prior to enrollment. Patients (total number [N]=406) were enrolled and randomized to one of three arms: either 1) home BP monitoring plus a nurse-delivered, telephone-based tailored patient education intervention, and enrollment in HealthVault and Heart360; 2) home BP monitoring plus a tailored, Web-based patient education intervention, and enrollment in HealthVault and Heart360; or 3) usual care.
A survey assessing patients’ perceptions of communication with their physicians and self-reported medication nonadherence, among other factors, was administered at enrollment. We used this baseline survey data to evaluate associations between self-reported medication nonadherence and items reflecting patient–provider communication.
Outcome measure: self-reported medication nonadherence
Self-reported medication nonadherence
A modified Morisky Medication-Taking Scale was used to assess self-reported medication nonadherence. To ease respondent burden, we used a validated, four-item measure rather than the lengthier eight-item measure.26–28 Patients were asked whether four statements about CVD medication-taking behaviors were true for them over the previous 30 days: 1) “I sometimes forget to take my medicine”; 2) “I am sometimes careless about taking my medicine”; 3) “when I feel better, I sometimes stop taking my medicine”; and 4) “if I feel worse when I take the medicine, sometimes I stop taking it”. Each of the medication adherence items could be answered on a four-point Likert scale with responses ranging from “strongly agree” to “strongly disagree”. Consistent with prior research,29 patients were dichotomized into either the “adherent” or “nonadherent” group. Individuals were classified as nonadherent if they responded affirmatively, “don’t know”, or “refused” to any of the four statements; otherwise, patients were classified as adherent. Patients with missing data on any of these four items were excluded from the analysis. The Cronbach’s alpha (α=0.80) for the Morisky medication adherence items indicated a good degree of internal consistency.
Primary independent variables: patient-reported communication and race
Patient-reported communication
The SPRITE baseline survey contained survey items extracted from the Primary Care Assessment Survey (PCAS),30 which was designed as a patient-completed questionnaire operationalizing the Institute of Medicine’s concept of primary care. The SPRITE baseline survey contained three of six items from the communication subdomain of the PCAS. We selected these items based on face validity and expected relevance to the post-MI patient population.
Communication questions included on the baseline survey were: “How often do you leave your doctor’s office with unanswered questions?”; “In the last 12 months, how often did your personal doctor explain things in a way that was easy to understand?”; and, “In the last 12 months, how often did your personal doctor listen carefully to you?” Response options for the “unanswered questions” item were on a four-point Likert scale. In addition to examining each communication item descriptively, a binary measure was created for the “unanswered questions” item for use in the analyses (“at least some of the time” versus another nonmissing response).
Race
As previously described, race impacts medication adherence and perceived communication.31 Race was based on patients’ self-reported race during the baseline survey. Possible response options included: “White or Caucasian”; “Black or African American”; “Asian”; “American Indian/Alaska Native”; “Native Hawaiian or Other Pacific Islander”; as well as “other”, “don’t know”, or “refused”. Because there were few non-African American minorities (sample number [n]=20), we created a binary measure of the race variable (minority versus all nonminority races).
Covariates: sociodemographic factors
As a proxy measure for social support, marital status was included. Married people tend to engage in healthier behaviors, including medication adherence, compared to those who are unmarried.32 This analysis included a binary measure for those who were partnered (married or living with a partner versus other). People with less than a high school education and/or who are unemployed are at increased risk for medication nonadherence.33–35
Low health literacy has been suggested to correspond with medication nonadherence and to also negatively influence communication between patients and their providers.4 Health literacy was assessed using the Rapid Estimate of Adult Literacy in Medicine (REALM) test.36 Low health literacy was a dichotomous variable defined as a REALM score of up to and including the eighth grade (≤60 score) versus the ninth grade or higher (>61 score).37
We included a binary measure of employment (employed part time or full time versus not employed).A dichotomized measure of patient-reported educational attainment was also included in the analysis (less than high school education versus high school or greater education). Patients were asked to describe their household’s current financial situation. Possible response options included: “after paying the bills, you still have enough money for special things that you want”; “you have enough money to pay the bills, but little spare money to buy extra or special things”; “you have money to pay the bills, but only because you have to cut back on things”; or “you are having difficulty paying the bills no matter what you do”. Patients who reported the latter two categories (eg, cutting back on things or difficulty paying bills) were considered to have an inadequate financial status.
Statistical analysis
Data were analyzed in Stata version 12.1 (StataCorp LP, College Station, TX, USA) and SAS version 9.2 (SAS Institute Inc., Cary, NC, USA). Descriptive statistics were used to summarize baseline patient characteristics and patient-reported communication by nonadherence status and race. Multivariable logistic regression was used to examine whether the association between medication nonadherence and communication (ie, unanswered questions) varied as a function of patients’ race. The model included an interaction term for unanswered questions by race and was adjusted for covariates that were selected a priori based on factors previously shown to impact medication nonadherence.31–35,38–41 Model results are presented as odds ratios (OR), 95% confidence intervals (CI), and P-values. The impact of the interaction term is reported by providing the interaction P-value and ORs for the simple main effects of unanswered questions conditional on level of race.
Results
Study population
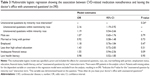
The total number of patients examined was 405. One patient was omitted from the analysis because of missing medication nonadherence information. More than half of the patients reported being adherent (n=232; 57%). Most patients were male (n=292; 72%) and married or living with a partner (n=269; 66%). A minority of patients had less than a high school education (n=53; 13%), low health literacy (n=68; 17%), were employed (n=149; 37%), or reported inadequate financial status (n=92; 23%). A full description of the patients’ baseline characteristics by adherence status and race is provided in Table 1.
Communication
Few patients reported always leaving their doctor’s office with unanswered questions (n=8; 2%). Overall, 298 patients (74%) reported never leaving their doctor’s office with unanswered questions. Among those who were adherent and nonadherent with their medications, 183 (79%) and 115 (67%) patients, respectively, never left their doctor’s office with unanswered questions. Similarly, most patients reported that their personal doctor always explained things in a way that was easy to understand (n=293; 72%). Among adherent patients, 181 (78%) reported always having things well explained by their doctor; among nonadherent patients, 112 (65%) reported always having things well explained by their doctor. The majority of patients (n=282; 70%) reported that their doctors always listened carefully. Additional information regarding individual communication items by adherence status and race are provided in Table 2.
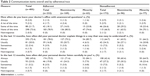  | Table 2 Communication items overall and by adherence/race |
Medication nonadherence
Table 3 presents results from the multivariable logistic regression model. The OR and 95% CI estimates are from the full model, which included the interaction term (ie, minority race by unanswered questions). Although the simple effects of the interaction term were different for patients of nonminority race (OR: 2.16; 95% CI: 1.19–3.92) and those of minority race (OR: 1.19; 95% CI: 0.54–2.66), the overall interaction effect was not statistically significant (P=0.24). Additionally, none of the a priori covariates including male sex (OR: 1.07; 95% CI: 0.65–1.76), married/living with a partner (OR: 0.92; 95% CI: 0.58–1.48), employed (OR: 1.18; 95% CI: 0.76–1.84), less than a high school education (OR: 1.43; 95% CI: 0.72–2.83), inadequate financial status (OR: 1.55; 95% CI: 0.94–2.56), and low health literacy (OR: 0.98; 95% CI: 0.52–1.85) were significantly associated with medication nonadherence.
Discussion
Productive interactions between informed patients and proactive providers are a critical element in the management of chronic disease.42 Despite the importance of communication, patients both in our study and in other studies43,44 have reported leaving their doctor’s office with unaddressed questions. We report two primary findings. First, consistent with existing literature, we found that nonwhite patients were more likely to be nonadherent than white patients.45,46 Second, we determined that factors associated with nonadherence did not differ as a function of patients’ race. We found that leaving with unanswered questions after a doctor’s visit was not associated with medication nonadherence as a function of race. These results differ from previously published studies.10–13 This may be because our study relied on subjective measures that were self-reported by patients. Differences in patients’ expectations as a function of their race and how violations of these expectations may influence their adherence behaviors are not known. For example, did patients’ expectations of whether or not doctors would or should address all of their questions vary by race? This was not addressed in the current study. Further, an association between financial burden and nonadherence is known,47,48 and while the estimated odds ratio for patient-reported inadequate financial status (OR: 1.55) was suggestive of an association with medication nonadherence, this was not significant (P=0.09) in the adjusted model.
While not addressed in the current study, when patients have unanswered questions, there may be uncertainty about how to properly take their medications. Patients may not speak with their doctor about important barriers to medication nonadherence, such as the cost of their medications. Atreja et al49 reviewed proven interventions to increase medication adherence and summarized key points in a mnemonic device. The mnemonic is “SIMPLE”: simplifying regimen characteristics; imparting knowledge; modifying patients’ beliefs; patient communication; leaving the bias; and evaluating adherence.49 The latter five elements hinge on strong communication between patients and their providers, highlighting its chief importance in improving adherence.
Because patients and providers often perceive the quality of communication differently,50 routinely asking patients if they have additional questions and/or asking them to rate interactions with their doctors may be an important tool to increase medication adherence. At minimum, this would increase awareness of the importance of communication among both patients and providers. Cultivating communication skills has been the focus of much attention and is now a standard part of most medical education curricula.51 While this is a critical first step, teaching providers about quality communication is only one-half of the equation for a productive interaction. Patients also must be educated. When both patients and providers are trained in effective communication, they exhibit a greater sense of control and preference for a more active role in decision making.52 In a study conducted by Haskard et al53 the researchers determined that when physicians were trained, patients reported increased satisfaction. When patients were trained, physicians’ satisfaction with data collection improved. If only the physician or the patient was trained (not both), then physician stress increased and satisfaction decreased.53
Our study has several limitations. Because this analysis is cross-sectional, we are unable to determine the directionality of the association between poor communication and medication nonadherence; it may be that, compared to those who are nonadherent, patients who adhere have other unmeasured characteristics that would lead them to be more proactive in their medical interactions. Similarly, whether the quality of patient–doctor interactions directly caused nonadherence behavior cannot be determined from these data. There may be unmeasured confounders, such as the length of time spent in the encounter,13 and/or cultural differences not assessed by race alone. We did not have information about race concordance between patients and their providers. For African American patients, race concordance between a patient and provider has been associated with adherence to CVD medications.14 Moreover, African American patients with uncontrolled BP have been shown to have shorter medical visits with less rapport building than white patients with controlled BP.13 At least one study concluded that patient race has a stronger association with the quality of the patient–physician communication than do certain clinical factors, such as BP control.13 The small percentage of non-African American minorities precluded us from evaluating specific differences among different minority groups. Additionally, medication nonadherence was measured through three patient-reported items. While we used a validated measure of medication adherence, it is possible that patients misrepresented their actual adherence behaviors. The three included items do not address a full spectrum of communication quality indicators. Ideally, a more comprehensive measure of patient-reported communication measures would be assessed in tandem with a potentially more objective observational measurement, such as videotaping or audio taping patient–doctor interactions. Lastly, failure to detect differences between medication nonadherence and communication by race may have resulted from a lack of statistical power, as the original study was not powered specifically to detect interaction effects.
Conclusion
The quality of patient–provider communication may be an important resource for supporting CVD medication adherence. While the association between race and having unanswered questions was not statistically significant, racial differences in medication adherence were prevalent and should be addressed to ensure maximum adherence. Future studies should seek to understand the temporality between communication and medication nonadherence, as well as to identify specific strategies to improve adherence in patients of diverse backgrounds at both an individual patient–provider dyad level, as well as at a health care facility or systems level.
Practice implications
Effort should be made to provide training opportunities for both patients and their providers to ensure strong communication skills.
Acknowledgments
This study was supported in part by an award from the American Heart Association Pharmaceutical Roundtable and David and Stevie Spina. Dr Zullig (CDA 13-025) and Dr Crowley (CDA 13-261) are supported by VA Health Services Research and Development Career Development Awards. Dr Bosworth was supported by a research career scientist award from VA Health Service Research and Development (VA HSR&D 08-027). This project was also supported in part by grant number U19HS021092 from the Agency for Healthcare Research and Quality.
Disclosure
SCG receives consulting fees from Gilead Sciences for serving on multiple Data and Safety Monitoring Boards (DSMBs). Although the relationship is not perceived to represent a conflict with the present work, it has been included in the spirit of full disclosure. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of Duke University, the US Department of Veterans Affairs, or the United States government. The other authors report no conflicts of interest in this work.
References
Bosworth HB. How can innovative uses of technology be harnessed to improve medication adherence? Expert Rev Pharmacoecon Outcomes Res. 2012;12(2):133–135. | ||
Jneid H, Anderson JL, Wright RS, et al. 2012 ACCF/AHA focused update of the guideline for the management of patients with unstable angina/non-ST-elevation myocardial infarction (updating the 2007 guideline and replacing the 2011 focused update): a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2012;60(7):645–681. | ||
van Dijk L, Heerdink ER, Somai D, et al. Patient risk profiles and practice variation in nonadherence to antidepressants, antihypertensives and oral hypoglycemics. BMC Health Serv Res. 2007;7:51. | ||
Jolles EP, Clark AM, Braam B. Getting the message across: opportunities and obstacles in effective communication in hypertension care. J Hypertens. 2012;30(8):1500–1510. | ||
Roter DL, Hall JA, Aoki Y. Physician gender effects in medical communication: a meta-analytic review. JAMA. 2002;288(6):756–764. | ||
Zolnierek KB, Dimatteo MR. Physician communication and patient adherence to treatment: a meta-analysis. Med Care. 2009;47(8):826–834. | ||
Linn AJ, van Weert JC, van Dijk L, Horne R, Smit EG. The value of nurses’ tailored communication when discussing medicines: Exploring the relationship between satisfaction, beliefs and adherence. J Health Psychol. 2014. pii: 1359105314539529. | ||
Deveugele M, Derese A, De Bacquer D, van den Brink-Muinen A, Bensing J, De Maeseneer J. Is the communicative behavior of GPs during the consultation related to the diagnosis? A cross-sectional study in six European countries. Patient Educ Couns. 2004;54(3):283–289. | ||
Linn AJ, van Weert JC, Schouten BC, Smit EG, van Bodegraven AA, van Dijk L. Words that make pills easier to swallow: a communication typology to address practical and perceptual barriers to medication intake behavior. Patient Prefer Adherence. 2012;6:871–885. | ||
Martin KD, Roter DL, Beach MC, Carson KA, Cooper LA. Physician communication behaviors and trust among black and white patients with hypertension. Med Care. 2013;51(2):151–157. | ||
Gerber BS, Cho YI, Arozullah AM, Lee SY. Racial differences in medication adherence: A cross-sectional study of Medicare enrollees. Am J Geriatr Pharmacother. 2010;8(2):136–145. | ||
Rolnick SJ, Pawloski PA, Hedblom BD, Asche SE, Bruzek RJ. Patient characteristics associated with medication adherence. Clin Med Res. 2013;11(2):54–65. | ||
Cené CW, Roter D, Carson KA, Miller ER 3rd, Cooper LA. The effect of patient race and blood pressure control on patient-physician communication. J Gen Intern Med. 2009;24(9):1057–1064. | ||
Traylor AH, Schmittdiel JA, Uratsu CS, Mangione CM, Subramanian U. Adherence to cardiovascular disease medications: does patient-provider race/ethnicity and language concordance matter? J Gen Intern Med. 2010;25(11):1172–1177. | ||
Gordon HS, Street RL, Sharf BF, Kelly PA, Souchek J. Racial differences in trust and lung cancer patients’ perceptions of physician communication. J Clin Oncol. 2006;24(6):904–909. | ||
Collins TC, Clark JA, Petersen LA, Kressin NR. Racial differences in how patients perceive physician communication regarding cardiac testing. Med Care. 2002;40(1 Suppl):I27–I34. | ||
Bosworth HB, Granger BB, Mendys P, et al. Medication adherence: a call for action. Am Heart J. 2011;162(3):412–424. | ||
Burgoon JK. A communication model of personal space violations: explication and an initial test. Hum Commun Res. 1978;4(2):129–142. | ||
Burgoon M, Birk TS, Hall JR. Compliance and satisfaction with physician-patient communication an expectancy theory interpretation of gender differences. Hum Commun Res. 1991;18(2):177–208. | ||
Sears SR, Stanton AL. Expectancy-value constructs and expectancy violation as predictors of exercise adherence in previously sedentary women. Health Psychol. 2001;20(5):326–333. | ||
Klingle RS. Bringing time into physician compliance-gaining research: toward a reinforcement expectation theory of strategy effectiveness. Health Commun. 1993;5(4):283–308. | ||
Burnett-Zeigler I, Kim HM, Chiang C, et al. The association between race and gender, treatment attitudes, and antidepressant treatment adherence. Int J Geriatr Psychiatry. 2014;29(2):169–177. | ||
Schoenthaler A, Allegrante JP, Chaplin W, Ogedegbe G. The effect of patient-provider communication on medication adherence in hypertensive black patients: does race concordance matter? Ann Behav Med. 2012;43(3):372–382. | ||
Schoenthaler A, Chaplin WF, Allegrante JP, et al. Provider communication effects medication adherence in hypertensive African Americans. Patient Educ Couns. 2009;75(2):185–191. | ||
Shah BR, Adams M, Peterson ED, et al. Secondary prevention risk interventions via telemedicine and tailored patient education (SPRITE): a randomized trial to improve postmyocardial infarction management. Circ Cardiovasc Qual Outcomes. 2011;4(2):235–242. | ||
Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care. 1986;24(1):67–74. | ||
Shalansky SJ, Levy AR, Ignaszewski AP. Self-reported Morisky score for identifying nonadherence with cardiovascular medications. Ann Pharmacother. 2004;38(9):1363–1368. | ||
Morisky DE, Ang A, Krousel-Wood M, Ward HJ. Predictive validity of a medication adherence measure in an outpatient setting. J Clin Hypertens (Greenwich). 2008;10(5):348–354. | ||
Thorpe CT, Bryson CL, Maciejewski ML, Bosworth HB. Medication acquisition and self-reported adherence in veterans with hypertension. Med Care. 2009;47(4):474–481. | ||
Safran DG, Kosinski M, Tarlov AR, et al. The Primary Care Assessment Survey: tests of data quality and measurement performance. Med Care. 1998;36(5):728–739. | ||
Gu Q, Burt VL, Paulose-Ram R, Dillon CF. Gender differences in hypertension treatment, drug utilization patterns, and blood pressure control among US adults with hypertension: data from the National Health and Nutrition Examination Survey 1999–2004. Am J Hypertens. 2008;21(7):789–798. | ||
Trivedi RB, Ayotte B, Edelman D, Bosworth HB. The association of emotional well-being and marital status with treatment adherence among patients with hypertension. J Behav Med. 2008;31(6):489–497. | ||
Park YH, Kim H, Jang SN, Koh CK. Predictors of adherence to medication in older Korean patients with hypertension. Eur J Cardiovasc Nurs. 2013;12(1):17–24. | ||
Gazmararian JA, Kripalani S, Miller MJ, Echt KV, Ren J, Rask K. Factors associated with medication refill adherence in cardiovascular-related diseases: a focus on health literacy. J Gen Intern Med. 2006;21(12):1215–1221. | ||
Mochari H, Ferris A, Adigopula S, Henry G, Mosca L. Cardiovascular disease knowledge, medication adherence, and barriers to preventive action in a minority population. Prev Cardiol. 2007;10(4):190–195. | ||
DeWalt DA, Hink A. Health literacy and child health outcomes: a systematic review of the literature. Pediatrics. 2009;124 Suppl 3:S265–S274. | ||
Dewalt DA, Berkman ND, Sheridan S, Lohr KN, Pignone MP. Literacy and health outcomes: a systematic review of the literature. J Gen Intern Med. 2004;19(12):1228–1239. | ||
Charles H, Good CB, Hanusa BH, Chang CC, Whittle J. Racial differences in adherence to cardiac medications. J Natl Med Assoc. 2003;95(1):17–27. | ||
Gehi A, Haas D, Pipkin S, Whooley MA. Depression and medication adherence in outpatients with coronary heart disease: findings from the Heart and Soul Study. Arch Intern Med. 2005;165(21):2508–2513. | ||
World Health Organization. Adherence to Long-Term Therapies: Evidence for Action. Geneva, Switzerland: World Health Organization; 2003. | ||
Ho PM, Bryson CL, Rumsfeld JS. Medication adherence: its importance in cardiovascular outcomes. Circulation. 2009;119(23):3028–3035. | ||
Wagner EH, Bennett SM, Austin BT, Greene SM, Schaefer JK, Vonkorff M. Finding common ground: patient-centeredness and evidence-based chronic illness care. J Altern Complement Med. 2005;11 Suppl 1:S7–S15. | ||
Heinrich C, Karner K. Ways to optimize understanding health related information: the patients’ perspective. Geriatr Nurs. 2011;32(1):29–38. | ||
Martin MY, Kohler C, Kim YI, et al. Taking less than prescribed: medication nonadherence and provider-patient relationships in lower-income, rural minority adults with hypertension. J Clin Hypertens (Greenwich). 2010;12(9):706–713. | ||
Blackwell SA, Baugh DK, Montgomery MA, Ciborowski GM, Waldron CJ, Riley GF. Noncompliance in the use of cardiovascular medications in the Medicare Part D population. Medicare Medicaid Res Rev. 2011:1(4). | ||
Zhang Y, Baik SH, Chang CC, Kaplan CM, Lave JR. Disability, race/ethnicity, and medication adherence among Medicare myocardial infarction survivors. Am Heart J. 2012;164(3):425.e4–433.e4. | ||
Nekhlyudov L, Madden J, Graves AJ, Zhang F, Soumerai SB, Ross-Degnan D. Cost-related medication nonadherence and cost-saving strategies used by elderly Medicare cancer survivors. J Cancer Surviv. 2011;5(4):395–404. | ||
Nguyen HG, Chamie K, Nguyen KG, Durbin-Johnson B, Kurzrock EA. Outcomes after pediatric ureteral reimplantation: a population based analysis. J Urol. 2011;185(6):2292–2297. | ||
Atreja A, Bellam N, Levy SR. Strategies to enhance patient adherence: making it simple. Med Gen Med. 2005;7(1):4. | ||
Kenny DA, Veldhuijzen W, Weijden TV, et al. Interpersonal perception in the context of doctor–patient relationships: a dyadic analysis of doctor–patient communication. Soc Sci Med. 2010;70(5):763–768. | ||
American Medical Association. Initiative to Transform Medical Education: Recommendations for Change in the System of Medical Education. Chicago, IL: American Medical Association; 2007. | ||
Harrington J, Noble LM, Newman SP. Improving patients’ communication with doctors: a systematic review of intervention studies. Patient Educ Couns. 2004;52(1):7–16. | ||
Haskard KB, Williams SL, DiMatteo MR, Rosenthal R, White MK, Goldstein MG. Physician and patient communication training in primary care: effects on participation and satisfaction. Health Psychol. 2008;27(5):513–522. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.