Back to Journals » Research and Reports in Neonatology » Volume 4
Oxygen resuscitation and oxidative-stress biomarkers in premature infants
Authors Kumar VH, Carrion V, Wynn KA, Nielsen L, Reynolds AM, Ryan RM
Received 18 February 2014
Accepted for publication 25 March 2014
Published 23 May 2014 Volume 2014:4 Pages 91—99
DOI https://doi.org/10.2147/RRN.S62679
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Video abstract presented by Vasanth HS Kumar.
Views: 686
Vasanth HS Kumar,1 Vivien Carrion,1 Karen A Wynn,1 Lori Nielsen,1 Anne Marie Reynolds,1 Rita M Ryan2
1Department of Pediatrics, The Women and Children's Hospital of Buffalo, Buffalo, NY, 2Department of Pediatrics, Medical University of South Carolina, Charleston, SC, USA
Background: Resuscitation of premature infants with 100% O2 may initiate significant oxidant stress during development, predisposing them to bronchopulmonary dysplasia. In the study reported here, we examined the effects of three different oxygen concentrations at resuscitation on oxygen saturations (SpO2) and oxidant stress in premature infants.
Study design: Infants <32 weeks gestational age were randomized to 21%, 40%, or 100% O2 and resuscitated as per 2005 neonatal resuscitation guidelines. Oxygen groups and SpO2 were unmasked at 10 minutes of age and FiO2 adjusted to maintain an SpO2 of 85%–95% for the next 20 minutes. Blood was collected at 24 hours, 1 week, and 4 weeks for measurement of the oxidative-stress markers, such as a reduced glutathione (GSH) to oxidized glutathione (GSSG) ratio (GSH/GSSG), nitrotyrosine levels, and 8-hydroxydeoxyguanosine (8-OHdG) levels. The study was stopped at 30% enrollment following publication of the 2010 neonatal resuscitation guidelines.
Results: We enrolled 18 patients during the study period. SpO2 increased over time (P<0.0001); however, this increase was not different among the three oxygen groups in the first 10 minutes after birth. FiO2 was significantly higher in the 100% O2 group, despite weaning (P<0.02) to maintain target saturations at 30 minutes of age. The GSH/GSSG ratio was significantly lower in the 100% O2 group at 24 hours than in the other groups (P<0.01). Plasma nitrotyrosine was significantly higher in the 40% and 100% O2 groups over time (P<0.01). Levels of 8-OHdG were significantly higher at 4 weeks compared with at 24 hours, independent of the oxygen group (P<0.0001).
Conclusion: In this study, we defined the natural evolution of SpO2 in the first 10 minutes of life with exposure to three different concentrations of oxygen. Randomization to higher FiO2 led to higher total oxygen exposure at resuscitation, and this was significantly correlated with markers of systemic oxidant stress.
Keywords: oxygen saturation, systemic oxidant stress, GSH/GSSG ratio, nitrotyrosine, resuscitation
Introduction
The transition from fetal to neonatal life in premature infants <32 weeks gestational age (GA) often requires some form of resuscitation, including administration of O2. However, defense mechanisms against high levels of oxygen exposure, such as antioxidant enzyme systems, are induced late in gestation1 and premature infants are not prepared to face the challenge of oxidative stress from relative hyperoxia.2,3 Resuscitation with 100% O2 at birth induces inflammation, free-radical production, and reduced antioxidant defenses in the lungs,4 heart,5 and brain.6 Conversely, the resuscitation of premature infants with oxygen of low concentration results in lower systemic oxidative stress, inflammation, and incidence of bronchopulmonary dysplasia (BPD).7 Prolonged oxidative stress8 and adverse effects on mortality9,10 have been reported in term newborn infants resuscitated in 100% O2 compared with those resuscitated in room air.
We have shown that ventilated premature lambs (born at 128 days, with lungs similar to 28 weeks’ gestation) are unable to appropriately increase antioxidant enzyme activity in response to hyperoxia, and exposure to O2 aggravates systemic oxidant stress, oxidant lung injury, and pulmonary arterial contractility in lambs.11 Oxidative stress plays a role in the development of BPD with immature lungs being particularly sensitive to injurious effects of oxygen and mechanical ventilation.12 Free radicals were elevated in the plasma within 24 to 48 hours after birth,13 and in the bronchoalveolar lavage within a week,14 in premature infants who subsequently developed BPD. Plasma nitrotyrosine (NT), a marker of peroxynitrite-mediated oxidant stress is increased in the first month in infants who develop BPD;15 however, there is a paucity of literature on NT as related to oxygen resuscitation at birth. Oxygen concentrations at resuscitation may determine the degree of oxidative stress in premature neonates with decreased ability to induce antioxidant enzymes. This may trigger an inflammatory response by pro-inflammatory cytokines leading to the development of BPD. In the current study, we tested the hypothesis that limiting oxygen exposure at resuscitation in premature infants <32 weeks GA would decrease systemic oxidative stress as assessed by reduced glutathione (GSH) to oxidized glutathione (GSSG) ratio (GSH/GSSG), plasma NT, and 8-hydrodeoxyguanosine (8-OHdG) at 24 hours, 1 week, or 4 weeks of age. We studied the clinical attributes in these infants, as reducing oxygen exposure should improve these outcomes. We randomized infants <32 weeks GA to receive one of three specified concentrations of O2 (21%, 40%, or 100% O2) during resuscitation for the first 10 minutes of life. The study was conducted prior to the 2010 AHA guidelines on neonatal resuscitation20 and the purpose was to demonstrate whether premature infants <32 weeks GA could be resuscitated successfully in 21% or 40% O2 and to correlate various oxygen exposures at birth with biomarkers of oxidative stress.
Methods
This study was a prospective, double-blind randomized controlled trial of the administration of three specific oxygen concentrations at birth in infants <32 weeks GA. Infants were enrolled from March 2009 to November 2010 at the Women & Children’s Hospital of Buffalo, New York, following institutional review board approval and written parental informed consent prior to delivery. Enrolled infants were randomized to receive 21%, 40%, or 100% O2 at resuscitation. Infants with known congenital or chromosomal anomalies were excluded from the study.
Immediately after birth, infants were placed on a radiant warmer and resuscitated as per 2005 Neonatal Resuscitation Program (NRP) guidelines by the AHA/AAP.19 Respiration, heart rate (HR), and color were evaluated at 30 seconds of age, after drying, stimulation, and repositioning of the infant. The study gas (21%, 40%, or 100% O2) assigned to each infant by randomization was delivered via a T-piece resuscitator (Neopuff™ Infant T-Piece Resuscitator; Fisher and Paykel, Auckland, New Zealand) to provide assisted ventilation as needed. The personnel in the delivery room (DR) (and all but one of the study personnel) were blinded to the study gas FiO2. Neonates who showed signs of increased difficulty in breathing initially underwent ventilation by continuous positive-airway pressure (5–7 cm H2O) with the T-piece resuscitator; positive-pressure ventilation (PPV) with facemask was followed by endotracheal intubation if needed, for lack of clinical response. Infants needing PPV were initiated with a peak inspiratory pressure of 18–20 cm of H2O, peal end expiratory pressure of 5 cm of H2O, and a rate of 30 to 40 per minute. Oxygen (21%, 40%, or 100% O2) was provided with the blender at flow rates of 8 L/min, via the T-piece resuscitator, and the peak inspiratory pressure was adjusted depending on chest rise, color, or the HR. For infants breathing spontaneously with a HR >100, the study gas was used to provide free-flow oxygen if needed, until they established regular respirations. Infants were switched to 100% O2 (and unmasked) only if they were not responding to the study gas (HR <100/min for >90 seconds) despite adequate ventilation at any time after birth and were excluded from the study. However, no infant received chest compressions or crossed over to 100% O2 during the study period.
Soon after birth, a preductal pulse oximeter probe was placed on the infant’s right hand by the study coordinator and connected to the pulse oximeter (Masimo Radical 7 SET Oximeter, Masimo Corporation, Irvine, CA, USA) to measure SpO2. Neonatal Hi-Fi sensors (LNOP Neo Masimo SET; Masimo Corporation) were used with 2-second averaging to achieve maximal sensitivity. SpO2 was recorded every 15 seconds for the first 30 minutes of life. SpO2 recordings were considered reliable when simultaneous readings of apical HR and the monitor HR were the same. Reliable SpO2 readings were established generally within 60 seconds of the birth of the infant.
The FiO2 determined at randomization was kept constant for the initial 10 minutes after birth. For the initial 10 minutes, both the FiO2 concentration and the SpO2 recordings were blinded from the resuscitation team and unmasked at 10 minutes of life. We continued the study gas as long as the SpO2 was in the target range of 85%–95%, and transferred the infant to the neonatal intensive care unit (NICU) in a transport isolette with the respiratory support required. FiO2 was decreased for SpO2 >95% and increased for SpO2 <85%, by 10%–20% every 60 seconds to maintain the SpO2 target of 85%–95%. The intervention portion of the study was complete at 30 minutes of life and the FiO2 was adjusted to maintain an SpO2 of 88%–94% as per NICU protocol at the time. Total oxygen exposure was calculated by summation of the products of “supplemental oxygen” and the duration of FiO2 for each study infant (30 minutes) to arrive at integrated excess FiO2 – that is, Σ(FiO2 – 0.21) × time (minutes).2 This measurement was then correlated with biomarkers of oxidative stress. The study was stopped in December 2010 due to implementation of the 2010 NRP guidelines. The new guidelines stated clearly that 100% oxygen should not be used as the starting FiO2 during resuscitation, so we felt we could no longer randomize infants to that oxygen concentration.
Biochemical measurements of oxidative stress
Systemic oxidant stress was measured by reduced GSH/GSSG ratio, NT, and 8-OHdG in the blood. The GSH/GSSG ratio is a useful indicator of oxidative stress and also measures the effectiveness of antioxidant intervention in whole blood. NT is an indicator of peroxynitrite formation in biological systems subject to oxidative stress, and the presence of 8-OHdG is the most common indicator of oxidative DNA damage. Blood was collected at 24 hours, 1 week, and 4 weeks of age from the central catheter (arterial or venous) or by a venous stick if a central catheter was not in place. Plasma 8-OHdG was measured at 24 hours and at 4 weeks of age.
GSH/GSSG assay
For the measurement of GSSG, 10 μL of 1-methyl-2-vinylpyridinium trifluoromethanesulfonate (M2VP), a thiol-scavenging reagent was added to 100 μL of whole blood. M2VP rapidly scavenges GSH in whole blood. Similarly, 50 μL of whole blood was collected in a micro-centrifuge tube for GSH measurements. The samples were stored at −80°C until the assay was performed. Calorimetric determination of reduced GSH and oxidized GSSG was performed using a Bioxytech® GSH/GSSG-412 assay kit (OxisResearch, Portland, OR, USA).
NT assay
The protein nitrotyrosine content in the sample plasma was determined by comparison with a standard curve prepared from predetermined nitrated bovine serum albumin standards. This was a competitive immunoassay for the quantitative measurement of NT in plasma (OxiSelect™ Nitrotyrosine ELISA [enzyme-linked immunosorbent assay] Kit, STA-305; Cell Biolabs, Inc., San Diego, CA, USA).
8-OHdG assay
The OxiSelect™ DNA Damage ELISA kit (STA-320; Cell Biolabs, Inc.) is a competitive enzyme immunoassay developed for rapid detection and quantitation of 8-OHdG in serum. The quantity of 8-OHdG in a sample was determined using this kit by comparing its absorbance with that of a known 8-OHdG standard curve.
Data collection to assess primary and secondary study outcomes
The primary outcome of the study was GSH/GSSG ratio at 24 hours of age. Based on our preterm lab studies, to detect a difference of 1.5 with a standard deviation (SD) of 1.5 in GSH/GSSG ratio at 24 hours with an alpha level of 0.05 and power of 80%, it was estimated that each group would require 20 patients. The three oxygen groups were stratified into two subgroups (23–27 6/7 weeks; 28 0/7–31 6/7 weeks) and infants were randomized within stratified groups to ensure homogeneity among the groups (21%, 40% and 100% O2).
Although not powered for these secondary outcomes, we also collected data regarding mortality, BPD (oxygen requirement at 36 weeks), necrotizing enterocolitis (NEC; stage II or higher), patent ductus arteriosus (PDA), and intraventricular hemorrhage (IVH) in these infants. All data are expressed as mean ± SD, with “n” being the number of infants in each group. Student’s t-test was used to analyze certain characteristics such as intubation and GA among the oxygen groups, and to analyze plasma 8-OHdG at 24 hours and 4 weeks in the three oxygen groups. The three oxygen groups were compared by one-way analysis of variance (ANOVA). When the overall comparison was significant, differences between individual groups were analyzed using the Tukey–Kramer method (with SAS software version 9.2 [SAS Institute, Cary, NC, USA]). A P-value of <0.05 was considered significant.
Results
We enrolled 18 infants during March 2009 through November 2010 and the study was stopped December 2010 with the implementation of 2010 AHA guidelines on neonatal resuscitation. Six infants were randomized to resuscitation with 21% O2, seven infants with 40% O2, and five infants with 100% O2 (Figure 1). Baseline characteristics, respiratory support at birth, blood gas on admission to the NICU, and total oxygen exposure in the three groups are shown in Table 1. Infants in the 100% O2 group were trending to be of lower GA (Table 1); however, this was not significant (P=0.3). There were no differences in birth weight or other characteristics among the three O2 resuscitated groups (Table 1). More infants in the 100% O2 resuscitated group were intubated and administered surfactant in the DR than in the other two groups (Table 1; 80% in the 100% O2 group, 43% in the 40% O2 group, and 17% in the 21% O2 group). Infants who were intubated had a significantly lower GA (27.2±2.1 vs 30.1±1.4; P<0.003). However, there was no significant difference in intubated patients among the oxygen groups (P=0.06). There were no differences in blood-gas parameters, such as pH, PaCO2, PaO2, and base deficit, as assessed at 60 minutes after birth among the three groups (Table 1). Total oxygen exposure during the study period was significantly different among the groups: the 100% O2 group had the highest oxygen exposure (P<0.0001 vs 21% O2 and 40% O2; ANOVA) and the 21% O2 group had the lowest oxygen exposure (P<0.001 vs 40% O2) (Table 1).
  | Figure 1 Trial flow chart displaying the distribution of infants during the study period. |
FiO2 and SpO2 values
Figure 2 illustrates the mean SpO2 values in the first 10 minutes of life in the three oxygen resuscitated groups. The mean SpO2 values were 50%, 53%, and 69% at 1 minute; 77%, 83%, and 95% at 5 minutes; and 92%, 92%, and 98% at 10 minutes in the 21% O2, 40% O2, and 100% O2 groups, respectively (Figure 2). There was no significant difference in SpO2 among the three oxygen groups at any given minute in the first 10 minutes of life. However, there was a trend toward significance at 5 minutes of life among the groups (P=0.06). SpO2 significantly increased over time in the first 10 minutes of life in all the three oxygen groups (P<0.0001; mixed-model ANOVA). However, oxygen groups alone (P=0.08) or in combination with time (P=0.36), were not significantly correlated with SpO2 in the first 10 minutes after birth. Resuscitation of premature infants with 100% O2 resulted in SpO2 values above the upper limit of the 2010 guidelines in the first 10 minutes after birth (Figure 2). The 40% O2 resuscitated group had SpO2 values below the NRP lower limit in the first 5 minutes and within the range by 6–10 minutes of age (Figure 2). Similarly, the 21% O2 resuscitated group had mean SpO2 values bordering the NRP lower limit in the first 5 minutes and within the NRP-defined SpO2 target range from 6 to 10 minutes. There were no differences in SpO2 among the groups at 10 and 30 minutes of life.
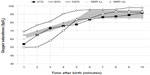  | Figure 2 Oxygen saturations (SpO2) in premature infants <32 weeks gestational age during the first 10 minutes after birth in the three resuscitated groups. Oxygen was kept constant for the first 10 minutes at either 21% O2 ( |
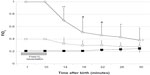
FiO2 was weaned to maintain SpO2 in the target range of 85%–95% from 10 minutes of age. Infants in the 21% O2, 40% O2, and 100% O2 groups were weaned to 24.8% (±5), 27.9% (±6), and 38% (±20) O2, respectively, at 30 minutes of age (Figure 3). Despite aggressive weaning, FiO2 was significantly higher in the 100% O2 group to maintain the target SpO2 until 30 minutes of age (P<0.02 vs 40% O2 and 21% O2 groups; ANOVA). There was no significant difference in FiO2 between the 40% O2 and 21% O2 groups during the weaning process (Figure 3). HR following resuscitation increased significantly over time in the first 10 minutes in all the three oxygen groups (P<0.0001, ANOVA), although this was not significant among them.
Oxygen resuscitation and oxidative-stress markers
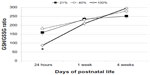
Over time, whole-blood GSH concentrations were significantly higher in the 21% O2 group compared with the 40% O2 and 100% O2 groups (P<0.01 vs the 40% and 100% O2 groups; two-way ANOVA; Table 2). Blood GSSG levels were significantly higher at 24 hours in the 100% O2 group compared with the other two groups (P<0.01); however, this was not different over time (1 week and 4 weeks) among the groups (Table 2). The GSH/GSSG ratio was significantly lower at 24 hours in the 100% O2 group compared with the 21% O2 and 40% O2 groups (P<0.01; Table 2), suggesting higher oxidative stress in this group (Figure 4). The ratio was not different among the groups at 1 week or at 4 weeks of age.
Plasma NT, a marker of peroxynitrite formation, was higher in the two oxygen resuscitated groups over time (Figure 5A) (P<0.01 vs the 40% O2 group; P<0.001 vs 100% O2 group). Also, the 100% O2 group had higher NT compared with the other two groups at 24 hours (P<0.01; Figure 5A). Levels of 8-OHdG were similar at 24 hours and at 4 weeks among the groups; however, they were significantly higher at 4 weeks compared with at 24 hours among the groups (P<0.0001*; Figure 5B).
Secondary outcomes
There were no significant differences in any of the secondary outcomes measured in the study. The incidence of any IVH was 40% in the 100% O2 group (bilateral Grade I in one infant and I/II in another) and none in the other groups. We had one infant with significant PDA in each of the 40% O2 and 100% O2 groups. The incidence of BPD was 16% (1/6), 42% (3/7), and 60% (3/5) in the 21% O2, 40% O2, and 100% O2 groups, respectively. Infants in the 21% O2 group were ventilated for a mean of 2.6 (±5.6) days compared with 7.3 (±10) days in the 40% O2 group and 26.4 (±27.3) days in the 100% O2 group; this was not significant among the groups (P=0.06). One infant in the 21% O2 group and one in the 40% O2 group died, while no infants in the 100% O2 group died. The combined outcome for BPD, NEC, or death was 50% (3/5), 71% (5/7), and 100% in the 21% O2, 40% O2, and 100% O2 resuscitated groups, respectively.
Discussion
Multiple studies have addressed oxygen administration at resuscitation by variation in oxygen titration strategies in the first 10 minutes after birth.16–18 The novelty of our study was in modifying this approach to allow for a fixed concentration of oxygen at resuscitation and, in addition, blinding the study gas for the first 10 minutes irrespective of the SpO2, adding value to our results. The major findings include derangement of markers of oxidative stress at 24 hours (GSH/GSSG ratio) and over time (NT), and this could be affected by total oxygen exposure at birth.
The study was designed originally when the 2005 NRP guidelines were in place, at which time the recommendations were to resuscitate premature infants between 21% and 100% O2, and for a graded increase or decrease in O2 using blender, with no defined target saturation for the first 10 minutes of age19 and no prescribed starting FiO2. Our original enrollment target of 60 patients with 20 infants in each arm was not met during the study period. Low enrollment was mostly due to exclusion of emergent deliveries and lack of appropriate study personnel (who we felt were necessary for this study) in place physically at the time of delivery, which limited our capacity to utilize every birth. Unfortunately, we discontinued the study to stay current with the changes to the neonatal resuscitation guidelines (titrating oxygen for a targeted pre-ductal SpO2) in 2010,20 adding to incomplete and low enrollment. Despite these limitations, the study is useful, as we report for the first time the natural evolution of SpO2 in the first 10 minutes of life during resuscitation with different concentrations of fixed levels of oxygen, including 21% O2, and how this relates to biomarkers of systemic oxidative stress in infants <32 weeks GA.
Requirement for endotracheal intubation was associated with a more premature GA, regardless of the oxygen group, suggesting prematurity as a major factor in PPV/intubation in the 100% O2 group. All infants in the 100% O2 group received PPV/intubation in the first 2 minutes of life, which means that intubation was likely due to hypoxia or ventilation issues rather than secondary to apnea from relative and prolonged hyperoxia. The contrast in total oxygen exposure is striking; however, that is mostly by design. Beginning resuscitation with high oxygen such as 100% O2 resulted in a mean (SD) oxygen load of 38% (±20), despite aggressive weaning by 30 minutes.
Despite limited subject enrollment, the study increases our understanding of the natural evolution of SpO2 when exposed to three different static oxygen concentrations in the first 10 minutes of life. SpO2 values in the 100% O2 group were higher compared with the NRP upper limit, suggesting that 100% O2 is probably not the right concentration for resuscitating premature infants to meet 2010 guidelines on targeted preductal SpO2 at birth. There were no significant differences in SpO2 between the 21% O2 and 40% O2 groups. Resuscitation with either 21% O2 or 40% O2 resulted in SpO2 within the NRP targeted range, especially from 6 to 10 minutes of life. This suggests that premature infants can probably be weaned to 21% O2 by 6 minutes of life. It is hard to justify 21% O2 in the first 5 minutes of birth with the small number of infants in our study. GA may be an important factor influencing O2 resuscitation at birth, as extremely premature infants (<26 weeks GA) will probably need some oxygen initially and infants >28 weeks GA may escape oxygen to maintain SpO2 within the defined targeted range. Multiple studies have addressed the issue by initial oxygen exposure followed by frequent titration to maintain a specific SpO2 range at resuscitation. Titrating from an initial concentration of 100% O2 was more effective than giving a static concentration of 100% O2 in maintaining preterm infants in a target SpO2 (85–92) in the first 10 minutes after birth. However, resuscitation with 21% O2 resulted in a high treatment-failure rate.17 A previous study has reported that infants resuscitated with 21% O2 failed to achieve a set target saturation and all infants in the room-air group needed oxygen by 3 minutes of age.18 However, resuscitation can be safely initiated in infants <28 weeks GA with a lower FiO2 (30% O2), which then can be adjusted to the infant’s needs, reducing the oxygen load to the neonate.16 Also, infants randomized to 30% O2 (compared with to 90% O2) at birth and then titrated to maintain a specific saturation, had lower oxidative stress and reduced incidence of BPD.7
In our study, resuscitation with 100% O2 was associated with a significantly higher GSSG and a lower GSH/GSSG ratio, indicative of oxidative stress at 24 hours of age; however, this effect was not sustained at 4 weeks of age. The absence of any difference in GSH/GSSG at 4 weeks among the groups may in part be due to lack of asphyxial insult or prematurity in these infants, as this has previously been demonstrated in term asphyxiated infants.8 However, in preterm infants with mild to moderate asphyxia, total hydroperoxide was significantly higher and redox potential to total hydroperoxide ratio was lower in the 100% O2 group compared with in the reduced O2 resuscitated group, indicating that oxidative stress can be reduced by lowering the inspired oxygen concentration.2 Resuscitation of premature infants with 30% O2 also decreased oxidative stress, as measured by GSSG/GSH ratio on days 1 and 3 of life, compared with 90% O2 resuscitation.7 Urinary markers of oxidative stress were also higher in the high-oxygen group, suggesting the detrimental effects of oxygen load at resuscitation.7
In the present study, plasma NT was significantly higher in the 100% O2 and 40% O2 resuscitated groups over time. The presence of nitrated proteins in the plasma may indicate either inflammation or the formation of peroxynitrite from nitric oxide and superoxide.21 In a case-control study, infants who developed BPD had a significantly higher plasma NT on the first day of life than infants who did not develop BPD.15 Although our study is limited by small numbers, more infants in the 100% O2 group developed BPD compared with in the other two groups. Plasma 8-OHdG increased over time; however, levels were not different among the oxygen groups. This may be related to similar birth weight and GA among the groups, as plasma 8-OHdG at birth has been shown to be negatively correlated with birth weight and GA.22 There is a paucity of literature on plasma 8-OHdG measurements as they relate to oxygen and oxidative DNA damage in the newborn. However, urinary elimination of oxidized guanosine, as measured by 8oxodG/2dG ratio, was higher in the first week in the high-oxygen group, implying oxygen at birth induces DNA damage.7 Further, 8-OHdG levels determined by ELISA are not highly specific, unlike when determined by mass spectrometry, which may explain the lack of association with the oxygen groups in our study.
We found no significant differences in SpO2 among the three oxygen groups in the first 10 minutes after birth; however, we found difference in oxidative-stress markers among the groups at 24 hours and 4 weeks of age. The SpO2 in the 100% O2 group was well above the NRP upper limit, whereas that in the 40% O2 and the 21% O2 groups bordered the NRP lower limit. Smaller changes in SpO2 are associated with larger changes in arterial PaO2, an optimal measure of assessing oxygenation. Measurement of SpO2, although noninvasive, has reduced sensitivity to hyperoxemia, more so in the first 10 minutes after birth when the relationship between FiO2 and SpO2 is not well established. Also, the 100% O2 group had higher O2 exposure by 30 minutes of age compared with the other two groups. This could explain a significantly higher GSSG, lower GSH/GSSG ratio, and higher NT in the plasma at 24 hours of age. However, subsequent O2 exposure and lung immaturity may have triggered an inflammatory response leading to the development of BPD. This is probably the reason for subsequent elevation of plasma NT in the 40% and 100% O2 groups at 4 weeks. The oxidative and nitrosative stress may also be related to a host of factors – including, among others, hypoxic episodes;23 sex;24 antenatal steroids;24 days on mechanical ventilation; and severity of lung disease, especially in chronically ventilated infants.
Conclusion
Although multiple studies have addressed issues involving oxygen at resuscitation, the novelty of our study was in keeping the oxygen concentration constant at resuscitation. This has helped us to define the natural evolution of SpO2 in the first 10 minutes to three different oxygen concentrations. We have shown that oxygen at resuscitation and total oxygen exposure correlates significantly with markers of oxidant and nitrosative stress. Despite the low number of infants enrolled, the study adds to the literature regarding the role of oxygen at resuscitation and its relation to systemic oxidant stress in premature infants <32 weeks GA.
Acknowledgments
We thank the Wildermuth Foundation, Buffalo, New York, for funding the study (VHK). We acknowledge the loan of pulse oximeters and related supplies by Masimo Corporation, Irvine, California, for use in the study. We wish to thank the respiratory therapists and nurses whose generous efforts made this study possible. We also thank Dr Chang-Xing Ma, PhD, Department of Biostatistics (University at Buffalo, Buffalo, NY), for statistical help.
Disclosure
The authors declare no conflicts of interest in this work.
References
Frank L, Sosenko IR. Prenatal development of lung antioxidant enzymes in four species. J Pediatr. 1987;110(1):106–110. | |
Ezaki S, Suzuki K, Kurishima C, et al. Resuscitation of preterm infants with reduced oxygen results in less oxidative stress than resuscitation with 100% oxygen. J Clin Biochem Nutr. 2009;44(1):111–118. | |
Saugstad OD. Oxygen toxicity in the neonatal period. Acta Paediatr Scand. 1990;79(10):881–892. | |
Kumar VH, Patel A, Swartz DD, et al. Exposure to supplemental oxygen and its effects on oxidative stress and antioxidant enzyme activity in term newborn lambs. Pediatr Res. 2010;67(1):66–71. | |
Vento M, Sastre J, Asensi MA, Vina J. Room-air resuscitation causes less damage to heart and kidney than 100% oxygen. Am J Respir Crit Care Med. 2005;172(11):1393–1398. | |
Solås AB, Kalous P, Saugstad OD. Reoxygenation with 100 or 21% oxygen after cerebral hypoxemia-ischemia-hypercapnia in newborn piglets. Biol Neonate. 2004;85(2):105–111. | |
Vento M, Moro M, Escrig R, et al. Preterm resuscitation with low oxygen causes less oxidative stress, inflammation, and chronic lung disease. Pediatrics. 2009;124(3):e439–e449. | |
Vento M, Asensi M, Sastre J, García-Sala F, Pallardó FV, Viña J. Resuscitation with room air instead of 100% oxygen prevents oxidative stress in moderately asphyxiated term neonates. Pediatrics. 2001;107(4):642–647. | |
Saugstad OD. Room air resuscitation-two decades of neonatal research. Early Hum Dev. 2005;81(1):111–116. | |
Tan A, Schulze A, O’Donnell CP, Davis PG. Air versus oxygen for resuscitation of infants at birth. Cochrane Database Syst Rev. 2005;(2):CD002273. | |
Patel A, Lakshminrusimha S, Ryan RM, et al. Exposure to supplemental oxygen downregulates antioxidant enzymes and increases pulmonary arterial contractility in premature lambs. Neonatology. 2009;96(3):182–192. | |
Saugstad OD. Bronchopulmonary dysplasia-oxidative stress and antioxidants. Semin Neonatol. 2003;8(1):39–49. | |
Ogihara T, Okamoto R, Kim HS, et al. New evidence for the involvement of oxygen radicals in triggering neonatal chronic lung disease. Pediatr Res. 1996;39(1):117–119. | |
Schock BC, Sweet DG, Halliday HL, Young IS, Ennis M. Oxidative stress in lavage fluid of preterm infants at risk of chronic lung disease. Am J Physiol Lung Cell Mol Physiol. 2001;281(6):L1386–L1391. | |
Banks BA, Ischiropoulos H, McClelland M, Ballard PL, Ballard RA. Plasma 3-nitrotyrosine is elevated in premature infants who develop bronchopulmonary dysplasia. Pediatrics. 1998;101(5):870–874. | |
Escrig R, Arruza L, Izquierdo I, et al. Achievement of targeted saturation values in extremely low gestational age neonates resuscitated with low or high oxygen concentrations: a prospective, randomized trial. Pediatrics. 2008;121(5):875–881. | |
Rabi Y, Singhal N, Nettel-Aguirre A. Room-air versus oxygen administration for resuscitation of preterm infants: the ROAR study. Pediatrics. 2011;128(2):e374–e381. | |
Wang CL, Anderson C, Leone TA, Rich W, Govindaswami B, Finer NN. Resuscitation of preterm neonates by using room air or 100% oxygen. Pediatrics. 2008;121(6):1083–1089. | |
American Heart Association, American Academy of Pediatrics. 2005 American Heart Association (AHA) guidelines for cardiopulmonary resuscitation (CPR) and emergency cardiovascular care (ECC) of pediatric and neonatal patients: neonatal resuscitation guidelines. Pediatrics. 2006;117(5):e1029–e1038. | |
Kattwinkel J, Perlman JM, Aziz K, et al. Part 15: neonatal resuscitation: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010;122(18 Suppl 3):S909–S919. | |
Ischiropoulos H. Biological tyrosine nitration: a pathophysiological function of nitric oxide and reactive oxygen species. Arch Biochem Biophys. 1998;356(1):1–11. | |
Negi R, Pande D, Kumar A, Khanna RS, Khanna HD. In vivo oxidative DNA damage and lipid peroxidation as a biomarker of oxidative stress in preterm low-birthweight infants. J Trop Pediatr. 2012;58(4):326–328. | |
Escobar J, Teramo K, Stefanovic V, et al. Amniotic fluid oxidative and nitrosative stress biomarkers correlate with fetal chronic hypoxia in diabetic pregnancies. Neonatology. 2013;103(3):193–198. | |
Vento M, Aguar M, Escobar J, et al. Antenatal steroids and antioxidant enzyme activity in preterm infants: influence of gender and timing. Antioxid Redox Signal. 2009;11(12):2945–2955. |
 © 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


 ), 40% O2 (-○-), or 100% O2 (-◊-) in each of the three groups. Each time point represents mean ± standard deviation. SpO2 significantly increased over time in the first 10 minutes after birth in all infants (P<0.0001 mixed-model analysis of variance). Upper (
), 40% O2 (-○-), or 100% O2 (-◊-) in each of the three groups. Each time point represents mean ± standard deviation. SpO2 significantly increased over time in the first 10 minutes after birth in all infants (P<0.0001 mixed-model analysis of variance). Upper ( ) and lower (
) and lower ( ) SpO2 limits (2010 AHA guidelines on neonatal resuscitation)
) SpO2 limits (2010 AHA guidelines on neonatal resuscitation)