Back to Journals » Drug Design, Development and Therapy » Volume 9
Management of severe sepsis: advances, challenges, and current status
Authors Martin-loeches I, Levy M, Artigas A
Received 5 December 2014
Accepted for publication 9 January 2015
Published 9 April 2015 Volume 2015:9 Pages 2079—2088
DOI https://doi.org/10.2147/DDDT.S78757
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Shu-Feng Zhou
Ignacio Martin-Loeches,1 Mitchell M Levy,2 Antonio Artigas3
1Multidisciplinary Intensive Care Research Organization (MICRO), St James’s University Hospital, Trinity Centre for Health Sciences, Dublin, Ireland; 2Brown University, Providence, RI, USA; 3Critical Care Center, CIBER Enfermedades Respiratorias, Sabadell Hospital, Corporació Sanitaria Universitaria Parc Tauli, Autonomous University of Barcelona, Barcelona, Spain
Abstract: The complexity of treating severe sepsis and septic shock has been elucidated in myriad studies, particularly in the past 10 years. The development of clinical guidelines, insight into the effect of bundle elements, and results of clinical trials have brought to light further opportunities and questions in the approach to pharmaceutical interventions for the global challenge to save lives and reduce healthcare costs. Therapeutic interventions including fluid resuscitation, hemodynamic monitoring, glycemic control, corticosteroids, and antimicrobial therapy and stewardship inform outcomes. Research on biomarkers, use of mesenchymal stem cells, blood purification, immunoglobulins, and antioxidative treatments apropos the immune response may soon yield viable therapies.
Keywords: sepsis, septic shock, guidelines, critical care, biomarkers, surviving sepsis campaign
Introduction
Severe sepsis is a complex syndrome that has been estimated to affect more than 750,000 people annually in the US alone. Epidemiology studies indicate that the number of people diagnosed with severe sepsis and septic shock is increasing year by year, eclipsing the incidence of stroke, cancer, and myocardial infarction as well as contributing enormously to health care costs.1 An aging population admitted to the hospitals with many comorbid conditions contributes to these increases. Simultaneously, outcomes have been improving. A retrospective, observational study including more than 100,000 patients with severe sepsis in Australia and New Zealand found that hospital mortality decreased steadily throughout the last decade.2 Interestingly, the authors found the same improvement occurred in nonseptic patients, but such patients had lower rates of discharge to home and higher rates of discharge to rehabilitation. In a similar time frame, Levy et al3 analyzed the association between compliance with the Surviving Sepsis Campaign (SSC) performance bundles and mortality measured in 29,470 subjects over 7.5 years and found that increased compliance with sepsis performance bundles was associated with a 25% relative risk reduction in mortality rate. Moreover, every 10% increase in compliance was associated with a significant decrease in the odds ratio (OR) for hospital mortality. The dissemination of awareness has contributed to increased successful initiatives of early recognition and implementation of protocols for better patient care. In addition, the hospital community is increasing the development of multidisciplinary approaches and shared protocols with simple interventions that might dramatically change the management of the patients.4 Unfortunately, over the last few years, many studies have been conducted in order to decrease the mortality rate associated with sepsis, but the pharmaceutical research community is not getting any substantial new messages regarding drug design, development, and therapy with a unanimous rate of failure.5,6 The improved communication among intensive care practitioners, emergency department personnel, and wards staff regarding best practices for early recognition and management of patients with severe sepsis has no doubt contributed to better patient care.
Epidemiology
The global epidemiologic data regarding outcomes for patients in intensive care units (ICUs) are scarce, but are important in understanding the worldwide burden of critical illness. The Intensive Care Over Nations (ICON) audit had a total of 730 participating centers in 84 countries comprising more than 10,000 patients.7 One-third of the patients had severe sepsis on admission or during the ICU stay; and while the general ICU mortality rate was 16.2%, the number almost doubled (25.8%) in patients with sepsis. The same trend was also seen when hospital mortality was analyzed. Hospitals have recognized the burden of sepsis and are currently at a landmark point for implementing strategic policies that address this within their facilities. The acknowledgment of the increasing sepsis rate has helped health authorities facilitate the acquisition of resources that foster needed policy and management pathways in designated areas.
It is important to note that despite the increasing number of severe sepsis patients, inconsistent coding obscures exact numbers. As Rhee et al8 have described, the “suspected infection” code is problematic. They report a dichotomous sustained decrease in hospitalizations for the infections that most commonly cause sepsis (pneumonia, urinary tract infections, intra-abdominal infections, and bacteremia). The implementation of policy mandates and surveillance methods might help clinicians and authorities better determine the “true” incidence of sepsis in the health care system. Doing so might balance the overuse of advanced diagnostic tools with judicious management processes and contain the use of broad-spectrum antibiotics. While antibiotic stewardship programs should be implemented, the burden of sepsis and the high associated mortality should determine a successful balance in the near future. Similar to other well-known diseases, prompt recognition has resulted in improved patient outcomes. Acute myocardial infarction (“door to balloon”), stroke (“time lost is brain lost”), and trauma (“golden hour”) are good examples of key messages about early recognition that can have a huge impact.
Implementation of guidelines and bundles
Following the publication of the Surviving Sepsis Campaign Guidelines in 2004,9 individual elements of care that were shown to produce better outcomes when applied together were grouped into “bundles of care”. Similarly, in patients with acute myocardial infarction, the successful event of opening an occluded coronary artery is the key intervention in the treatment process. In severe sepsis and septic shock, many interventions need to be completed at the same time using a multidisciplinary approach. The SSC grouped interventions into two bundles of care: the resuscitation bundle and the management bundle, which were to be achieved over the first 6 and 24 hours from recognition of severe sepsis, respectively. Application of this multidisciplinary, global approach resulted in a reduction of hospital mortality directly related to the implementation of the care bundles.10 In a multicenter, prospective study with a large cohort of severely septic patients in which an educational program based on SSC guidelines and bundles was implemented, Ferrer et al11 demonstrated improvement in the application of individual process-of-care bundle elements and reduced mortality in patients with severe sepsis and septic shock. Interestingly, a further study that aimed to evaluate the cost-effectiveness of the SSC protocol after the implementation of an educational program found that mean costs per patient were higher in the SSC protocol care cohort, largely as a result of increased length of stay; however, mean life years gained were higher in the SSC protocol care cohort, 0.54 years (95% CI 0.02–1.05 years), demonstrating that the SSC protocol seems to be a cost-effective option.12
More recently, Castellanos-Ortega et al13 performed a quasi-experimental study with a historical comparison group to determine the contribution of the various elements of the bundles to the outcome and found that the benefits depended on the number of interventions accomplished within the time limits. The 6-hour resuscitation bundle showed greater compliance and effectiveness than the 24-hour management bundle. This also supports the theory that the most important parts of the process of care are related to early intervention.
Guidelines and bundles updates
In 2012, SSC updated the guidelines based on new evidence since the first revision of 2008.14,15 Several recommendations were updated (Table 1). However, several elements remain controversial.
  | Table 1 SSC 2013 updates |
The ProCESS trial randomized and included 1,341 patients with early septic shock and compared three management strategies: Protocolized Early Goal-Directed Therapy (EGDT), protocolized standard care, and usual care.16 The main conclusion is that protocol-based EGDT using central venous catheterization and oxygen-saturation monitoring does not lead to better outcomes for septic patients when compared with management without a protocol. While this study could not show the beneficial effect of EGDT, one point was especially relevant: Early detection with timely administration of antibiotics and fluids was the single most important factor in reducing mortality and morbidity from sepsis. In addition, when comparing the different study groups, no benefit was found for titrating to SCVo2 or central venous pressure (CVP) measurements and might allow for the refinement of EGDT by defining fluid administration boundaries to avoid the complications of renal failure and pulmonary dysfunction. What the study could not say was that hemodynamic monitoring should be eliminated in relation to care of patients with severe sepsis. Importantly, the true mortality figures in this study were around 28% at 60 days and around 32% at 90 days due to the way the mortality data were censored at hospital discharge. The sample size had to be recalculated in the first interim analysis based on apparent lower mortality rates and the fact that the fluid challenge defined in the protocol as 20 mL/kg over 30 minutes was modified to 1,000 mL of fluids over 30 minutes, which may have led to the inclusion of less sick patients (Figure 1).
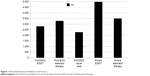  | Figure 1 Fluid administration between 0 and 6 hours. |
The results from the Australasian Resuscitation In Sepsis Evaluation (ARISE) Randomised Controlled Trial also showed that in critically ill patients presenting to the emergency department with early septic shock, EGDT did not reduce all-cause mortality at 90 days.17 In light of the evidence from the ProCESS and ARISE trials and pending the results of the Protocolized Management in Sepsis (ProMISe) Trial, the SSC guidelines committee will review the evidence and assess whether the guidelines need to be updated.18 The SSC bundles will also be reviewed and revised as needed on the basis of the recommendations.
Current antibiotic strategies for severe sepsis and septic shock
The use of early and appropriate antibiotic therapy is crucial to improved survival rates in severe sepsis and septic shock. Early antimicrobial therapy along with other supportive resuscitation goals should be achieved to avoid the further development of cellular dysfunction, tissue injury, and overwhelming inflammatory response. This theory was launched 100 years ago with Paul Ehrlich’s paradigm: “Frapper fort et frapper vite” or “Hit hard and hit fast”. Kumar et al19 analyzed a retrospective cohort of 2,731 adult patients with septic shock and found that effective antimicrobial administration within the first hour of documented hypotension was associated with increased survival to hospital discharge.20 Despite a progressive increase in mortality rate with increasing delays, only 50% of septic shock patients received effective antimicrobial therapy within 6 hours of documented hypotension. Several articles have also reported similar results, which make the common delay in the administration of antibiotics puzzling (Table 2). Ferrer et al20 conducted a retrospective analysis of 17,990 patients from 28,150 patients with severe sepsis and septic shock collected prospectively for the SSC database from 165 multinational ICUs in Europe, USA, and South America. The results demonstrate that a delay in first antibiotic administration was associated with increased in-hospital mortality, with a linear increase in the mortality for each hour’s delay in antibiotic administration. Moreover, the adjusted hospital mortality ORs steadily increased from 1.00 to 1.52 as time to antibiotic administration increased from 0 to 6 hours, where 0–1 hour is the referent group. The probability of mortality increased from 24.6% to 33.1%. It is important to determine that time of severe sepsis recognition, rather than onset, is used as “time zero”, or “when the clock starts”, for determining elapsed time to antibiotics.
  | Table 2 Common delays in antibiotic administration in landmark sepsis studies |
Antibiotic stewardship in severe sepsis and septic shock: combination vs de-escalation
Recent studies show that some antibiotic strategies can improve survival in patients with severe sepsis and septic shock. Díaz-Martín et al21 found that in patients who received antimicrobials within the first 6 hours of diagnosis, combination antimicrobial agents with different mechanisms of action – termed “different-class combination therapy” (DCCT) – may be useful in a subset of critically ill patients. Particularly in those with septic shock in more than 1,000 patients with severe sepsis, the mortality rate was significantly lower in patients administered DCCTs than in those who were administered monotherapy and any other combination therapy possibilities (non-DCCT). On the other hand, Brunkhorst et al22 could not find any benefit from treatment with combined meropenem and moxifloxacin compared with meropenem alone in mortality or organ failure. Antibiotic stewardship strategies are necessary to counterbalance the administration of appropriate antibiotic treatment in a timely manner with the threat of generating resistance.
De-escalation of antimicrobials in patients with severe sepsis is one approach. De-escalation, defined as discontinuation of an antimicrobial agent or change of antibiotic to one with a narrower spectrum once culture results were available, was analyzed by Garnacho-Montero et al.23 The authors carried out a prospective observational study of patients with severe sepsis or septic shock and found that de-escalation was applied to one-third of the patients. Not only the multivariate analysis, but also the propensity-score adjusted logistic regression models confirmed that de-escalation therapy was a protective factor not only for in-hospital but also for 90-day mortality. Interestingly, Leone et al’s24 multicenter nonblinded randomized noninferiority trial did not show a different mortality rate, but the strategy based on de-escalation of antibiotics resulted in prolonged duration of ICU stay.
General management paradigms
While different organizations agree that the topics of the individual elements in the SSC care bundles – fluid resuscitation, hemodynamic management, and antibiotic administration – should be included in general management of severe sepsis and septic shock patients, they have suggested different approaches.
Fluid resuscitation
The effects of the use of aggressive fluid resuscitation and types of fluids in severe sepsis patients continue to be debated. Several studies have been published to determine the efficacy of crystalloids compared with that of colloids. Colloids are used as they are thought to remain in the intravascular space longer, achieve faster circulatory stabilization, and require less amount of fluid for resuscitation compared with crystalloids.25 Perner et al26 elegantly demonstrated that patients with severe sepsis who received fluid resuscitation with HES 130/0.42 had increased mortality, increased risk of renal replacement therapy, a tendency toward increased bleeding, and increased blood product transfusion when compared with resuscitation with Ringers acetate. Myburgh et al27 assigned 7,000 patients who had been admitted to an ICU in a 1:1 ratio to receive either 6% HES with a molecular weight of 130 kD and a molar substitution ratio of 0.4 (130/0.4, Voluven, Fresenius Kabi Norge AS, Halden, Norway) in 0.9% sodium chloride or 0.9% sodium chloride (saline) for all fluid resuscitation and found no difference in 90-day mortality in a heterogeneous group of critically ill patients. Therefore, taking into consideration the absence of significant clinical benefit and the potential harmful effect of starches based on the above studies, the 2013 SSC28 guidelines recommended against using any HES in patients with severe sepsis. Three additional studies should be mentioned: SAFE trial,29 Therapy in the Colloids Versus Crystalloids for the Resuscitation of the Critically Ill (CRISTAL) trial,30 and albumin replacement in patients with severe sepsis or septic shock (ALBIOS).31 The SAFE trial compared the effect of fluid resuscitation with albumin or saline on mortality in a heterogeneous population of patients in the ICU in a multicenter, randomized, double-blind study and found that the use of either 4% albumin or normal saline for fluid resuscitation results in similar outcomes at 28 days. The CRISTAL trial tested whether the use of colloids compared with that of crystalloids for fluid resuscitation alters mortality in patients admitted to the ICU with hypovolemic shock and found that the use of colloids vs crystalloids did not result in a significant difference in 28-day mortality. On the other hand, in the ALBIOS trial, 1,818 patients from 100 ICUs with severe sepsis were randomly assigned to receive either 20% albumin and crystalloid solution or crystalloid solution alone. Authors found no mortality differences at 28 and 90 days. However, the post hoc univariate and multivariate analyses of data from the 1,121 patients with septic shock showed significantly lower mortality at 90 days in the albumin group than in the crystalloid group. Conversely, in the subgroup of patients with severe sepsis without shock, mortality appeared to be higher among those who were treated with albumin than among those treated with crystalloids alone.
Current hemodynamic management
Several recommendations have been made to optimize hemodynamic monitoring. Despite debate over the use of CVP levels as measures instead of dynamic parameters, the overriding goal is to achieve an optimal blood flow to the tissues. No large, randomized controlled trial exists to support a mean arterial pressure (MAP) target in sepsis. A higher MAP goal than the current 65 mmHg that was recommended by the SSC may theoretically improve end-organ perfusion, especially for those with chronic hypertension. However, whether this blood pressure target is more or less effective than a higher target is unknown. For this reason, a multicenter, open-label trial (SEPSISPAM) was conducted, and 776 patients were assigned a target MAP of either 80–85 mmHg (high-target group) or 65–70 mmHg (low-target group).32 The authors found no difference in either 28-day mortality (36.6% vs 34% [HR, 1.07; 95% CI, 0.84–1.38]) or 90-day mortality (43.8% vs 42.3% [RR, 1.04; 95% CI, 0.83–1.30]). Interestingly, the authors found less use of renal support in chronic hypertensive patients (42.2% vs 31.7% [OR 0.64; 95% CI, 0.41–0.99; P=0.046]). Some points should be mentioned regarding interpretation of the results of this study: It was not blinded; there was an incomplete recording of inclusion variables (right-heart catheterization, pulse pressure measurement, stroke volume measurement, and echocardiography); it was underpowered secondary to lower-than-expected mortality; MAPs achieved tended to be above their goal ranges (70–75 and 85–90 mmHg); there was widespread corticosteroid use; and the incidence of stroke was not measured, which is problematic given the rate of atrial fibrillation reported (2.8% vs 6.7% [P=0.02]).
Novel approaches in the pipeline
Mesenchymal stem cells
In sepsis, endothelial damage leads to further organ deterioration. Despite the use of different experimental therapies to block the immune cascade, often damage has already occurred. The use of mesenchymal stem cells (MSCs) has been a promising alternative in a variety of diseases, including cardiovascular, neurodegenerative, peripheral vascular, renal, and others. Their beneficial effects are due to the ability of MSC to repair tissue in injury and inflammation, to attenuate the inflammatory response, and to accelerate tissue healing and neoangiogenesis.33,34
The potential therapeutic value of cell-based therapy with MSC has been reported in mouse models of polymicrobial peritoneal sepsis. The potential therapeutic effect of intravenous bone marrow-derived human MSC in peritoneal sepsis induced by gram-negative bacteria has been tested.35 In this model, survival was significantly increased, and a marked reduction in the number of bacterial colony-forming units of Pseudomonas aeruginosa was shown in the blood treated with intravenous MSC compared with control mice. The effect was in part explained by a monocyte-dependent increase in bacterial phagocytosis. While this is a new area of investigation, several studies are being conducted, and the body of evidence is rising. It is important to take into account that sepsis is a complex process where several factors play key roles in the pathogenesis: direct effects of bacterial compound, cytokine storm, activation of the endothelium, and subsequently the complement and coagulation process. By affecting the overall cascade, MSC would be helpful in restoring and counteracting the deleterious effect that sepsis creates in the tissues. The encouraging trials in animal models would likely transfer to clinical settings, but a rational and careful approach with deep understanding of MSC mechanisms and actions is warranted under inflammatory conditions.
Blood purification
Therapies based on blood purification to counteract the deleterious effects of bacteria on the endothelium have recently emerged.36 The vast majority of the studies are focused on blocking endotoxin, one of the principal components on the outer membrane of gram-negative bacteria, as it is considered to be a factor in sepsis pathogenesis. High levels of endotoxin activity have been associated with worse clinical outcomes.37 A landmark study was published in 2009.38 With a limited sample size (64 patients), polymyxin B hemoperfusion added to conventional therapy significantly improved hemodynamics and organ dysfunction and reduced 28-day mortality in severe sepsis and septic shock patients affected by Gram-negative infections. In addition, a systematic review and meta-analysis of randomized trials were conducted to determine the association between various blood purification techniques and all-cause mortality in humans with sepsis.36 A total of 16 trials (n=827) were analyzed, and blood purification techniques including hemoperfusion, plasma exchange, and hemofiltration with hemoperfusion were associated with lower mortality in patients with sepsis. However, after pooling all trials of blood purification for treatment of sepsis, the therapies were not associated with lower mortality.
At this writing, three studies of blood purification treatments are being conducted. ABDO-MIX is a multicenter French Phase III study of hemoperfusion with a polymyxin column vs standard therapy in patients with peritonitis and septic shock. EUPHRATES is a multicenter US-based Phase III trial in patients with confirmed endotoxemia, incorporating sham perfusion and two treatments in 24 hours with polymyxin. SAFE-BT is a randomized, multicenter, controlled clinical study on the effect of the selective adsorption system for removal of negatively charged large biomolecules. The forthcoming results of these studies should provide a strong recommendation regarding the exact role, benefits, and cost-effectiveness of blood purification therapies.
Other therapies
Apart from the aforementioned therapies, there are some promising therapies to be considered in the future, two of which are of special relevance: innate immunity modulation with the use of infused immunoglobulin (IgM enriched immunoglobulins) and antioxidative therapies.
The efficacy of polyclonal intravenous immunoglobulin (IVIG) as adjunct therapy in sepsis has been a matter of debate over the last few years.39 Interestingly, several studies have shown a good correlation with low levels of certain immunoglobulins in blood in patients with severe sepsis. Tamayo et al40 described an inverse correlation of the levels of IgG1, IgG2, IgG3, IgM, IgA, and total IgG to the probability of death at 28 days. Recently, a meta-analysis that included 43 out of 88 potentially eligible studies found that there was a favorable outcome among adults with sepsis with the infusion of polyclonal IVIG but only with a very selected population.
During the sepsis injury and the inflammatory response, there is a marked oxidative state that may result in organ damage,41 for which the potential benefit of modulation by antioxidant therapy has been suggested. There is a molecule that seems to be promising in animal studies via antioxidant effects: melatonin. Fink et al42 recently discovered that melatonin receptors mediate improvements of survival after polymicrobial sepsis. While studies in patients are still being awaited, melatonin seems to be very promising for future RCT.
Updates on controversial topics
Tight glycemic control
Hyperglycemia is very common in patients with sepsis. At the same time, hyperglycemia has been reported to be associated with adverse events, including oxidative stress disorder, impairment of the immune system that might carry a higher susceptibility to infection due to an endothelial dysfunction.43 Several studies in the past found that the presence of hyperglycemia was independently associated with increased mortality in critically ill patients,44 especially in those with sepsis.45 Before the launch of the SSC 2013 update, the previous guidelines included a recommendation for intensive insulin therapy (IIT). However, some RCTs that have attempted to determine whether IIT targeted toward establishing normoglycemia could benefit septic patients have produced inconsistent results. A meta-analysis up to September 2013 that included randomized controlled trials of 4,100 patients comparing IIT with conventional glucose management in septic patients found that IIT did not reduce any of the outcomes: overall, 28-day, 90-day, ICU, and hospital mortality.46 As secondary outcomes, neither severity of illness nor length of ICU stay was better in patients with IIT. On the contrary, the incidence of hypoglycemia was markedly higher with the IIT. Therefore, the 2013 update of the SSC guidelines included a strong recommendation for a protocolized approach to blood glucose management in ICU patients with severe sepsis, commencing insulin dosing when two consecutive blood glucose levels are >180 mg/dL. This protocolized approach should target an upper blood glucose level ≤180 mg/dL rather than an upper target blood glucose level ≤110 mg/dL. The use of automated closed-loop control based on subcutaneous glucose measurements is currently feasible and may provide efficacious and hypoglycemia-free glucose control in critically ill adults.47
Corticosteroids: friend or foe
Endogenous glucocorticoids as end-effectors play a role in inhibiting inflammation, but are not always effective in suppressing the cytokine storm driven by a systemic inflammation, even though cortisol levels have been correlated with grades of severity of illness and mortality. With the concept of corticosteroid illness-related corticosteroid insufficiency (CIRCI) and the results of clinical trials showing immune and hemodynamic benefits, corticosteroid therapy has re-emerged as a promising adjunct for the treatment of severe sepsis. From the 1950s to the 1980s, high-dose steroids were used in the management of sepsis. Over the last 40 years, the use of steroids for treatment of infections, sepsis, and septic shock has vacillated (Figure 2).14,48–57 While the use until the late 1990s was based mainly on high doses, the use of low doses (relative adrenal insufficiency dose) has since been the focus of study. On the basis of more recent evidence and published meta-analysis, the benefit of treatment with steroids seems to be limited to patients with vasopressor-dependent septic shock with adequate fluid resuscitation. The adrenocorticotropic hormone stimulation test should not be used to identify those patients with septic shock who should receive glucocorticoids.
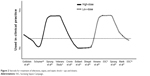  | Figure 2 Steroids for treatment of infections, sepsis, and septic shock – ups and downs. |
Diagnosis mandates: how to use biomarkers wisely
The use of biomarkers has been promising for sepsis management. Results from clinical trials of biomarker-guided therapeutic drugs that boost immunity showed promising findings in sepsis.58 Whereas the use of such markers has been focused on the diagnosis of sepsis, in order to differentiate between infectious and noninfectious processes, new developments are based on monitoring the response to the treatment in patients with sepsis. Several biomarkers have been proposed, but it is important to note the use of procalcitonin for targeting treatment duration, and resolution of sepsis. Procalcitonin has also been found useful to implement an appropriate plan of treatment, to measure and tailor the response of the treatment and a good correlation with clinical severity. In addition, biomarker guidance of antibiotic stewardship seems to be a very promising new approach. In several randomized controlled trials, including critically ill adult patients, procalcitonin guidance was repeatedly associated with a decrease in the duration of antibiotic therapy.59
Probably because the sepsis process has a very complex pathophysiology, many biomarkers have been considered. Many markers are based on inflammation monitoring, but coagulation, complement, contact system activation, and apoptosis have been proposed to play a fundamental role.60 Therefore, several markers might be used to inform about which part of the system is affected.
Final considerations
The appropriate balance between inflammation and anti-inflammation seems to be fundamental to a better understanding of the sepsis syndrome. Several mediator-selective anti-inflammatory drugs were utilized for a brief period, but were considered disappointing. While an exaggerated inflammatory response is deleterious, the timing and appropriateness of therapy may be key to patient outcomes. To date, more than 100 RCTs (Phases I–III) looking at therapies that can modulate inflammation have been conducted, with contradictory results. With more than 200 potential targets, it is worrisome that there are no definitive therapies to improve the outcome in septic patients.
Additional considerations should be taken into account. First, sepsis is a complex process with a high degree of heterogeneity. One patient will not modulate the infectious insult and the inflammatory response in the same manner as another. Second, therapeutic interventions are often not given in an appropriate dosage or duration. In addition, the timing of interventions affects therapeutic modulation, so time of diagnosis is crucial. The outcome of the patient is a matter of debate. Also, different endpoints have been considered (ie, ICU, 28-day, 90-day, hospital mortality, etc), but other less rigid surrogates such as length of stay or ventilator-free days are being included as the primary outcome of the RCT. In addition, quality of life after discharge is a cornerstone and might provide the balance in the investment for health care system sustainability.
Summary
An urgent need exists for correct patient classification that describes the degree of immune response.60 Monitoring immune status with the use of panels of biomarkers at regular intervals to assess the clinical and immune response seems to be a rational approach to better understand the value of the treatments provided. Much larger sample sizes will be needed to detect the relatively smaller effects of new therapies for sepsis. Further, revising the definition of sepsis to be sure that RCTs recruit appropriate patients remains a challenge.
Disclosure
The authors report no conflicts of interest in this work.
References
Angus DC, Linde-Zwirble WT, Lidicker J, Clermont G, Carcillo J, Pinsky MR. Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit Care Med. 2001;29(7):1303–1310. | ||
Kaukonen K-M, Bailey M, Suzuki S, Pilcher D, Bellomo R. Mortality related to severe sepsis and septic shock among critically ill patients in Australia and New Zealand, 2000–2012. JAMA. 2014;311(13):1308–1316. doi:10.1001/jama.2014.2637. | ||
Levy MM, Rhodes A, Phillips GS, et al. Surviving sepsis campaign: association between performance metrics and outcomes in a 7.5-year study. Crit Care Med. 2015;43(1):3–12. doi:10.1097/CCM.0000000000000723. | ||
Martin-Loeches I, de Haro C, Dellinger RP, et al. Effectiveness of an inspiratory pressure-limited approach to mechanical ventilation in septic patients. Eur Respir J. 2013;41(1):157–164. doi:10.1183/09031936.00221611. | ||
Lyle NH, Pena OM, Boyd JH, Hancock REW. Barriers to the effective treatment of sepsis: antimicrobial agents, sepsis definitions, and host-directed therapies. Ann N Y Acad Sci. 2014;1323:101–114. doi:10.1111/nyas.12444. | ||
Schorr CA, Zanotti S, Dellinger RP. Severe sepsis and septic shock: management and performance improvement. Virulence. 2014;5(1):190–199. doi:10.4161/viru.27409. | ||
Vincent J-L, Marshall JC, Namendys-Silva SA, et al. Assessment of the worldwide burden of critical illness: the Intensive Care Over Nations (ICON) audit. Lancet Respir Med. 2014;2(5):380–386. doi:10.1016/S2213-2600(14)70061-X. | ||
Rhee C, Gohil S, Klompas M. Regulatory mandates for sepsis care – reasons for caution. N Engl J Med. 2014;370(18):1673–1676. doi:10.1056/NEJMp1400276. | ||
Surviving Sepsis Campaign Guidelines 2004. | ||
Levy MM, Dellinger RP, Townsend SR, et al. The Surviving Sepsis Campaign: results of an international guideline-based performance improvement program targeting severe sepsis. Intensive Care Med. 2010;36(2):222–231. doi:10.1007/s00134-009-1738-3. | ||
Ferrer R, Artigas A, Levy MM, et al. Improvement in process of care and outcome after a multicenter severe sepsis educational program in Spain. JAMA. 2008;299(19):2294–2303. doi:10.1001/jama.299.19.2294. | ||
Suarez D, Ferrer R, Artigas A, et al. Cost-effectiveness of the Surviving Sepsis Campaign protocol for severe sepsis: a prospective nation-wide study in Spain. Intensive Care Med. 2011;37(3):444–452. doi:10.1007/s00134-010-2102-3. | ||
Castellanos-Ortega A, Suberviola B, García-Astudillo LA, et al. Impact of the Surviving Sepsis Campaign protocols on hospital length of stay and mortality in septic shock patients: results of a three-year follow-up quasi-experimental study. Crit Care Med. 2010;38(4):1036–1043. doi:10.1097/CCM.0b013e3181d455b6. | ||
Dellinger RP, Levy MM, Rhodes A, et al. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock, 2012. Intensive Care Med. 2013;39(2):165–228. doi:10.1007/s00134-012-2769-8. | ||
Dellinger RP, Carlet JM, Masur H, et al. Surviving Sepsis Campaign guidelines for management of severe sepsis and septic shock. Crit Care Med. 2004;32(3):858–873. Available from: http://www.ncbi.nlm.nih.gov/pubmed/15090974. Accessed October 10, 2014. | ||
Yealy DM, Kellum JA, Huang DT, et al. A randomized trial of protocol-based care for early septic shock. N Engl J Med. 2014;370(18):1683–1693. doi:10.1056/NEJMoa1401602. | ||
ARISE Investigators; ANZICS Clinical Trials Group; Peake SL, Delaney A, Bailey M, et al. Goal-directed resuscitation for patients with early septic shock. N Engl J Med. 2014;371(16):1496–1506. doi:10.1056/NEJMoa1404380. | ||
Power GS, Harrison DA, Mouncey PR, Osborn TM, Harvey SE, Rowan KM. The Protocolised Management in Sepsis (ProMISe) trial statistical analysis plan. Crit Care Resusc. 2013;15(4):311–317. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24289513. Accessed October 9, 2014. | ||
Kumar A, Roberts D, Wood KE, et al. Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock. Crit Care Med. 2006;34(6):1589–1596. doi:10.1097/01.CCM.0000217961.75225.E9. | ||
Ferrer R, Martin-Loeches I, Phillips G, et al. Empiric antibiotic treatment reduces mortality in severe sepsis and septic shock from the first hour: results from a guideline-based performance improvement program. Crit Care Med. 2014;42(8):1749–1755. doi:10.1097/CCM.0000000000000330. | ||
Díaz-Martín A, Martínez-González ML, Ferrer R, et al. Edusepsis Study Group. Antibiotic prescription patterns in the empiric therapy of severe sepsis: combination of antimicrobials with different mechanisms of action reduces mortality. Crit Care. 2012;16(6). | ||
Brunkhorst FM, Oppert M, Marx G, et al. Effect of empirical treatment with moxifloxacin and meropenem vs meropenem on sepsis-related organ dysfunction in patients with severe sepsis: a randomized trial. JAMA. 2012;307(22):2390–2399. doi:10.1001/jama.2012.5833. | ||
Garnacho-Montero J, Gutiérrez-Pizarraya A, Escoresca-Ortega A, et al. De-escalation of empirical therapy is associated with lower mortality in patients with severe sepsis and septic shock. Intensive Care Med. 2014;40(1):32–40. doi:10.1007/s00134-013-3077-7. | ||
Leone M, Bechis C, Baumstarck K, et al. De-escalation versus continuation of empirical antimicrobial treatment in severe sepsis: a multicenter non-blinded randomized noninferiority trial. Intensive Care Med. 2014;40(10):1399–1408. Available from: http://icmjournal.esicm.org/journal/134/0/10/3411/0/. | ||
Estrada CA, Murugan R. Hydroxyethyl starch in severe sepsis: end of starch era? Crit Care. 2013;17(2):310. doi:10.1186/cc12531. | ||
Perner A, Haase N, Guttormsen AB, et al. Hydroxyethyl starch 130/0.42 versus Ringer’s acetate in severe sepsis. N Engl J Med. 2012;367(2): 124–134. doi:10.1056/NEJMoa1204242. | ||
Myburgh JA, Finfer S, Bellomo R, et al. Hydroxyethyl starch or saline for fluid resuscitation in intensive care. N Engl J Med. 2012;367(20): 1901–1911. doi:10.1056/NEJMoa1209759. | ||
Dellinger RP, Levy MM, Rhodes A, et al. Surviving Sepsis Campaign Guidelines Committee including The Pediatric Subgroup. Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock, 2012. Intensive Care Med. 2013;39(2):165–228. | ||
Finfer S, Bellomo R, Boyce N, French J, Myburgh J, Norton R. A comparison of albumin and saline for fluid resuscitation in the intensive care unit. N Engl J Med. 2004;350(22):2247–2256. doi:10.1056/NEJMoa040232. | ||
Annane D, Siami S, Jaber S, et al. Effects of fluid resuscitation with colloids vs crystalloids on mortality in critically ill patients presenting with hypovolemic shock: the CRISTAL randomized trial. JAMA. 2013;310(17):1809–1817. doi:10.1001/jama.2013.280502. | ||
Caironi P, Tognoni G, Masson S, et al. Albumin replacement in patients with severe sepsis or septic shock. N Engl J Med. 2014;370(15):1412–1421. doi:10.1056/NEJMoa1305727. | ||
Asfar P, Meziani F, Hamel J-F, et al. High versus low blood-pressure target in patients with septic shock. N Engl J Med. 2014;370(17):1583–1593. doi:10.1056/NEJMoa1312173. | ||
Mei SH, Haitsma JJ, Dos Santos CC, et al. Mesenchymal stem cells reduce inflammation while enhancing bacterial clearance and improving survival in sepsis. Am J Respir Crit Care Med. 2010;182(8):1047–1057. doi:10.1164/rccm.201001-0010OC. | ||
Weil BR, Markel TA, Herrmann JL, Abarbanell AM, Kelly ML, Meldrum DR. Stem cells in sepsis. Ann Surg. 2009;250(1):19–27. doi:10.1097/SLA.0b013e3181a77b9c. | ||
Krasnodembskaya A, Samarani G, Song Y, et al. Human mesenchymal stem cells reduce mortality and bacteremia in gram-negative sepsis in mice in part by enhancing the phagocytic activity of blood monocytes. Am J Physiol Lung Cell Mol Physiol. 2012;302(10):L1003–L1013. doi:10.1152/ajplung.00180.2011. | ||
Zhou F, Peng Z, Murugan R, Kellum JA. Blood purification and mortality in sepsis: a meta-analysis of randomized trials. Crit Care Med. 2013;41(9):2209–2220. doi:10.1097/CCM.0b013e31828 cf412. | ||
Marshall JC, Foster D, Vincent J-L, et al. Diagnostic and prognostic implications of endotoxemia in critical illness: results of the MEDIC study. J Infect Dis. 2004;190(3):527–534. doi:10.1086/422254. | ||
Cruz DN, Antonelli M, Fumagalli R, et al. Early use of polymyxin B hemoperfusion in abdominal septic shock: the EUPHAS randomized controlled trial. JAMA. 2009;301(23):2445–2452. doi:10.1001/jama.2009.856. | ||
Norrby-Teglund A, Haque KN, Hammarstrom L. Intravenous polyclonal IgM-enriched immunoglobulin therapy in sepsis: a review of clinical efficacy in relation to microbiological aetiology and severity of sepsis. J Intern Med. 2006;260(6):509–516. doi:10.1111/j.1365-2796.2006.01726.x. | ||
Tamayo E, Fernández A, Almansa R, et al. Beneficial role of endogenous immunoglobulin subclasses and isotypes in septic shock. J Crit Care. 2012;27(6):616–22. | ||
Trefler S, Rodríguez A, Martín-Loeches I, et al. Oxidative stress in immunocompetent patients with severe community-acquired pneumonia. A pilot study. Med Intensiva. 2014;38(2):73–82. | ||
Fink T, Glas M, Wolf A, et al. Melatonin receptors mediate improvements of survival in a model of polymicrobial sepsis. Crit Care Med. 2014;42(1):e22–e31. doi:10.1097/CCM.0b013e3182a63e2b. | ||
Dungan KM, Braithwaite SS, Preiser J-C. Stress hyperglycaemia. Lancet. 2009;373(9677):1798–1807. Available from: http://linkinghub.elsevier.com/retrieve/pii/S0140673609605535. | ||
Van den Berghe G, Wilmer A, Hermans G, et al. Intensive insulin therapy in the medical ICU. N Engl J Med. 2006;354(5):449–461. doi:10.1056/NEJMoa052521. | ||
Ellger B, Westphal M, Stubbe HD, Van den Heuvel I, Van Aken H, Van den Berghe G. Blutzuckerkontrolle bei Patienten mit Sepsis und septischem Schock [Glycemic control in sepsis and septic shock: friend or foe?]. Anaesthesist. 2008;57(1):43–48. doi:10.1007/s00101-007-1285-7. | ||
Song F, Zhong L-J, Han L, et al. Intensive insulin therapy for septic patients: a meta-analysis of randomized controlled trials. Biomed Res Int. 2014;2014:698265. doi:10.1155/2014/698265. | ||
Leelarathna L, English SW, Thabit H, et al. Feasibility of fully automated closed-loop glucose control using continuous subcutaneous glucose measurements in critical illness: a randomized controlled trial. Crit Care. 2013;17(4):R159. doi:10.1186/cc12838. | ||
Goldstein IM, Roos D, Weissmann G, Kaplan HB. Influence of corticosteroids on human polymorphonuclear leukocyte function in vitro: reduction of lysosomal enzyme release and superoxide production. Inflammation. 1976;1(3):305–315. doi:10.1007/BF00917870. | ||
Schumer W. Steroids in the treatment of clinical septic shock. Ann Surg. 1976;184(3):333–341. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=1344393&tool=pmcentrez&rendertype=abstract. Accessed October 10, 2014. | ||
Sprung CL, Caralis PV, Marcial EH, et al. The effects of high-dose corticosteroids in patients with septic shock. A prospective, controlled study. N Engl J Med. 1984;311(18):1137–1143. doi:10.1056/NEJM198411013111801. | ||
The Veterans Administration Systemic Sepsis Cooperative Study Group. Effect of high-dose glucocorticoid therapy on mortality in patients with clinical signs of systemic sepsis. N Engl J Med. 1987;317(11):659–665. doi:10.1056/NEJM198709103171102. | ||
Cronin L, Cook DJ, Carlet J, et al. Corticosteroid treatment for sepsis: a critical appraisal and meta-analysis of the literature. Crit Care Med. 1995;23(8):1430–1439. Available from: http://www.ncbi.nlm.nih.gov/pubmed/7634816. Accessed October 10, 2014. | ||
Bollaert PE, Charpentier C, Levy B, Debouverie M, Audibert G, Larcan A. Reversal of late septic shock with supraphysiologic doses of hydrocortisone. Crit Care Med. 1998;26(4):645–650. Available from: http://www.ncbi.nlm.nih.gov/pubmed/9559600. Accessed October 10, 2014. | ||
Briegel J, Forst H, Haller M, et al. Stress doses of hydrocortisone reverse hyperdynamic septic shock: a prospective, randomized, double-blind, single-center study. Crit Care Med. 1999;27(4):723–732. Available from: http://www.ncbi.nlm.nih.gov/pubmed/10321661. Accessed October 10, 2014. | ||
Annane D, Sébille V, Charpentier C, et al. Effect of treatment with low doses of hydrocortisone and fludrocortisone on mortality in patients with septic shock. JAMA. 2002;288(7):862–871. Available from: http://www.ncbi.nlm.nih.gov/pubmed/12186604. Accessed October 10, 2014. | ||
Sprung CL, Annane D, Keh D, et al. Hydrocortisone therapy for patients with septic shock. N Engl J Med. 2008;358(2):111–124. doi:10.1056/NEJMoa071366. | ||
Marik PE, Pastores SM, Annane D, et al. Recommendations for the diagnosis and management of corticosteroid insufficiency in critically ill adult patients: consensus statements from an international task force by the American College of Critical Care Medicine. Crit Care Med. 2008;36(6):1937–1949. doi:10.1097/CCM.0b013e31817603ba. | ||
Lévy Y, Sereti I, Tambussi G, et al. Effects of recombinant human interleukin 7 on T-cell recovery and thymic output in HIV-infected patients receiving antiretroviral therapy: results of a phase I/IIa randomized, placebo-controlled, multicenter study. Clin Infect Dis. 2012;55(2):291–300. doi:10.1093/cid/cis383. | ||
Póvoa P, Salluh JI. Biomarker-guided antibiotic therapy in adult critically ill patients: a critical review. Ann Intensive Care. 2012;2(1):32. doi:10.1186/2110-5820-2-32. | ||
Hotchkiss RS, Monneret G, Payen D. Sepsis-induced immunosuppression: from cellular dysfunctions to immunotherapy. Nat Rev Immunol. 2013;13(12):862–874. doi:10.1038/nri3552. | ||
Gaieski DF, Mikkelsen ME, Band RA. Impact of time to antibiotics on survival in patients with severe sepsis or septic shock in whom early goal-directed therapy was initiated in the emergency department. Crit Care Med. 2010;38:1045–1053. | ||
Daniels R, Nutbeam T, McNamara G, Galvin C. The sepsis six and the severe sepsis resuscitation bundle: a prospective observational cohort study. Emerg Med J. 2011;28(6):507–12. | ||
Appelboam R, Tilley R, Blackburn J. Time to antibiotics in sepsis. Crit Care. 2010;14(Suppl 1):50. | ||
Levy MM, Dellinger RP, Townsend SR, et al. The Surviving Sepsis Campaign: results of an international guideline-based performance improvement program targeting severe sepsis. Crit Care Med. 2010; 38:1–8. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
