Back to Journals » Research and Reports in Neonatology » Volume 5
Newborn care practices in rural Bangladesh
Authors Islam MT, Islam N, Yoshimura Y, Nisha MK, Yasmin N
Received 22 April 2015
Accepted for publication 13 May 2015
Published 2 July 2015 Volume 2015:5 Pages 65—72
DOI https://doi.org/10.2147/RRN.S87122
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Robert Schelonka
Mohammad Tajul Islam,1 Nazrul Islam,2 Yukie Yoshimura,1 Monjura Khatun Nisha,3 Nawzia Yasmin4
1Safe Motherhood Promotion Project, Japan International Cooperation Agency (JICA), Dhaka, Bangladesh; 2School of Population and Public Health, Faculty of Medicine, University of British Columbia, Vancouver, BC, Canada; 3International Centre for Diarrhoeal Disease Research, Bangladesh (icddr,b); 4Department of Public Health, State University of Bangladesh, Dhaka, Bangladesh
Background: Neonatal mortality is high in Bangladesh. Most of the neonatal deaths are preventable through simple and cost-effective essential newborn care interventions. Studies to document the determinants of unhealthy newborn care practices are scarce.
Objective: The objective of this study is to describe the pattern of neonatal care practices and their determinants in rural Bangladesh.
Methodology: This study is based on baseline data of a community-based intervention to assess impact of limited postnatal care services on maternal and neonatal health-seeking behavior. Data from 510 women, who had a live birth at home 1 year prior to survey, of six randomly selected unions of an Upazila (subdistrict) were analyzed.
Results: Majority of the respondents were at an age group of 20–34 years. Only 6% had delivery by skilled providers. Immediate drying and wrapping, and giving colostrums to newborns were almost universal. Unhealthy practices, like unclean cord care (42%), delayed initiation of breastfeeding (60%), use of prelacteals (36%), and early bathing (71%) were very common. Muslims were more likely to give early bath (adjusted odds ratio [OR]: 2.01; 95% confidence interval [CI]: 1.13–3.59; P=0.018) and delay in initiating breastfeeding (adjusted OR: 1.45; 95% CI: 1.18–1.78; P<0.001) to newborns. Practice of giving prelacteals was associated with teenage mothers (adjusted OR: 2.26; 95% CI: 1.19–4.28; P=0.013) and women’s lack of education (adjusted OR: 2.64; 95% CI: 1.46–4.77; P=0.001).
Conclusion: Unhealthy neonatal care practices are widespread in rural Bangladesh. Continued education to the community and home delivery attendants on essential newborn care could benefit newborn survival in Bangladesh.
Keywords: newborn care, cord care, bathing, breastfeeding, prelacteals, determinants, Bangladesh
Background
The number of newborns dying every year within the first 28 days following birth worldwide is as high as 3.6 million.1 The main causes of neonatal deaths include birth asphyxia, conditions related to prematurity and low birth weight, and severe infections.2,3 Three quarters of neonatal deaths take place in the first 7 days, and a child born in a developing country is almost 14 times more likely to die during the first 28 days of life compared to one born in developed countries.3,4
Far too little attention has been observed toward the deaths of newborns in developing countries. The death toll of neonatal mortality constitutes almost 40% of all under-five deaths.4 A staggering 98% of all neonatal deaths occur in the developing countries.5
Unhealthy newborn care practices are common in developing countries. Cord infections and neonatal tetanus, due to unhygienic cord care, continue to be the important causes of neonatal morbidity and mortality.6 A substantial proportion (37%) of neonatal deaths related to infections is due to cord infection.7 While rare in developed countries, incidence of cord infections in developing countries varies from 3% to 15%.8–10 Factors associated with cord infections include application of unhygienic materials, and lack of hand washing of caregivers and birth attendants.11
Recently conducted community-based randomized trials in Bangladesh, Nepal, and Pakistan found that application of 4% chlorhexidine on umbilical cord stump soon after birth significantly reduced severe cord infections, and neonatal mortality by 20%–38% compared to dry cord care.10,12,13 A systematic review and meta-analysis by Imdad et al on use of 4% chlorhexidine showed a 23% reduction in all-cause neonatal mortality among the home deliveries in the community.14 Based on the recent findings, the World Health Organization (WHO) recommends “Daily chlorhexidine (7.1% chlorhexidine digluconate aqueous solution or gel, delivering 4% chlorhexidine) application to the umbilical cord stump during the first week of life is recommended for newborns who are born at home in settings with high neonatal mortality (30 or more neonatal deaths per 1,000 live births).”15
Neonatal hypothermia is another important contributing factor for neonatal death, especially in low- and middle-income countries.16–18 Factors associated with neonatal hypothermia include low birth weight and prematurity, lack of skin-to-skin contact with mother, and early breastfeeding.19,20 Though there is no evidence to indicate that early bathing is associated with hypothermia, especially when the babies are of normal weight and full term,19 early bathing removes the vernix from the skin, which is a potent inhibitor of Escherichia coli, a common pathogen for neonatal infection.21 Regarding baby’s first bath, WHO recommends that if cultural tradition demands bathing, this should not be done before 6 hours and preferably be given on the second or third day of life, so long as the baby is healthy and his/her temperature is normal.18
In Bangladesh, the risk of dying in the first 28 days of life (neonatal mortality rate: 32 per 1,000 live births) is nearly threefold greater than that in the subsequent 11 months (11 per 1,000). Deaths in the neonatal period account for more than 60% of under-five mortality. Data also indicate that the decline in neonatal morality is the slowest compared to the decline in under-five and infant deaths.22 Further decrease in neonatal deaths needs efforts for reducing the infant mortality rate in the country to look beyond the achievement of the Millennium Development Goal 4.
Majority of the neonatal deaths could be prevented through simple and cost-effective essential newborn care interventions both in the community and health facilities.23 The essential newborn care is focused on prevention of infection, thermal protection, resuscitation of newborn with asphyxia, early and exclusive breastfeeding, care for the low-birth weight babies, and identification and appropriate referral of sick neonates.23,24
Among the developing countries, Bangladesh reports high home delivery (71%), mostly (73%) by medically unskilled persons.22 Community-based interventions have been found to reduce neonatal or perinatal mortality in several studies.25–27 Although some information is available on newborn care practices by the rural women in Bangladesh, studies are scarce to look at the factors for unhealthy practices related to newborn care, especially for home deliveries. It is important to monitor the progress and identify the factors associated with and challenges related to unhealthy newborn care practices for programmatic interventions. The objective of this study is to describe the pattern of and factors associated with newborn care practices by the rural women who had delivery at home.
Methodology
The methodology has been described in detail elsewhere.28 In short, the Safe Motherhood Promotion Project was implemented by the Directorate General of Health Services (DGHS), Ministry of Health and Family Welfare, Bangladesh, supported by Japan International Cooperation Agency. Under the project, a community-based intervention was designed to study the impact of limited postnatal care (PNC) services on recently delivered women in a rural community. In order to evaluate the intervention, a baseline survey was conducted in June 2010 in six out of eleven randomly selected unions (sub-subdistrict) of Monohardi Upazila (subdistrict) of Narsingdi district, situated about 75 km northeast of the capital, Dhaka. All the households of the selected unions were surveyed to identify women who had a live birth within 1 year prior to data collection. The household survey yielded 675 eligible women, of whom 510 (75.6%) had home delivery. This study analyzed the data collected from women who had a live birth at home (n=510).
Data were collected from the women through interview by a group of trained female interviewers using a pretested questionnaire after taking informed verbal consent. The questions for newborn care practices were tested and validated in other studies.23,29 This paper describes the essential newborn care practices, such as drying and wrapping, cord care, early breastfeeding including colostrums, and delayed bathing.
Data were analyzed using SAS Software (version 9.2) and SPSS (version 16.0). First, bivariate analysis was done. To find association in bivariate analysis, crude odds ratio (OR) with 95% confidence interval (CI) was calculated, while chi-square test was used to find the significance of association. Finally, unconditional logistic regression was done for each of the dichotomized dependent variables (bathed within 3 days [1= yes, 0= no], breastfed after 30 minutes [1= yes, 0= no], and gave prelacteals [1= yes, 0= no]) to identify the determinants of unhealthy practices. Factors which may influence the newborn care practices, and those found to be significant at a P-value of ≤0.10 in bivariate analysis were selected for the multivariable logistic regression models after checking for multi-collinearity. All the tests were two-sided, and a P-value of <0.05 was considered as significant.
Ethical consideration
This study is based on secondary data (baseline survey) of a community-based intervention aimed at behavior change of women for seeking PNC services from skilled providers. The intervention was provided under the ongoing Safe Motherhood Promotion Project, approved by the DGHS. Data were collected from the women after taking informed verbal consent. Ethical permission was obtained from the ethics committee of the State University of Bangladesh for analyzing the data.
Results
Out of the 510 women interviewed, only 32 (6.3%) had delivery by skilled persons. The sociodemographic characteristics of the respondents are summarized in Table 1. Majority of the respondents were Muslims (89.2%) and at the age group of 20–34 years (83.3%). A small proportion (11.4%) was at the teenage group. Only 13.7% women did not attend any school. Almost all the respondents (95.7%) were housewives. The median family income was Tk 6,000 (USD 75) per month.
  | Table 1 Sociodemographic characteristics of the respondents |
Majority of the newborns were dried (90%) and wrapped (92.7%) immediately after birth, and were provided colostrums (95.1%) (Table 2). However, more than two-thirds (71.2%) of the newborns were given bath within 3 days following delivery. More than half of the newborns were applied “something” on the umbilical cord stump. The substances commonly used to the umbilical cord (among those who provided something; n=286) were mustard oil (39.6%), antibiotic powder/antiseptics (25.4%), ash (17.7%), and boric acid powder (11.7%) (Figure 1). Only 40% of the newborns were put to the breast within half an hour of delivery, and a notable proportion (36.1%) were given prelacteals. Common prelacteals provided to the newborns (among those who provided prelacteals; n=184) included sugar water (46.2%), plain water (21.3%), and honey (18.6%) (Figure 2).
  | Table 2 Essential newborn care practices in rural Bangladesh |
  | Figure 1 Materials used on umbilical cord stump in newborn in rural Bangladesh. |
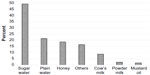  | Figure 2 Substances used as prelacteals for the newborn in rural Bangladesh. |
Table 3 shows the results of bivariate analysis of selected neonatal care practices. There was significant association between religion and early bathing of the newborns. Compared to Hindus, Muslim families were two times more likely to give bath within 3 days of delivery (OR: 2.09; 95% CI: 1.14–3.84; P=0.01). Association was found between women’s education and number of living children with practices of giving prelacteals. Uneducated mothers were 2.4 times more likely to provide prelacteals to the newborns compared to the mothers who had six or more years of education (95% CI: 1.36–4.21; P=0.001). Similarly, compared to having three or more children in the family, women who had two children were less likely (OR: 0.57; 95% CI: 0.35–0.93; P=0.014) to provide prelacteals to the newborns. Significant association was also found between complications during delivery and giving prelacteals (OR: 1.58; 95% CI: 1.01–2.47; P=0.04). No significant association of sociodemographic and other factors was found with unhygienic cord care and delayed initiation of breastfeeding (after 30 minutes of delivery).
The results of the multivariable logistic regression are presented in Table 4. After adjustment, religion was found to be significantly associated with early bathing (adjusted OR for being Muslim: 2.01; 95% CI: 1.13–3.59; P=0.018) and delayed initiation of breastfeeding (adjusted OR for being Muslim: 1.45; 95% CI: 1.18–1.78; P<0.001). Similarly, women’s age (adjusted OR for teenage mothers: 2.26; 95% CI: 1.19–4.28; P=0.013) and women’s education (adjusted OR for no education: 2.64; 95% CI: 1.46–4.77; P=0.001) were found to be significantly associated with giving prelacteals.
  | Table 4 Determinants of neonatal care practices: multivariable logistic regression analysis |
Discussion
Our study demonstrated that immediate drying (90.0%) and wrapping (92.7%), and giving colostrums (95.1%) to the newborns were almost universal. However, practices related to unhygienic cord care (41.8%), early bathing (71.2%), lack of early breastfeeding (60.0%), and use of prelacteals (36.1%) were highly prevalent and need programmatic actions for improvement.
Unhygienic practices of cord care are very common in developing countries.30–32 This study shows that “something was applied to the cord stump” in more than half of the newborns. The commonly used materials on to the cord stump, found in this study, were mustard oil (39.6%) and ash (17.7%), while a substantial proportion (25.4%) used antibiotics/antiseptics (tetracycline or gentamicin ointment/powder). WHO recommends use of 4% chlorhexidine (which was not commercially available in Bangladesh at the time of this study) on cord stump to reduce severe infection and neonatal mortality.15 The materials used on cord stump depend on traditional practices and belief that they would cause early separation and prevent bleeding.33 Ash, oil, vermillion, colostrums, butter, spices, herbs, and mud are some of the commonly used substances found in other studies.30–32 These substances, often contaminated with bacteria and spores, may greatly increase the risk of cord infection. The findings of this study indicate that the community and home delivery providers need to be educated on harmful effects of using traditional materials on the cord stump with emphasis on hand washing and breastfeeding to prevent cord infections.6,11
In some countries, immediately after birth, the newborn is placed on the floor without drying and wrapping and given a bath immediately considering vernix and blood on skin to be dirty.34,35 Such an activity may lead to hypothermia and delay in putting the baby on to the mother’s breast. To prevent hypothermia, it is necessary to keep the baby pleasantly warm. Recommendations to prevent hypothermia in newborn infants include delivery in a warm room, immediate drying and wrapping with dry warm cloths, skin-to-skin contact with mother for the first few hours after birth, and early breastfeeding.23 Though WHO recommends delaying the first bath until after 24 hours, Bangladesh newborn care policy and guideline suggests delaying the first bath for 3 days.36 We have, therefore, analyzed data in line with the Bangladesh newborn care policy. Our study showed that >70.0% babies were bathed before 3 days of birth (49.6% bathed within 24 hours). This finding is similar to other studies conducted in Asia and Africa.32,34,35,37 Our study found that Muslims were two times more likely to give early bath (before 3 days), which may be because of their belief that the newborns are “napak” (unholy) till they are bathed.35
There is no controversy about the innumerable benefits of breastfeeding both for the baby and mother.38–41 It is ideal to initiate breastfeeding within half an hour of birth for production of breast milk and prevention of postpartum hemorrhage.42,43 Our study showed that though all the babies were breastfed, only 40.0% were put to the breast within 30 minutes. Moreover, contrary to the recommendations, about a third of the newborns were offered some kind of prelacteals before initiation of breastfeeding. Prelacteal feedings are usually given due to perceived delay in the flow of breast milk, and stop the baby from crying.44 The findings of this study are comparable with other studies conducted in Asia34,35,37 and Africa.31,32 Our study found that Muslims were 1.5 times more likely to delay breastfeeding to the newborn compared to the Hindus. Moreover, teenage mothers and women with no education were more likely (more than two times) to give prelacteals. All these findings suggest that pregnant women, their family members, and home delivery attendants in rural areas need information and education on benefits of early breastfeeding and harmful effects of prelacteals. Opportunities should be taken at all routine contacts to educate them on all the neonatal health issues.
This study was conducted in a rural subdistrict of Bangladesh. Naturally, the study findings may not be generalizable. However, all the study findings are consistent with the Bangladesh Demographic and Health Survey conducted in 2010 taking a nationally representative sample of women who had a live birth 3 years preceding the survey.22
In our study, questions about newborn care practices were restricted to women who had a live birth within a year preceding the interview to minimize recall bias. However, some information biases may still exist. For example, the newborns are usually managed either by the birth attendant or relatives present during home delivery, and the mother may not be informed about the cord care and use of prelacteals. Moreover, this study does not explain why such unhealthy behaviors are carried out and who are the people actually influencing the unhealthy practices. In order to develop effective interventions to change newborn care practices, such information is important but missing in this study.
Conclusion
The findings of this study suggest that unhealthy practices related to newborn care, such as unhygienic cord care, delayed initiation of breastfeeding, use of prelacteals, and early bathing are prevalent in rural areas of Bangladesh. Religion and women’s education were the important determinants of such behaviors. Effective implementation of widespread education program for the community and home delivery attendants on early and exclusive breastfeeding, delayed bathing, and WHO-recommended cord care could benefit newborn survival in Bangladesh.
Acknowledgments
The authors are thankful to the Ministry of Health and Family Welfare of Bangladesh, Japan International Cooperation Agency (JICA), and CARE-Bangladesh for implementing the limited PNC operations research project from where data were extracted. We also thank the district project and CARE-Bangladesh staff involved in supervision of field data collection as well as the data collectors for their hard work. This study was financially and technically supported by JICA, Bangladesh, under Technical Cooperation Project category. JICA did not have any influence in any stage of this publication including data analysis, interpretation of the findings, or the decision/choice of publication.
Author contributions
MTI and YY conceptualized and designed the study and data collection methods. MTI, NI, YY, and MKN analyzed the data. All authors contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
Lawn JE, Kerber K, Enweronu-Laryea C, Cousens S. 3.6 million neonatal deaths – what is progressing and what is not? Semin Perinatol. 2010;34(6):371–386. | |
Investigators of the National Neonatal Perinatal Database (NNPD) – National Neonatology Forum of India. Morbidity and mortality among outborn neonates at 10 tertiary care institutions in India during the year 2000. J Trop Pediatr. 2004;50(3):170–174. | |
Lawn JE, Cousens S, Zupan J. 4 million neonatal deaths: when? where? why? Lancet. 2005;365(9462):891–890. | |
UNICEF. Maternal and Newborn Health, The State of the World’s Children 2009. New York, USA: UNICEF; 2009. | |
Carlo WA, Goudar SS, Jehan I, et al; First Breath Study Group. Newborn-care training and perinatal mortality in developing countries. N Engl J Med. 2010;362(7):614–623. | |
World Health Organization. Care of the Umbilical Cord: A Review of the Evidence. Reproductive Health (Technical Support) Maternal and Newborn Health: Safe Motherhood. Geneva, Switzerland: World Health Organization; 1998. | |
Antia-Obong O, Ekanem E, Udo J, Utsalo S. Septicaemia among neonates with tetanus. J Trop Pediatr. 1992;38(4):173–175. | |
Faridi M, Rattan A, Ahmad S. Omphalitis neonatorum. J Indian Med Assoc. 1993;91(11):283–285. | |
McKenna H, Johnson D. Bacteria in neonatal omphalitis. Pathology. 1977;9(2):111–113. | |
Mullany LC, Darmstadt GL, Khatry SK, et al. Topical applications of chlorhexidine to the umbilical cord for prevention of omphalitis and neonatal mortality in southern Nepal: a community-based, cluster-randomised trial. Lancet. 2006;367(9514):910–918. | |
Mullany LC, Darmstadt GL, Katz J, et al. Risk factors for umbilical cord infection among newborns of southern Nepal. Am J Epidemiol. 2007;165(2):203–211. | |
Arifeen SE, Mullany LC, Shah R, et al. The effect of cord cleansing with chlorhexidine on neonatal mortality in rural Bangladesh: a community-based, cluster-randomised trial. Lancet. 2012;379(9820):1022–1028. | |
Soofi S, Cousens S, Imdad A, Bhutto N, Ali N, Bhutta ZA. Topical application of chlorhexidine to neonatal umbilical cords for prevention of omphalitis and neonatal mortality in a rural district of Pakistan: a community-based, cluster-randomised trial. Lancet. 2012;379(9820):1029–1036. | |
Imdad A, Mullany LC, Baqui AH, et al. The effect of umbilical cord cleansing with chlorhexidine on omphalitis and neonatal mortality in community settings in developing countries: a meta-analysis. BMC Public Health. 2013;13(Suppl 3):S15. | |
World Health Organization. WHO Recommendations on Postnatal Care of the Mother and Newborn. Geneva, Switzerland: World Health Organization; 2013. | |
Kumar V, Shearer J, Kumar A, Darmstadt G. Neonatal hypothermia in low resource settings: a review. J Perinatol. 2009;29(6):401–412. | |
Mullany LC, Katz J, Khatry SK, LeClerq SC, Darmstadt GL, Tielsch JM. Risk of mortality associated with neonatal hypothermia in southern Nepal. Arch Pediatr Adolesc Med. 2010;164(7):650–656. | |
World Health Organization. Thermal Protection of the Newborn: a Practical Guide. Division of Reproductive Health (Technical Support). Geneva, Switzerland: World Health Organization; 1997. | |
Mullany LC, Katz J, Khatry SK, LeClerq SC, Darmstadt GL, Tielsch JM. Neonatal hypothermia and associated risk factors among newborns of southern Nepal. BMC Med. 2010;8(1):43. | |
Ogunlesi TA, Ogunfowora OB, Ogundeyi MM. Prevalence and risk factors for hypothermia on admission in Nigerian babies <72 h of age. J Perinat Med. 2009;37(2):180–184. | |
Tollin M, Bergsson G, Kai-Larsen Y, et al. Vernix caseosa as a multi- component defence system based on polypeptides, lipids and their interactions. Cell Mol Life Sci. 2005;62(19–20):2390–2399. | |
National Institute of Population Research and Training. Bangladesh Demographic and Health Survey 2011. Dhaka, Bangladesh: National Institute of Population Research and Training, Mitra and Associates. Calverton, Maryland, USA: MEASURE DHS, ICF International; 2013. | |
World Health Organization. Essential Newborn Care: Report of a Technical Working Group (Trieste, 25–29 April 1994). Geneva, Switzerland: World Health Organization; 1996. | |
Costello A, Manandhar D. Improving Newborn Infant Health in Developing Countries. London: Imperial College Press; 2000. | |
Bang AT, Bang RA, Baitule SB, Reddy MH, Deshmukh MD. Effect of home-based neonatal care and management of sepsis on neonatal mortality: field trial in rural India. Lancet. 1999;354(9194):1955–1961. | |
Baqui AH, El-Arifeen S, Darmstadt GL, et al; Projahnmo Study Group. Effect of community-based newborn-care intervention package implemented through two service-delivery strategies in Sylhet district, Bangladesh: a cluster-randomised controlled trial. Lancet. 2008;371(9628):1936–1944. | |
Manandhar DS, Osrin D, Shrestha BP, et al; Members of the MIRA Makwanpur trial team. Effect of a participatory intervention with women’s groups on birth outcomes in Nepal: cluster-randomised controlled trial. Lancet. 2004;364(9438):970–979. | |
Islam N, Islam MT, Yoshimura Y. Practices and determinants of delivery by skilled birth attendants in Bangladesh. Reprod Health. 2014;11(1):86. | |
Yoder P, Rosato M, Mahmud R, Fort A, Rahman F. Womens Recall of Delivery and Neonatal Care in Bangladesh and in Malawi. A Study of Terms Concepts and Survey Questions. Calverton, MD: ICF Macro; 2010. | |
Andrews JY, Dalal K. Umbilical cord-cutting practices and place of delivery in Bangladesh. Int J Gynecol Obstet. 2011;114(1):43–46. | |
Penfold S, Hill Z, Mrisho M, et al. A large cross-sectional community- based study of newborn care practices in southern Tanzania. PLoS One. 2010;5(12):e15593. | |
Waiswa P, Peterson S, Tomson G, Pariyo GW. Poor newborn care practices-a population based survey in eastern Uganda. BMC Pregnancy Childbirth. 2010;10(1):9. | |
Obuekwe IF, Obuekwe IC. Identifying Indigenous Health Technologies used by women in a rural community in Nigeria on the cord stumps of newborns: a decrease in cord infections and neonatal tetanus? J Int Womens Stud. 2003;4(3):148–153. | |
Fikree FF, Ali TS, Durocher JM, Rahbar MH. Newborn care practices in low socioeconomic settlements of Karachi, Pakistan. Soc Sci Med. 2005;60(5):911–921. | |
Moran AC, Choudhury N, Uz Zaman Khan N, et al. Newborn care practices among slum dwellers in Dhaka, Bangladesh: a quantitative and qualitative exploratory study. BMC Pregnancy Childbirth. 2009;9(1):54. | |
Ministry of Health and Family Welfare. National Neonatal Health Strategy and Guidelines for Bangladesh. Dhaka, Bangladesh: Ministry of Health and Family Welfare; Government of the People’s Republic of Bangladesh; 2009. | |
Sreeramareddy CT, Joshi HS, Sreekumaran BV, Giri S, Chuni N. Home delivery and newborn care practices among urban women in western Nepal: a questionnaire survey. BMC Pregnancy Childbirth. 2006;6(1):27. | |
Hanson L, Söderström T. Human milk: defense against infection. Prog Clin Biol Res. 1980;61:147–159. | |
Horta BL, Bahl R, Martines JC, Victora CG. Evidence on the Long-Term Effects of Breastfeeding: Systematic Reviews and Meta-Analyses. Geneva, Switzerland: World Health Organization; 2007. | |
Ip S, Chung M, Raman G, et al. Breastfeeding and Maternal and Infant Health Outcomes in Developed Countries. Rockville, MD: Agency for Healthcare Research and Quality; 2007. | |
World Health Organization, UNICEF. Global Strategy for Infant and Young Child Feeding. Geneva, Switzerland: World Health Organization; 2003. | |
Matthiesen AS, Ransjö-Arvidson AB, Nissen E, Uvnäs-Moberg K. Postpartum maternal oxytocin release by newborns: effects of infant hand massage and sucking. Birth. 2001;28(1):13–19. | |
Widström A, Winberg J, Werner S, Hamberger B, Eneroth P, Uvnäs- Moberg K. Suckling in lactating women stimulates the secretion of insulin and prolactin without concomitant effects on gastrin, growth hormone, calcitonin, vasopressin or catecholamines. Early Hum Dev. 1984;10(1):115–122. | |
Darmstadt GL, Syed U, Patel Z, Kabir N. Review of domiciliary newborn- care practices in Bangladesh. J Health Popul Nutr. 2006;24(4):380. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

