Back to Journals » Neuropsychiatric Disease and Treatment » Volume 11
Influence of 5-HT1A and 5-HTTLPR genetic variants on the schizophrenia symptoms and occurrence of treatment-resistant schizophrenia
Authors Terzic T, Kastelic M, Dolzan V, Plesnicar B
Received 27 October 2014
Accepted for publication 10 December 2014
Published 20 February 2015 Volume 2015:11 Pages 453—459
DOI https://doi.org/10.2147/NDT.S76494
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Roger Pinder
Tea Terzić,1 Matej Kastelic,2 Vita Dolžan,2 Blanka Kores Plesničar1
1Ljubljana University Psychiatric Hospital, Ljubljana, Slovenia; 2Pharmacogenetics Laboratory, Institute of Biochemistry, Faculty of Medicine, University of Ljubljana, Ljubljana, Slovenia
Abstract: This study aimed to explore the influence of two genetic polymorphisms of the 5-hydroxytryptamine 1A receptor (5-HT1A) and solute carrier family 6, member 4 (SLC6A4) genes on the clinical symptoms and treatment resistance in Slovenian patients with schizophrenia. A total of 138 patients with schizophrenia were evaluated using the Positive and Negative Syndrome Scale, Brief Psychiatric Rating Scale, Clinical Global Impression, and Global Assessment of Functioning. Based on the selected criteria, 94 patients were included in the treatment-responsive and 44 in the treatment-resistant group. All subjects and 94 controls were genotyped for the 5-HT1A rs6295 and 5-HTTLPR polymorphisms. There were no statistically significant differences in the frequencies of these polymorphisms between the patients with schizophrenia and the control group and between the treatment-resistant and treatment-responsive group of schizophrenia patients. Polymorphisms rs6295 and 5-HTTLPR had an influence on the Global Assessment of Functioning scale score, while 5-HTTLPR also had an influence on the total score of the negative subscale within the Positive and Negative Syndrome Scale. Although we found no effect on progression toward the treatment-resistant schizophrenia, our data suggest that the rs6295 and 5-HTTLPR polymorphisms can influence some clinical symptoms in schizophrenia.
Keywords: genetic polymorphisms, serotonergic system, antipsychotics, SLC6A4, serotonergic receptor
Introduction
Treatment-resistant schizophrenia represents a significant public health problem. Studies have shown that one-fifth to one-third of patients with schizophrenia do not respond to treatment.1 These patients have persistent positive psychotic symptoms (delusions and hallucinations), more pronounced negative symptoms (apathy, blunted affect, lack of spontaneity, and emotional withdrawal) and more pronounced cognitive symptoms (memory and attention impairment) than treatment-responsive patients.1 Furthermore, they stay in the hospital longer and have a very low level of functioning in the community.2
A recent American study showed that schizophrenia is a group of heritable disorders caused by a moderate number of separate genotypic networks associated with several distinct clinical syndromes.3 The serotonin system plays an important role in schizophrenia. The role of genetic variants of serotonin (5-HT) receptors in treatment-resistant schizophrenia has already been investigated.4 The serotonergic system is involved in the pharmacological mechanisms of atypical antipsychotics, which are widely used for the treatment of schizophrenia. 5-HT1A is a subtype of the serotonergic receptor that has an important influence on dopamine release.5 When serotonin acts on 5-HT1A receptors, it accelerates dopamine release in the prefrontal cortex and consequently improves the negative, cognitive and affective symptoms of schizophrenia.5 5-HT1A receptors have an important role in the modulation of mood, cognition and motor behavior6 and in the control of nonpsychotic symptoms,7 which is an important clinical issue in treatment-resistant schizophrenia. The main indication of clozapine is treatment-resistant schizophrenia,8 in which it acts as a weak partial agonist at the level of 5-HT1A receptors.9 In 1999, Wu and Comings reported a common polymorphism in the promoter region of the 5-HT1A gene,10 which was later shown to have a significant association with schizophrenia.11
The serotonin transporter (5-HTT), encoded by the SLC6A4 gene, is a major regulator of serotonin function.12 5-HTT is specific for serotonin and helps to terminate its actions by pumping it out of the synapse.5 5-HTTLPR is a 44-bp insertion/deletion polymorphism in the promoter region of SLC6A4 that has been frequently studied in a number of psychiatric disorders.13,14 It has also been shown to have an important association with schizophrenia.15 Indeed, some previous studies examined the influence of 5-HTTLPR variants on the symptoms and treatment response in schizophrenia.16,17
An early response to antipsychotic treatment is important for schizophrenia patients, as it predicts further treatment effectiveness.18 Classification of the genes responsible for heritable components of various psychiatric disorders is crucial to the advancement of our understanding of the underlying neurobiology and pathology of complex psychiatric diseases.19 As responses to psychotropic medication are complex, the identification of the key phenotypic measures for their definition is still a major issue in psychiatry and pharmacogenomics and has as yet been only partially implemented in the clinical setting.20
The present study investigated the association between the genetic variants of the 5-HT1A and SLC6A4 genes and the clinical symptoms and development of treatment-resistant schizophrenia.
Materials and methods
Sample collection and DNA preparation
Patients diagnosed with schizophrenia according to the Diagnostic and Statistical Manual IV were randomly recruited from the outpatient unit of the Ljubljana University Psychiatric Clinic (Slovenia). Their psychopathological symptoms were assessed using the Positive and Negative Syndrome Scale (PANSS),21 Brief Psychiatric Rating Scale (BPRS),22 Clinical Global Impression (CGI) Scale,23 and Global Assessment of Functioning (GAF).24
The inclusion criteria for the treatment-resistant group were based on the definition of Conley and Kelly1 and included patients who did not respond to treatment with at least two different antipsychotics (at least one being atypical) at doses equivalent to more than 400–600 mg chlorpromazine, for a period of 6 weeks. Furthermore, they showed a moderate item score (≥4) on at least two of four symptom items according to PANSS (P2, P3, P6, and G9) and at least moderately severe illness as rated by the total BPRS score (≥45), with no stable period of good social and/or occupational functioning within the last 5 years.1 The inclusion criteria for the treatment-responsive group were based on those of Andreasen et al25 and van Os et al.26 Treatment responders had achieved remission and had an item score of ≤3 on the selected symptom items according to PANSS (P1, P2, P3, P6, N1, N4, N6, G5, and G9). The exclusion criteria were the presence of another mental or somatic disorder, poor compliance to treatment, and the occurrence of important side effects during previous antipsychotic treatments. Healthy blood donors constituted the control group. The chlorpromazine-equivalent daily dose of antipsychotics administered to each patient was calculated according to the guidelines for atypical antipsychotics,27 for fluphenasine decanoate,28 and for classic antipsychotics.29
The study was approved by The Slovenian Ethics Committee for Research in Medicine. Written informed consent was obtained from each subject prior to his/her inclusion in the study.
Genotyping method
Genomic DNA was isolated from peripheral blood leukocytes using Qiagen FlexiGene kits (Qiagen, Hilden, Germany). Blood samples (5 mL) were taken from patients, and cells from the blood donation were retrieved for the control group. Genotyping was performed blind to the patient clinical status and was carried out using fluorescence-based competitive allele-specific polymerase chain reaction (KASPar) assays according to the manufacturer’s instructions (KBiosciences, Herts, UK). Two functional polymorphisms were studied, 5-HT1A rs6295 and 5-HTTLPR. The dominant allele model was followed and the CG and GG genotypes for 5-HT1A rs6295 were grouped. For the 5-HTTLPR genotypes, a two-stage genotyping approach was used, with the biallelic 5-HTTLPR genotypes (L and S alleles) determined first. The SS and SL genotypes were grouped as in previous studies.12,16 In the second step, the A → G substitution within the L allele was identified, so that the LA represented the common allele and the LG the polymorphic allele. The LG allele can be considered similar to the S allele in terms of transcriptional efficiency.30
The frequencies of the SL and LALGS alleles for 5-HTTLPR were in the Hardy–Weinberg equilibrium (P=0.94, P=0.24, respectively). The frequencies of HTR1A rs6295 were not in the Hardy–Weinberg equilibrium (P=0.012), but matched those found in the single-nucleotide polymorphism database. The frequencies of HTR1A rs6295 in the control group were in the Hardy–Weinberg equilibrium (P=0.103).
Statistical analysis
Statistical analysis was carried out using the SPSS software (Version 21.0) for Windows. The values of the variables are presented as arithmetic means with standard deviations or as frequencies or other descriptive statistical forms. The dominant genetic model was used, and the associations of having at least one minor allele versus having two wild-type alleles were tested. Association tests between the genotypes and the demographic traits were carried out with χ2 tests and Mann–Whitney U-tests. Association tests between the genotypes and the clinical responses were performed using analysis of covariance, with the current antipsychotic dose acting as a confounder. The differences in allele frequencies between responsive and resistant schizophrenic patients were assessed using χ2 tests. The limit of statistical significance was set at 0.05.
Results
Among the 138 patients with schizophrenia included in the study (70 female, 68 male), 94 met the criteria for the treatment-responsive group and 44 for the treatment-resistant group. The control group consisted of 94 healthy blood donors. All subjects were of Slovenian origin.
Some significant differences in the demographical data were found between the treatment-responsive and treatment-resistant groups. The treatment-resistant group included 28 (63.6%) male and 16 (36.4%) female patients, while the treatment-responsive group included 40 (42.6%) male and 54 (57.4%) female patients. The treatment-resistant group had significantly more male than female patients (P=0.021). The first psychotic episode occurred at an average age of 24.26 years in the treatment-resistant group and 28.12 years in the treatment-responsive group, which also represents a significant difference (P=0.005). Treatment-resistant patients had a significantly higher number of psychiatric hospitalizations (P<0.001) and had received significantly higher doses of antipsychotic agents (P<0.05) compared to treatment responders. Most of the patients were prescribed more than one antipsychotic at the time of the inclusion in the study. Clozapine was prescribed to 58 patients with schizophrenia, 44 of them were treatment resistant and 14 were treatment responsive. Furthermore, 28 patients were prescribed risperidone, 25 aripiprazole, 21 fluphenazine, 19 zuclopenthixol, 18 quetiapine, 13 amisulpride, and 12 olanzapine, while other prescribed antipsychotics were less frequent (paliperidone, ziprasidone, flupentixol, haloperidol, and promazine).
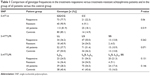
The frequencies of 5-HT1A rs6295 in the group of all patients included in the study were 81.9% for GG/CG and 18.1% for CC, while the frequencies in the control group were 85.1% for GG/CC and 14.9% for CC. There were no significant differences in the frequencies of the polymorphisms either between the group of all patients and the control group (P=0.519) or between the treatment-responsive and treatment-resistant patients (P=0.06) (Table 1).
The frequencies of 5-HTTLPR in the group of all patients were 37.7% for LL, 51.4% for LS, and 10.9% for SS. The frequencies of the three-allelic 5-HTTLPR genotypes were 28.3% for LA LA, 54.3% for LA S or LA LG, and 17.4% for LGLG, LGS, or SS. In the control group, the frequencies were 50.0% for LL, 36.2% for LS, 13.8% for SS, 40.4% for LA LA, 43.6% for LA S or LA LG, and 16.0% for LGLG, LGS or SS (Table 1). There were no significant differences in the frequencies of the allelic variants between the group of all patients and the control group (P=0.071 and P=0.146) or between the treatment-responsive and treatment-resistant groups of patients (P=0.262 and P=0.131) (Table 1).
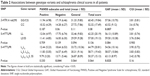
The possible associations between the genotypes and severity of symptoms in all patients were also investigated. An association between the 5-HT1A rs6295 and GAF (P=0.007) was found. Patients carrying the CC genotype had higher GAF scores compared to those with the CG or GG genotypes, which indicates better global patient functioning. No significant associations were found between the 5-HT1A rs6295 variants and the other clinical scores (Table 2).
No significant association was found between the LS carriers of 5-HTTLPR and the severity of symptoms either. However, there was an association between the three-allelic 5-HTTLPR polymorphism and GAF (P=0.025) and the negative subscale of PANSS (P=0.044). Patients with the LG or S alleles had higher GAF scores and lower total scores on the negative subscale of PANSS compared to those with at least one LA allele, which means better patient functioning and fewer negative symptoms (Table 2).
Discussion
Our study investigated the influence of 5-HT1A rs6295 and 5-HTTLPR on the occurrence of schizophrenia and treatment-resistant schizophrenia and clinical symptoms in Slovenian patients.
Demographical characteristics in the treatment-resistant group were as expected. Male predominance and an earlier onset of the first psychotic episode in treatment-resistant schizophrenia patients have already been described in other studies.31 These patients had a higher number of psychiatric hospitalizations and had received significantly higher doses of antipsychotic agents compared to treatment responders, which has also been reported in other studies.32 Among the prescribed antipsychotics clozapine, aripiprazole, haloperidol, olanzapine, quetiapine, and ziprasidone act as partial agonists on 5-HT1A and risperidone as an antagonist on 5-HT1A. 5-HTTLPR genetic variants seem to affect the 5-HT1A receptor binding. A PET (positron emission tomography) study reported that 5-HT1A receptor binding potential values were lower in all brain regions in subjects with 5-HTTLPR SS or SL genotypes than in those with LL genotypes.33 The lower transcriptional efficiency associated with the S allele of the 5-HTTLPR may lead to decreased 5-HTT function, which in turn may lead to a lifelong increase in 5-HT tone, which may in turn desensitize and downregulate 5-HT1A receptors.33
Our data showed no significant influence of the 5-HT1A rs6295 allelic variants on the occurrence of schizophrenia, although some studies have indicated this association.11 Similarly, there was no increased risk for treatment-resistant schizophrenia in the 5-HT1A variants, although activation of these receptors can influence adult neurogenesis34 and might therefore influence the clinical outcome of the disease.
The 5-HTTLPR allelic variants also had no influence on increased risk for schizophrenia, which is consistent with prior studies.35 Furthermore, no association was found between 5-HTTLPR and treatment-resistant schizophrenia. However, a Croatian study reported that 5-HTTLPR SS carriers were less likely to develop treatment-resistant schizophrenia compared to those with all other 5-HTTLPR genotypes and that LAS carriers were almost three times more likely to develop treatment-resistant schizophrenia compared to SS carriers.36 Reduced function of the serotonin transporter means higher serotonin concentrations for downstream regulation of 5-HT receptors and could probably play a factor in creating more favorable conditions for antipsychotic treatment, with a reduced probability of developing treatment-resistant schizophrenia.36 The difference from our study could be explained in the different sample size and different inclusion criteria for the treatment-resistant schizophrenia. In the Croatian study, there were 53.2% of treatment-resistant patients,36 which is a considerably higher percentage than in our study.
Allelic variants of 5-HT1A rs6295 showed a correlation with the GAF score. The GAF score was also shown to correlate with positive and negative symptoms, as well as with agitation levels.37 Although no significant associations were found between the 5-HT1A rs6295 variants and the other clinical scores, it can be assumed that the CC genotype is associated with better patient functioning. These data are in agreement with the suggestion that the occurrence of a G allele at this locus prevents the binding of putative repressor proteins, which leads to enhanced gene expression and reduced serotonergic neurotransmission.38 Other studies have reported similar data, with the G allele being involved in reduced serotonergic neurotransmission. Two studies described an association between the CC genotype of 5-HT1A rs6295 and greater improvement in negative symptoms following treatment, compared with the CG or GG genotypes.39,40
An association was also found between the LG or S alleles and higher GAF scores or lower scores on the negative subscale of PANSS, while other studies have reported conflicting data regarding this association. An American study reported that the LL carriers had worse clinical schizophrenia outcomes when compared with the LS/SS carriers.16 On the other hand, in a Korean population, the SS genotype of 5-HTTLPR was found to be connected to a higher negative symptom score and general psychopathology score, compared to the LS/LL carriers.41 The S allele has even been associated with violent suicide attempts in patients with schizophrenia.42 A Slovenian study showed that the LG or S alleles of 5-HTTLPR are associated with lower improvement in schizophrenia symptoms during treatment.43 In patients with depressive disorder, the L variants of 5-HTTLPR were associated with a higher probability of remission and response to selective serotonin reuptake inhibitors.44 Theoretically, the L and S alleles can differentially modulate the transcription of the SLC6A4 gene. The S allele reduces the transcriptional efficiency of the gene, which results in reduced 5-HTT expression and serotonin uptake.12 Evidence suggests that the LG allele might have a transcriptional activity similar to that of the S allele, while only the LA allele increases transcriptional activity.45 However, it is possible that other mechanisms, such as regulatory posttranslational processing of 5-HTT, can influence receptor activity.46
Our study had several limitations. Treatment resistance was defined retrospectively and a part of the initial group of patients could not be classified because of insufficient information. The criteria for treatment-resistant schizophrenia remain to be fully defined. A number of studies have proposed criteria for treatment resistance in patients with schizophrenia,8,47 as well as the guidelines for their treatment.48 Furthermore, the P-values were not corrected for multiple comparisons. The data should be interpreted with caution because of the small sample size and borderline statistical significance, so there is a chance of false-positive findings.
The present study examined the influence of two genetic polymorphisms in the 5-HT1A gene and SLC6A4 gene on clinical symptoms and treatment resistance in patients with schizophrenia. The 5-HT1A rs6295 and the 5-HTTLPR polymorphisms have an influence on global patient functioning, and the 5-HTTLPR has an influence on the negative symptoms of schizophrenia. However, neither of the polymorphisms have any impact on the development of treatment-resistant schizophrenia. Because a limited sample size was used, these findings should be replicated in larger data sets.
Acknowledgments
We thank Anja Plemenitaš, who contributed the blood samples of the healthy blood donors for the study. This study was financially supported by the Slovenian Research Agency (ARRS grant numbers P1-0170 and P3-0366).
Disclosure
The authors report no conflicts of interest in this work.
References
Conley RR, Kelly DL. Management of treatment resistance in schizophrenia. Biol Psychiatry. 2001;50(11):898–911. | ||
Lindenmayer JP, Khan A. Assessment of therapy-resistant schizophrenia. Adv Biol Psychiatry. 2010;26:9–32. | ||
Arnedo J, Svrakic DM, Del Val C, et al. Uncovering the hidden risk architecture of the schizophrenias: confirmation in three independent genome-wide association studies. Am J Psychiatry. 2014; 172:1–15. | ||
Ji X, Takahashi N, Saito S, et al. Relationship between three serotonin receptor subtypes (HTR3A, HTR2A and HTR4) and treatment-resistant schizophrenia in the Japanese population. Neurosci Lett. 2008;435(2):95–98. | ||
Stahl SM. Stahl’s Essential Psychopharmacology. 3rd ed. New York: Cambridge University Press; 2008. | ||
Barnes NM, Sharp T. A review of central 5-HT receptors and their function. Neuropharmacology. 1999;38(8):1083–1152. | ||
Newman-Tancredi A. The importance of 5-HT1A receptor agonism in antipsychotic drug action: rationale and perspectives. Curr Opin Investig Drugs. 2010;11(7):802–812. | ||
Kane J, Honigfeld G, Singer J, Meltzer H. Clozapine for the treatment-resistant schizophrenic. A double-blind comparison with chlorpromazine. Arch Gen Psychiatry. 1988;45(9):789–796. | ||
Newman-Tancredi A, Chaput C, Verriele L, Millan MJ. Clozapine is a partial agonist at cloned, human serotonin 5-HT1A receptors. Neuropharmacology. 1996;35(1):119–121. | ||
Wu S, Comings DE. A common C-1018g polymorphism in the human 5-HT1A receptor gene. Psychiatr Genet. 1999;9(2):105–106. | ||
Huang YY, Battistuzzi C, Oquendo MA, et al. Human 5-ht1a receptor C(-1019)G polymorphism and psychopathology. Int J Neuropsychopharmacol. 2004;7(4):441–451. | ||
Lesch KP, Bengel D, Heils A, et al. Association of anxiety-related traits with a polymorphism in the serotonin transporter gene regulatory region. Science. 1996;274(5292):1527–1531. | ||
Manchia M, Zai CC, Squassina A, Vincent JB, De Luca V, Kennedy JL. Mixture regression analysis on age at onset in bipolar disorder patients: investigation of the role of serotonergic genes. Eur Neuropsychopharmacol. 2010;20(9):663–670. | ||
Crisafulli C, Fabbri C, Porcelli S, et al. Pharmacogenetics of antidepressants. Front Pharmacol. 2011;2:6. | ||
Vijayan NN, Iwayama Y, Koshy LV, et al. Evidence of association of serotonin transporter gene polymorphisms with schizophrenia in a south Indian population. J Hum Genet. 2009;54(9):538–542. | ||
Malhotra AK, Goldman D, Mazzanti C, Clifton A, Breier A, Pickar D. A functional serotonin transporter (5-HTT) polymorphism is associated with psychosis in neuroleptic-free schizophrenics. Mol Psychiatry. 1998;3(4):328–332. | ||
Bozina N, Medved V, Kuzman MR, Sain I, Sertic J. Association study of olanzapine-induced weight gain and therapeutic response with SERT gene polymorphisms in female schizophrenic patients. J Psychopharmacol. 2007;21(7):728–734. | ||
Giegling I, Porcelli S, Balzarro B, et al. Antipsychotic response in the first week predicts later efficacy. Neuropsychobiology. 2012; 66(2):100–105. | ||
Kenna GA, Roder-Hanna N, Leggio L, et al. Association of the 5-HTT gene-linked promoter region (5-HTTLPR) polymorphism with psychiatric disorders: review of psychopathology and pharmacotherapy. Pharmgenomics Pers Med. 2012;5:19–35. | ||
Squassina A, Manchia M, Manolopoulos VG, et al. Realities and expectations of pharmacogenomics and personalized medicine: impact of translating genetic knowledge into clinical practice. Pharmacogenomics. 2010;11(8):1149–1167. | ||
Kay SR, Flszbein A, Opfer LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13(2):261. | ||
Overall JE, Gorham DR. The brief psychiatric rating scale. Psychol Rep. 1962;10(3):799–812. | ||
Garver DL, Nair TR, Christensen JD, Holcomb J, Ramberg J, Kingsbury S. Clinical global impression (CGI). Assessment Manual for Psychopharmacology. 1976;21(1):125–126. | ||
Hall RCW. Global assessment of functioning: a modified scale. Psychosomatics. 1995;36(3):267–275. | ||
Andreasen NC, Carpenter WT, Kane JM, Lasser RA, Marder SR, Weinberger DR. Remission in schizophrenia: proposed criteria and rationale for consensus. Am J Psychiatr. 2005;162(3):441–449. | ||
van Os J, Burns T, Cavallaro R, et al. Standardized remission criteria in schizophrenia. Acta Psychiatr Scand. 2006;113(2):91–95. | ||
Woods SW. Chlorpromazine equivalent doses for the newer atypical antipsychotics. J Clin Psychiatry. 2003;64(6):663–667. | ||
Atkins M, Burgess A, Bottomley C, Riccio M. Chlorpromazine equivalents: a consensus of opinion for both clinical and research applications. Psychiatr Bull R Coll Psychiatr. 1997;21(4):224–226. | ||
Bazire S. Psychotropic Drug Directory 2005: The Professionals’ Pocket Handbook and Aide Memoire. London: Fivepin Publishing LTD; 2005. | ||
Hu XZ, Lipsky RH, Zhu G, et al. Serotonin transporter promoter gain-of-function genotypes are linked to obsessive-compulsive disorder. Am J Hum Genet. 2006;78(5):815–826. | ||
Meltzer HY, Rabinowitz J, Lee MA, et al. Age at onset and gender of schizophrenic patients in relation to neuroleptic resistance. Am J Psychiatry. 1997;154(4):475–482. | ||
Castro APWD, Elkis H. Rehospitalization rates of patients with schizophrenia discharged on haloperidol, risperidone or clozapine. Rev Bras Psiquiatr. 2007;29(3):207–212. | ||
David SP, Murthy NV, Rabiner EA, et al. A functional genetic variation of the serotonin (5-HT) transporter affects 5-HT1A receptor binding in humans. J Neurosci. 2005;25(10):2586–2590. | ||
Schreiber R, Newman-Tancredi A. Improving cognition in schizophrenia with antipsychotics that elicit neurogenesis through 5-HT receptor activation. Neurobiol Learn Mem. 2014;110:72–80. | ||
Tsai SJ, Hong CJ, Yu YW, et al. Association study of a functional serotonin transporter gene polymorphism with schizophrenia, psychopathology and clozapine response. Schizophr Res. 2000;44(3):177–181. | ||
Bilic P, Jukic V, Vilibic M, Savic A, Bozina N. Treatment-resistant schizophrenia and DAT and SERT polymorphisms. Gene. 2014;543(1): 125–132. | ||
Goldman M, DeQuardo JR, Tandon R, Taylor SF, Jibson M. Symptom correlates of global measures of severity in schizophrenia. Compr Psychiatry. 1999;40(6):458–461. | ||
Lemonde S, Turecki G, Bakish D, et al. Impaired repression at a 5-hydroxytryptamine 1A receptor gene polymorphism associated with major depression and suicide. J Neurosci. 2003;23(25):8788–8799. | ||
Wang L, Fang C, Zhang A, et al. The – 1019 C/G Polymorphism of the 5-HT1A receptor gene is associated with negative symptom response to risperidone treatment in schizophrenia patients. J Psychopharmacol. 2008;22(8):904–909. | ||
Kim YK, Yoon HK. Effect of serotonin-related gene polymorphisms on pathogenesis and treatment response in Korean schizophrenic patients. Behav Genet. 2011;41(5):709–715. | ||
Pae CU, Kim JJ, Lee SJ, et al. Polymorphism of the serotonin transporter gene and symptomatic dimensions of schizophrenia in the Korean population. Neuropsychobiology. 2003;47(4):182–186. | ||
Bayle FJ, Leroy S, Gourion D, et al. 5HTTLPR polymorphism in schizophrenic patients: further support for association with violent suicide attempts. Am J Med Genet B Neuropsychiatr Genet. 2003; 119B(1):13–17. | ||
Dolzan V, Serretti A, Mandelli L, Koprivsek J, Kastelic M, Plesnicar BK. Acute antipyschotic efficacy and side effects in schizophrenia: association with serotonin transporter promoter genotypes. Prog Neuropsychopharmacol Biol Psychiatry. 2008;32(6):1562–1566. | ||
Porcelli S, Fabbri C, Serretti A. Meta-analysis of serotonin transporter gene promoter polymorphism (5-HTTLPR) association with antidepressant efficacy. Eur Neuropsychopharmacol. 2012;22(4):239–258. | ||
Lipsky RH, Hu XZ, Goldman D. Additional functional variation at the Slc6a4 gene. Am J Med Genet B Neuropsychiatr Genet. 2009; 150B(1):153. | ||
Ramamoorthy S, Giovanetti E, Qian Y, Blakely RD. Phosphorylation and regulation of antidepressant-sensitive serotonin transporters. J Biol Chem. 1998;273(4):2458–2466. | ||
Suzuki T, Remington G, Mulsant BH, et al. Defining treatment-resistant schizophrenia and response to antipsychotics: a review and recommendation. Psychiatry Res. 2012;197(1–2):1–6. | ||
Dold M, Leucht S. Pharmacotherapy of treatment-resistant schizophrenia: a clinical perspective. Evid Based Ment Health. 2014; 17(2):33–37. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.