Back to Journals » Patient Preference and Adherence » Volume 9
Patient-reported treatment satisfaction and choice of dosing frequency with biologic treatment for moderate to severe plaque psoriasis
Authors Zhang M, Brenneman S, Carter C, Essoi B, Farahi K, Johnson M , Lee S, Olson W
Received 31 March 2015
Accepted for publication 12 May 2015
Published 16 June 2015 Volume 2015:9 Pages 777—784
DOI https://doi.org/10.2147/PPA.S85773
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Johnny Chen
Mingliang Zhang,1 Susan K Brenneman,2 Chureen T Carter,1 Breanna L Essoi,2 Kamyar Farahi,1 Michael P Johnson,2 Seina Lee,1 William H Olson3
1Health Economics and Outcomes Research, Janssen Scientific Affairs, LLC, Horsham, PA, 2Health Economics and Outcomes Research, Optum Life Sciences, Eden Prairie, MN, 3Research and Analysis Strategy, Janssen Scientific Affairs, LLC, Titusville, NJ, USA
Background: Moderate to severe plaque psoriasis has a serious effect on health-related quality of life. Patients treated with biologic medications place importance on satisfaction and treatment frequency options. We assessed patient-reported treatment satisfaction and dosing frequency choice with biologics.
Methods: We used a health care claims database to identify patients with moderate to severe plaque psoriasis. Participants completed the Treatment Satisfaction Questionnaire for Medication. Results were compared between patients experienced with biologics (adalimumab, etanercept, or ustekinumab) or not (cyclosporine or methotrexate). Participants were asked for their choices of dosing options of once every 1–2 weeks, 3–4 weeks, 1–2 months, or 2–3 months. Participants were also asked for their choices of dosing options of every 1, 2, 3, and so on up to every 12+ weeks.
Results: A total of 426 patients completed the survey (263 biologic-experienced and 163 biologic-naïve patients). Patient satisfaction with psoriasis treatment was significantly higher in the biologic-experienced cohort. The most frequently chosen option (38.8% of all participating patients) was every 2–3 months; 37.3% chose once every 1–2 weeks. Significant differences were found in the percentage of biologic-naïve patients choosing 2–3-month (49.7%) over 1–2-week (20.9%) dosing (P<0.001). Among biologic-experienced patients, the difference between the percentage of patients choosing the 2–3-month (35.7%) and 1–2-week (41.8%) options was not significant (P=0.264). The two most often week-specific intervals chosen by biologic-naïve patients were 12+ weeks (42.3%) and 4 weeks (15.6%). The biologic-experienced patients most often chose 12+ weeks (31.2%) and 1 week (25.9%).
Conclusion: Patients using biologics reported satisfaction with their treatment, which may positively affect outcomes. Longer dosing intervals were chosen most frequently among all patients combined. Reports of patient satisfaction with prior treatments and choices regarding dosing frequency, among all other considerations, should be evaluated in determining an appropriate biologic medication for psoriasis.
Keywords: psoriasis, biologic treatment, patient satisfaction, biologic dosing, patient choice
Introduction
Psoriasis is a non-contagious, chronic, systemic, immune-mediated skin disease, which affects 2%–3% of the US population (6–8 million people).1,2 The most prevalent autoimmune disease in the USA,1 psoriasis can present at any age, but primarily affects adult males and females equally.3 Although the impact varies according to disease severity, psoriasis can impose a substantial economic burden, in terms of loss of productivity, disability, and treatment costs.4–9 In addition to economic consequences, the social stigma associated with psoriasis affects social relationships and health-related quality of life.9,10
There is no cure for psoriasis, and only suppressive/remittive therapies are available. In addition, treatment is challenging due to the recurring and remitting nature of psoriasis.11 Traditionally, psoriasis has been treated with topical medications, phototherapy, and conventional systemic medications, but patient satisfaction with these has been low due to side effects, inconvenience, and toxicity.12 Biologic medications have improved treatment of the symptoms of psoriasis and had positive effects on quality of life and clinical outcomes13 and on productivity.14 Biologics eliminate the need for application of messy topical medications and offer the convenience of less frequent dosing (for maintenance, 1–2 times weekly to once every 12 weeks) than other systemic medications.11 Despite recent advances in treatment options, approximately one in three patients in the USA with moderate to severe psoriasis is untreated.15 Furthermore, up to 50% of patients with moderate to severe psoriasis are still treated only with topical medications.15 Thus, non-treatment and under-treatment are significant issues, and dissatisfaction with treatments may be a contributing factor.
Patients treated with biologics place importance on the benefits of treatment and treatment frequency, and have reported higher treatment satisfaction than those on traditional therapy.16 Higher treatment satisfaction is associated with improvement in health-related quality of life.17 Dissatisfaction with treatment can lead to poor adherence and, as a consequence, suboptimal health outcomes.18 Satisfaction, adherence, and outcomes can vary based upon a patient’s prior experience with treatments;10,15,19 switching therapies or increasing the frequency of dosing has been a common approach to inadequate outcomes.20–22 Because of these recent findings, interest is growing in patient-centered approaches to psoriasis treatment, ie, individualized options that incorporate patient preferences.16,23,24 Furthermore, data are scarce on how patient choice of dosing frequency and treatment satisfaction depend on prior experience with biologics. Thus, the objectives of this study were to assess patient-reported treatment satisfaction and patient-reported choice of dosing frequency options among patients with moderate to severe psoriasis and treated with a subcutaneous injectable biologic (adalimumab, etanercept, or ustekinumab) or a non-biologic (cyclosporine or methotrexate) medication. The patient responses were analyzed by whether (biologic-experienced) or not (biologic-naïve) the patients had current or prior experience with biologic treatments.
Patients and methods
Study design
This was a sample survey study using stratified random sampling. We used an administrative health care claims database to identify patients who were taking a subcutaneous injectable biologic (adalimumab, etanercept, or ustekinumab), methotrexate, or cyclosporine for the treatment of moderate to severe plaque psoriasis and to obtain demographic and clinical data. Following identification, patients were invited by mail to participate in a cross-sectional research survey. After providing informed consent, participants completed a paper survey instrument.
Data sources
The study population included data for commercial health plan insured members in the Optum Research Database, representing all US geographic census regions.25 For the study period of 2012–2013, the Optum Research Database had medical and pharmacy data for 12,570,620 patients.
Study sample
The target population in this study were commercial health plan members from the Optum Research Database who had moderate to severe plaque psoriasis, and were identified using claims occurring between January 1, 2012 and July 1, 2013 (identification period). Treatment characteristics were assessed with regard to the 12-month time period prior to the index date (date of the last claim for a systemic [biologic, methotrexate, or cyclosporine] therapy for psoriasis within the identification period).
Inclusion/exclusion criteria
Patients were included if they met all of the following criteria: at least one claim with a diagnosis of psoriasis (ICD-9-CM 696.1) in any position within the identification period;26 at least one claim for methotrexate, cyclosporine, or an injectable biologic (adalimumab, etanercept, or ustekinumab) prescription for treatment of psoriasis within the identification period or 1 year prior to the first diagnosis of psoriasis during the identification period; age 18 years or older; willingness to sign and return the informed consent and health information release forms; and a patient-confirmed diagnosis of psoriasis.
The only exclusion criterion was evidence of any biologic agent use other than adalimumab, etanercept, and ustekinumab during the identification period.
Sampling plan
Potential participants were stratified by claims-based biologic treatment experience (biologic-naïve vs biologic-experienced) before selection for inclusion in the survey. They were flagged for specific psoriasis treatment during the pre-index period as biologic-experienced (current or past experience with a biologic medication) or biologic-naïve (only had experience with methotrexate or cyclosporine).
All patients who had been classified as biologic-naïve were included in the survey study sample (n=901). A random sample (n=1,098) of biologic-experienced patients (from among n=3,396 eligible) was selected using a random-number from a uniform distribution. Each patient record was assigned a value using the RANUNI function in SAS. The data were then sorted by this number and the appropriate number of observations was selected.
A target sample size was determined by the value and desired precision of measured proportions. Because the actual proportions were unknown, the largest sample size required for a precision of ±0.05 for all values of proportions was targeted (n=385).
Data captured
Medical claims included diagnosis of psoriasis (ICD-9-CM 696.1); and pharmacy claims for methotrexate, cyclosporine, or a subcutaneous injectable biologic agent (adalimumab, etanercept, ustekinumab). Demographic characteristics derived from claims data included: sex; age (as of index year); race/ethnicity (White, Black, Native Hawaiian or other Pacific Islander, American Indian or Alaska Native, Asian, Hispanic, other race, or uncoded); and geographic region, with five geographic regions in accordance with the US Census Bureau’s region designations (Northeast, Midwest, South, West, or other).25
Patient characteristics obtained from the survey included weight (in lbs at time of survey); years since diagnosis; self-reported disease severity (number of patient handprint-sized areas covered converted into percentage of skin affected and labeled into categories “very mild”, “mild”, “moderate”, “severe”, and “extremely severe”); self-reported health status (“excellent”, “very good”, “good”, “fair”, and “poor”); and current treatment regimen (methotrexate, cyclosporine, adalimumab, etanercept, or ustekinumab).
Primary outcomes measures
The survey instrument (see Supplementary materials) contained questions designed to assess patients’ choice for biologic maintenance dosing frequency among the options currently available (ie, once every 1–2 weeks, 3–4 weeks, 1–2 months, or 2–3 months); a preferred specific interval period between doses (choice of any whole number between 1 and 12+ weeks between doses); experience with other biologic and/or traditional therapies; and treatment satisfaction (the Treatment Satisfaction Questionnaire for Medication [TSQM-9]).27 The TSQM-9 is a 9-item measure that assesses the most common dimensions patients use to evaluate their medication (ie, global satisfaction, effectiveness, and convenience). The results for each scale are presented from 0 to 100, where higher scores represent better satisfaction.
Statistical analysis
Claims and survey study variables were analyzed descriptively for survey respondents with complete responses. Responses were considered complete if they included completed survey instruments, signed consent and release forms, and confirmation of a diagnosis of psoriasis. Design-based stratified random sampling inference was performed where patients in each stratum were weighted by the inverse probability of a patient meeting the eligibility criteria and returning a complete survey in that stratum.
Numbers and percentages were provided for dichotomous and categorical variables based on the number of subjects who answered the question at hand. Mean and standard error were provided for continuous measures. All comparisons are based on 95% confidence intervals (CIs) unless otherwise noted.
SAS/STAT28 version 9.2 survey procedures for stratified simple random sampling were used. PROC SURVEYMEANS and PROC SURVEYFREQ were used to calculate the statistics. In these analyses, the finite population correction was used so that the inference is to the sampling frame from which samples were taken.
Regulatory considerations
All data were used in compliance with state and federal laws and regulations related to the privacy and security of individually identifiable health information, such as the Health Insurance Portability and Accountability Act Standards for Privacy of Individually Identifiable Health Information. Institutional review board (IRB) approval was obtained from the New England IRB and research review board overseeing studies using the Optum Research Database. These IRBs reviewed and approved the study protocol, survey instruments, patient informed consent form, health information release form, and patient cover letter. All participants provided written informed consent to participate in the study.
Results
Study enrollment and final sample
A total of 1,999 patients were identified in the administrative claims and invited to participate, of whom 54.9% (n=1,098) were biologic-experienced patients (Figure 1). Among the 24.8% (n=495) of patients who responded, 21.3% (n=426) were eligible for analysis (263 biologic-experienced and 163 biologic-naïve). A higher percentage of survey respondents were biologic-experienced than were biologic-naïve (61.7% vs 38.3%).
Demographic and clinical characteristics
Among the participants, a significant difference in mean (± standard deviation) age (P=0.009) existed between biologic-naïve (51±0.8 years) and biologic-experienced (49±0.7 years) participants (Table 1). More biologic-experienced than biologic-naïve patients reported having severe psoriasis (36% vs 23%, respectively, P=0.004), with the mean number of hand-print sized areas with lesions being 8±0.72 vs 5±0.44, respectively (P=0.002). The biologic-naïve cohort contained significantly more Black/African American patients than the biologic-experienced cohort (4% vs 1%, P=0.014), and a shorter time since diagnosis (14 years vs 19 years; P<0.001).
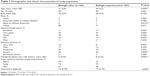  | Table 1 Demographic and clinical characteristics of study population |
Assessment of treatment satisfaction
Mean scores for effectiveness were significantly (P<0.001) higher for biologic-experienced patients (74 [standard error (SE) 1.34], 95% CI 71.4–76.7) than biologic-naïve (60 [1.74], 95% CI 56.3–63.2) patients. Mean global satisfaction was significantly (P<0.001) higher for biologic-experienced (70 [1.33]; 95% CI 67.1–72.3) than biologic-naïve (56 [1.74]; 95% CI 52.9–59.7) patients. The scores for convenience were not significantly different (P=0.625; Figure 2).
Choice of dosing frequency
One survey question was:
If your physician provided you with several options for the frequency of an injection maintenance medication for your psoriasis, which of the following would you request?
The response options were “Once every 1–2 weeks”, “Once every 3–4 weeks”, “Once every 1–2 months”, and “Once every 2–3 months”. Among all patients (biologic-naïve and biologic-experienced, combined), the greatest percentage of respondents (38.8%) chose dosing every 2–3 months (not shown), and the next most often chosen dosing (among all patients) was once every 1–2 weeks (37.3%). A significant difference was found in the percentage of biologic-naïve patients choosing 2–3-month dosing (49.7%) over 1–2-week dosing (20.9%; P<0.001). Among the biologic-experienced patients, the difference between the 2–3-month (37.3%) and 1–2-week options (41.8%) was not significant (P=0.264; Figure 3).
When asked to choose a specific dose interval by number of weeks between doses, 12+ weeks was the interval chosen by the greatest percentage of the respondents overall, and was chosen more by the biologic-naïve patients than the biologic-experienced patients (Figure 4). The two most often week-specific intervals chosen among biologic-naïve patients were 12+ weeks (42.3%) and 4 weeks (16.0%). The biologic-experienced patients most often chose 12+ weeks (31.2%) and 1 week (25.9%).
Discussion
Prior studies have demonstrated greater satisfaction with biologic treatments than other treatment options among patients with psoriasis.10 Our study used patient survey data to explore satisfaction and dosing interval choices in the overall population and in subpopulations of biologic-naïve and biologic-experienced patients. Greater patient satisfaction promotes patient compliance with any medication, and historically, satisfaction with psoriasis treatments has been low.15 A recent study on satisfaction with psoriasis treatments using a version of the TSQM concluded that satisfaction was greater with biologics and traditional systemic medications than with phototherapy or topical drugs.16 In a study that validated the TSQM-9, high correlation coefficients were observed, and in each domain, researchers were able to differentiate between medium and low levels of compliance among respondents. All scores, for effectiveness, convenience, and global satisfaction, were lower among patients with low levels of compliance.27 This validation study established that “the convenience domain had the strongest association with adherence, followed by effectiveness and global satisfaction”.27 In our study, we found the highest satisfaction score was in the convenience domain for all patients, biologic-naïve and biologic-experienced, but the differences between groups was not significant. Thus, we suggest that the higher overall satisfaction in biologic-experienced patients is primarily a function of greater efficacy of biologics.
We found significantly greater satisfaction (global score and effectiveness score) among biologic-experienced patients than biologic-naïve patients. Few studies have examined differences in satisfaction related to prior experience with biologic medications. In 2014, Callis Duffin et al also assessed patient satisfaction via patient survey, using the TSQM-11, and demonstrated greatest satisfaction with biologics (either as monotherapy or combined with methotrexate), over all other treatment options.19 They found a significant correlation between overall satisfaction and Psoriasis Area and Severity Index (ρ=−0.36, P<0.001). The National Psoriasis Foundation Surveys in 2003–2011 found a high (52.3%) treatment dissatisfaction rate among patients with psoriasis.15 The most common reasons patients did not pursue oral systemic or injected biologic treatments were related to side effects. The least common self-reported reasons were related to failing such treatments in the past.15 Our results suggest a possible relationship between experience with biologics and higher satisfaction scores. There are many factors for a patient to consider in selecting a treatment for psoriasis, including efficacy, side effects, convenience, and cost. Our results suggest that published reports regarding satisfaction with treatment and patient choice of dosing frequency should also be among the factors considered. In our study, the greatest percentage of patients (among both cohorts combined) chose the longest interval available (every 2–3 months; or specifically every 12 weeks) between doses of biologic treatments, and this longer interval option was chosen by more biologic-naïve patients than biologic-experienced patients. More frequent dosing was chosen more often (between 1-week and 4-week intervals) by biologic-experienced patients than biologic-naïve patients. However, the difference is not statistically significant. We do not know the reasons behind the difference in choice of dosing interval based on prior experience. Ours is the first study to examine patient-reported dosing schedule choices in psoriasis; only one published study compared actual dosing between biologic-naïve and biologic-experienced patients. In 2014, Cao et al29 performed a retrospective observational study to evaluate treatment patterns and found similar dosing patterns between biologic-naïve and biologic-experienced patients, both consistent with prescribing guidelines, but with no assessment of patient choice of frequency. The differences seen in our study are noteworthy, especially considering patients’ prior experience with biologics, and provide a basis for more detailed study of the possible impact of patient choice on adherence with (and ultimately success of) any treatment option.
Limitations
Some studies may be hindered by errors found in administrative claims databases, but the inclusion criteria were few in this study, which should limit the impact of coding errors. In addition, the presence of a diagnosis claim alone is not proof of diagnosis; to lessen the impact of such a limitation, the diagnoses of psoriasis found in the claims database were confirmed by patient self-report. Further, we used patient assessment of severity, rather than physician determination of severity, but this should not have affected our results because our assignment to groups was based only on the presence of biologic or no biologic experience, rather than severity. The fact that the biologic-experienced group reported greater severity is consistent with prescribing indications, in that biologics are usually prescribed for more severe cases that would not have responded well to other treatments.
We did not evaluate differences in satisfaction or frequency choices, based upon psoriasis severity, age, current therapy frequency, or other possible confounders obtainable via the claims database. Future studies should provide for multivariate analyses to determine the possible influences of demographic or clinical characteristics on survey findings. The possibility always exists that an important factor which could influence the results is simply unavailable or not included in the database or survey used for this study. For example, side effects that may have influenced a patient’s satisfaction were not specifically explored.
Comparisons with other survey studies on psoriasis are limited by variation in survey instruments, which are commonly used to assess satisfaction with medications. The TQSM-9 is a validated, shorter version of previous versions, one of which has been used in a previous study of psoriasis.19 No significant differences would be expected between the results obtained from this population and the overall population of patients with psoriasis but, as with any survey-based study, there is a chance that patients who respond to the survey are different from patients who do not respond. Finally, these findings may not be generalizable to those that might be obtained among patients enrolled in a different health care system.
Conclusion
Overall, patient satisfaction with biologic treatment of psoriasis is good among patients who have previously tried or are currently receiving a biologic treatment. We conclude that patients’ choices regarding dosing schedule and treatment satisfaction should be included among all other considerations in determining an appropriate treatment for psoriasis. It will be helpful in the future to determine the factors associated with greater satisfaction and specific dosing schedule choices.
Acknowledgment
Optum Inc received funding from Janssen Scientific, LLC, to conduct the research, analysis, and assist in developing the manuscript. Medical writing support was provided by Caroline Jennermann, an employee of Optum Inc.
Disclosure
MZ, CC, KF, SL, and WHO are employees of Janssen Scientific, LLC. SKB, BE, and MPJ are employees of Optum Inc. The authors report no other conflicts of interest.
References
National Psoriasis Foundation. Moderate to severe psoriasis and psoriatic arthritis: biologics. Available from: http://www.psoriasis.org/about-psoriasis/treatments/biologics. Accessed March 27, 2015. | ||
Rachakonda TD, Schupp CW, Armstrong AW. Psoriasis prevalence among adults in the United States. J Am Acad Dermatol. 2014;70(3):512–516. | ||
National Institute of Arthritis and Musculoskeletal and Skin Diseases. Questions and answers about psoriasis. October 2013. Available from: http://www.niams.nih.gov/Health_Info/Psoriasis/. Accessed March 27, 2015. | ||
Navarini AA, Laffitte E, Conrad C, et al. Estimation of cost-of-illness in patients with psoriasis in Switzerland. Swiss Med Wkly. 2010;140:85–91. | ||
Driessen RJ, Bisschops LA, Adang EM, Evers AW, Van De Kerkhof PC, De Jong EM. The economic impact of high-need psoriasis in daily clinical practice before and after the introduction of biologics. Br J Dermatol. 2010;162:1324–1329. | ||
Ghatnekar O, Ljungberg, Wirestrand LE, Svensson A. Costs and quality of life for psoriatic patients at different degrees of severity in southern Sweden – a cross-sectional study. Eur J Dermatol. 2012;22:238–245. | ||
Ekelund M, Mallbris L, Qvitzau S, Stenberg B. A higher score on the Dermatology Life Quality Index, being on systemic treatment and having a diagnosis of psoriatic arthritis is associated with increased costs in patients with plaque psoriasis. Acta Derm Venereol. 2013;93:684–688. | ||
Levy AR, Davie AM, Brazier NC, et al. Economic burden of moderate to severe plaque psoriasis in Canada. Int J Dermatol. 2012;51:1432–1440. | ||
Lewis-Beck C, Abouzaid S, Xie L, Baser O, Kim E. Analysis of the relationship between psoriasis symptom severity and quality of life, work productivity, and activity impairment among patients with moderate-to-severe psoriasis using structural equation modeling. Patient Pref Adherence. 2013;7:199–205. | ||
Feldman SR, Malakouti M, Koo JY. Social impact of the burden of psoriasis: effects on patients and practice. Dermatol Online. 2014;20(8). pii:13030/qt48r4w8h2. | ||
Sandoval LF, Feldman SR. Biologics in practice: adherence to biologic therapy in psoriasis. Dermatologist. 2013;21(2):30–34. | ||
Finlay AY, Ortonne JP. Patient satisfaction with psoriasis therapies: an update and introduction to biologic therapy. J Cutan Med Surg. 2004;8(5):310–320. | ||
Norlin JM, Steen Carlsson K, Persson U, Schmitt-Egenolf M. Resource use in patients with psoriasis after the introduction of biologics in Sweden. Acta Derm Venereol. 2015;95(2):156–161. | ||
Uhlenhake EE, Mehregan DA. Ustekinumab: differential use in psoriasis. Clin Cosmet Investig Dermatol. 2011;4:93–99. | ||
Armstrong AW, Robertson AD, Wu J, Lebwohl MG. Undertreatment, treatment trends, and treatment dissatisfaction among patients with psoriasis and psoriatic arthritis in the United States: findings from the National Psoriasis Foundation surveys, 2003–2011. JAMA Dermatol. 2013;149(10):1180–1185. | ||
Schaarschmidt M-L, Umar N, Schmider, A, et al. Patient preferences for psoriasis treatments: impact of treatment experience. J Eur Acad Dermatol Venereol. 2012;147(11):1285–1294. | ||
de Korte J, Sprangers MA, Mombers FM, Bos JD. Quality of life in patients with psoriasis: a systematic literature review. J Investig Dermatol Symp Proc. 2004;9:140–147. | ||
Barbosa CD, Balp MM, Kulich K, Germain N, Rofail D. A literature review to explore the link between treatment satisfaction and adherence, compliance, and persistence. Patient Prefer Adherence. 2012;6:39–48. | ||
Callis Duffin K, Yeung H, Takeshita J, et al. Patient satisfaction with treatments for moderate-to-severe plaque psoriasis in clinical practice. Br J Dermatol. 2014;170(3):672–680. | ||
Puig L. Treatment of moderate to severe plaque psoriasis with biologics: analysis of the additional cost of temporary dose escalation vs switch to another biologic after failure of maintenance therapy. Actas Dermosifiliogr. 2014;105(4):401–412. | ||
Degli Esposti L, Sangiorgi D, Perrone V, et al. Adherence and resource use among patients treated with biologic drugs: findings from BEETLE study. Clinicoecon Outcomes Res. 2014;6:401–407. | ||
Ayala F, Lambert J; on Behalf of the TANGO Study Group. Efficacy, tolerability and safety of switching from etanercept to infliximab for the treatment of moderate-to-severe psoriasis: a multicenter, open-label trial (TANGO). J Dermatolog Treat. 2014;18:1–8. | ||
Umar N, Yamamoto S, Loerbroks A, Terris D. Elicitation and use of patients’ preferences in the treatment of psoriasis: a systematic review. Acta Derm Venereol. 2012;92(4):341–346. | ||
Carter C, Schenkel B, Freedman D, et al. An approach to patient-centered care for patients with psoriatic arthritis. J Am Acad Dermatol. 2013;68(4):AB192. | ||
United States Census Bureau. US Department of Commerce, Economics, and Statistics Administration. Census Regions and Divisions of the United States. Available from: http://www2.census.gov/geo/pdfs/maps-data/maps/reference/us_regdiv.pdf. Accessed March 27, 2015. | ||
Centers for Disease Control and Prevention. International Classification of Diseases, Ninth Revision, Clinical Modification. Last revision 2013. Available from: http://www.cdc.gov/nchs/icd/icd9cm.htm. Accessed March 27, 2015. | ||
Bharmal M, Payne K, Atkinson MJ, Desrosiers MP, Morisky DE, Gemmen E. Validation of an abbreviated Treatment Satisfaction Questionnaire for Medication (TSQM-9) among patients on antihypertensive medications. Health Qual Life Outcomes. 2009;7:36. | ||
SAS Institute Inc. SAS/STAT® 9.2 User’s Guide. Cary, NC, USA: SAS Institute Inc; 2008. | ||
Cao Z, Carter C, Wilson KL. Ustekinumab dosing, persistence, and discontinuation patterns in patients with moderate-to-severe psoriasis. J Dermatolog Treat. February 20, 2014. [Epub ahead of print]. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.