Back to Journals » Journal of Multidisciplinary Healthcare » Volume 7
Is there an increased risk of hip fracture in multiple sclerosis? Analysis of the Nationwide Inpatient Sample
Authors Bhattacharya R, Vaishnav N, Dubinsky R
Received 21 September 2013
Accepted for publication 27 November 2013
Published 13 February 2014 Volume 2014:7 Pages 119—122
DOI https://doi.org/10.2147/JMDH.S54786
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Rajib K Bhattacharya, Niralee Vaishnav, Richard M Dubinsky
Departments of Endocrinology, Metabolism and Genetics and Neurology, University of Kansas Medical Center, Kansas City, KS, USA
Background: Impaired ambulation, frequent falls, and prolonged immobilization combined with the high rate of vitamin D deficiency in people with multiple sclerosis (MS) could lead to an increased risk of hip fracture.
Methods: A retrospective cohort analysis of 20 years of the Nationwide Inpatient Sample (AHRQ.gov), a 20% stratified yearly sample of USA hospital admissions from the year 1988–2007, was performed. Based on International Classification of Diseases Ninth Revision (ICD9) codes, admissions with a primary diagnosis of acute hip fracture (ICD9 code 226.xx) and a secondary diagnosis of MS (ICD9 code 340) was identified. Indirect adjustment was used to compare the prevalence of MS in this population with that of the USA. Significance was set a priori at P<0.0001 due to the large number of records and multiple comparisons.
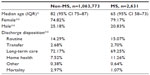
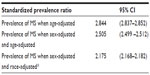
Results: A total of 1,066,404 hip fracture admissions were identified and 0.25% had MS. Those with MS were younger, had lower mortality rates (0.25% for people with MS versus 2.97% for those without MS, P<0.0001) and lower rates of discharge to nursing home or rehabilitation (69.25% for people with MS versus 72.17% for those without MS, P<0.0001). When compared with the population prevalence, the predicted prevalence of MS among patients with hip fracture was 2.844 (95% confidence interval [CI] 2.837–2.852) greater than expected when adjusted for age, 2.505 (95% CI 2.499–2.512) when adjusted for sex and age, and 2.175 (95% CI 2.168–2.182) when adjusted for race (white, black). Race was specified for only 65% of the sample.
Conclusion: In this nationwide sample of 20 years of hospital admissions in the USA, the prevalence of MS in the population with hip fracture was greater than twice that predicted, and MS patients suffered an acute fracture at an earlier age.
Keywords: osteoporosis, patients at risk, multiple sclerosis
Introduction
Multiple sclerosis (MS) is a chronic inflammatory disease of the myelin sheath that results in progressive immobilization, muscle weakness, poor balance, and an increased risk of falls.1 When compared with healthy individuals, bone mineral density (BMD) in MS patients is significantly reduced.2 Multiple studies have found the femoral bone to be affected more and the bone disease to be more severe in the subset of patients with progressive MS.1,3,4 Furthermore, individuals with MS are exposed to steroid therapy and tend to have hypovitaminosis D from sun avoidance, contributing to bone loss.
The chronic nature of MS results in continued inflammation and activation of proinflammatory cytokines that disturb the balance between activation of osteoclastogenesis via osteoprotegerin and inhibition of osteoclastogenesis via receptor activator of nuclear factor kappa B ligand.3 This shift in continuum towards activation of osteoclastogenesis results in ongoing bone loss. Coupled with physical inactivity, a chronic debilitating neurological disorder like MS leads to continued bone loss.5
Currently, patients are treated for osteoporosis based on history of a fragility fracture, BMD that is 2.5 standard deviations below the BMD of a young adult reference population, and if the 10-year risk for a hip fracture is greater than 3% or the 10-year risk for a major osteoporotic fracture is greater than 20% based on the Fracture Risk Assessment Tool (FRAX).6 Although MS patients have higher rates of hip fracture as shown in previous studies1,7 and lower BMD when compared with patients without MS, FRAX may underestimate their risk because the calculation does not incorporate risk factors such as hypovitaminosis D and immobility.
The Nationwide Inpatient Sample (NIS, AHRQ.gov), is a 20% stratified sample of all acute care hospitalizations in the USA and is available from 1988 through 2011. This administrative dataset is used to study health care utilization, hospital outcomes, and disease burden.4 The purpose of this study was to analyze acute hip fracture admissions over the last 20 years to determine if the prevalence of MS is increased in these cases compared with the general population.
Materials and methods
Population
Using retrospective cohort analysis of the NIS from 1988 to 2007 and clinical classification software to redact International Classification of Diseases Ninth Revision (ICD9) diagnostic and procedure codes, we set our inclusion criteria as those patients with a primary diagnosis of any type of hip fracture (ICD9 code 226.xx) and defined the cohorts by the secondary diagnosis of MS (ICD9 code 340). Initial analysis of the entire sample showed an age range from 18 to 123 years, showing admissions that were likely to be miscoded or otherwise in error. We dropped the bottom and top 5% based on age. This methodology was used in prior publications by the authors.5
Statistical analysis
To analyze the effects of time, we divided the records into four cohorts based on 5-year periods, ie, 1988–1992, 1993–1997, 1998–2002, and 2003–2007. SAS version 9.1 software (SAS Institute Inc., Cary, NC, USA) was used for the analysis. Comparison of categorical data was undertaken using χ2. Since initial analysis of the entire cohort showed that age was skewed, the Kruskal–Wallis test was used for comparison. Unique identifiers in the NIS prevented identification of multiple admissions for the same subject.
The primary purpose of this study was to determine if MS was overrepresented in this population of individuals admitted for hip fracture. We used indirect standardization using the prevalence of MS based on the National Health Interview Survey by Noonan et al to determine the number of expected MS cases based on the entire cohort of hip fracture patients.8,9 This was calculated based on age, sex, and, for the proportion where race was available, for whites and blacks. Discharge disposition was a secondary outcome. Because of the large number of records and multiple comparisons, P was set a priori at <0.0001.
Results
MS was a secondary diagnosis in 0.25% of 1,066,404 hip fracture admissions. Over the 20 years of this dataset, the proportion of patients with MS increased from 0.21% to 0.31%. There was less mortality (1.07% in MS patients versus 2.97% in non-MS patients, P<0.0001, Table 1) and a lower rate of discharge to nursing home or rehabilitation (69.25% for MS patients versus 72.17% for non-MS patients, P<0.0001, Table 1) for persons with MS. The effect of time did not result in significant differences in mortality and discharge disposition. With indirect standardization, the prevalence of MS among patients with hip fracture was 2.844 (95% confidence interval [CI] 2.837–2.852, Table 2) predicted when age-adjusted, 2.505 (95% CI 2.499–2.512, Table 2) when sex-adjusted and age-adjusted, and 2.175 (95% CI 2.168–2.182, Table 2) when sex-adjusted and race-adjusted (white, black). Race was specified for 65% of the sample.
Discussion
Data from this retrospective study encompassing hospital admissions in the USA over 20 years suggest an increased fracture risk in MS patients. This prevalence was over two times greater than in the non-MS cohort and was similar to findings from the English National Hospital Episode Statistics database which demonstrated a relative risk for femoral fracture of 2.79 in patients with MS.7 MS patients were also significantly younger at time of fracture, with a median age of 65 years for MS patients versus 82 years for non-MS patients. These younger MS patients are less likely to have comorbidities than their non-MS counterparts, which helps to explain their reduced need for discharge to a nursing home and reduced mortality.
Previous studies have shown decreased BMD from hypovitaminosis D and glucocorticoid treatment in patients with MS.3,10 In addition, people with MS are also at increased risk for fractures due to frequent falls as a result of reduced muscle strength, visual deficits, and problems with balance and coordination. In fact, a 2009 study revealed that 72% of women with MS self-reported impaired mobility after the age of 50 years.11 Studies have also shown reduced BMD measurements in secondary progressive MS when compared with relapsing-remitting MS, suggesting that a longer duration of disease may result in greater accrual of risk factors and worsening BMD.1
The World Health Organization developed the FRAX tool to identify patients aged 40–90 years at risk for a major osteoporotic fracture or hip fracture at 10 years.12 The FRAX incorporates individual risk factors that increase the risk for osteoporosis, such as glucocorticoid use, history of fractures, smoking, and alcohol use to allow identification of individuals at greatest risk for fracture. However, the FRAX calculator does not account for risk factors commonly found in MS and other debilitating diseases, such as Parkinson’s disease, that result in higher fracture rates, such as immobility, imbalance, frequent falls, and low vitamin D status.5 Thus, even though MS patients have higher rates of hip fractures as shown in our study, the calculated FRAX score underestimates the 10-year fracture risk for persons with MS. Clinicians should assess for the presence of these specific risks to allow for risk factor modification, subsequent prevention of future fractures, and early initiation of treatment for osteoporosis.
In addition to this, clinicians should promote physical activity because immobility is a significant part of MS, and these patients have bone loss due to a lack of mechanical stress-related loading and off-loading that induces osteoblast bone formation and maintenance.3,12
The strengths of our study include it being a large retrospective analysis over 20 years. Its limitations include a lack of information on preadmission functional status, medication use, severity and duration of MS, and the rate of falls in the MS cohort compared with the non-MS cohort. Further stratification of MS patients using information on specific risk factors, such as number of falls, level of mobility, and other known contributors to low BMD such as vitamin D status and type of MS, will enable identification of significant risk factor(s) and early intervention to improve BMD and fracture rate.
Conclusion
People with MS have a greater than two times higher risk for fractures that is independent of age, sex, and race, and they are sustaining these fractures at a significantly younger age. Several unique risk factors have been suggested for the increased fracture risk and lower BMD in patients with MS. These risk factors are not included in the FRAX calculation, resulting in an underestimation of the 10-year fracture risk in patients with MS. Thus, health care providers who encounter MS patients, such as physical therapists, neurologists, orthopedic surgeons, and endocrinologists, should incorporate these risk factors in their decision-making when determining the risk for osteoporotic fracture and initiation of therapy to prevent and/or treat osteoporosis in MS patients.
Disclosure
This work was presented in part at the annual meeting of the American Academy of Neurology, New Orleans, LA, USA, April 21–28, 2012. Otherwise, the authors report no conflicts of interest in this work.
References
Zikan V. Bone health in patients with multiple sclerosis. J Osteoporos. 2011;2011:596294. | |
Moen SM, Celius EG, Sandvik L, Nordsletten L, Eriksen EF, Holmøy T. Low bone mass in newly diagnosed multiple sclerosis and clinically isolated syndrome. Neurology. 2011;77:151–157. | |
Dabbaghmanesh MH, Yousefipour GA. Bone loss with multiple sclerosis: effect of glucocorticoid use and functional status. Iran Red Crescent Med J. 2011;13:9–14. | |
Dionyssiotis Y. Bone loss and fractures in multiple sclerosis: focus on epidemiologic and physiopathological features. Int J Gen Med. 2011;4:505–509. | |
Bhattacharya RK, Dubinsky RM, Lai SM, Dubinsky HM. Is there an increased risk of hip fracture in Parkinson disease (PD)? A Nationwide Inpatient Sample (NIS). Mov Disord. 2012;27:1440–1443. | |
National Osteoporosis Foundation. Newly Revised 2013 Clinician’s Guide to Prevention and Treatment of Osteoporosis. Available from: http://nof.org/files/nof/public/content/resource/913/files/580.pdf. Accessed January 8, 2014. | |
Ramagopalan SV, Seminog O, Goldacre R, Goldacre MJ. Risk of fractures in patients with multiple sclerosis: record-linkage study. BMC Neurol. 2012;12:135. | |
Noonan CW, Kathman SJ, White MC. Prevalence estimates for multiple sclerosis in the United States and evidence of an increasing trend for women. Neurology. 2002;58:136–138. | |
International Agency for Research on Cancer. Statistical Methods in Cancer Research, Volume II: The Design and Analysis of Cohort Studies, IARC Scientific Publications, No 82. Available from: http://www.iarc.fr/en/publications/pdfs-online/stat/sp82/SP82.pdf. Accessed January 8, 2014. | |
Nieves J, Cosman E, Herbert J, Shen V, Lindsay B. High prevalence of vitamin D deficiency and reduced bone mass in multiple sclerosis. Neurology. 1994;44:1687–1692. | |
Marrie RA, Cutter G, Tyry T, Villmer T. A cross-sectional study of bone health in multiple sclerosis. Neurology. 2009;73:1394–1398. | |
World Health Organization. Atlas: Multiple Sclerosis Resources in the World 2008. Available from: http://whqlibdoc.who.int/publications/2008/9789241563758_eng.pdf. Accessed June 2013. |
 © 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.