Back to Journals » OncoTargets and Therapy » Volume 8
Increased risk of severe infections in cancer patients treated with vascular endothelial growth factor receptor tyrosine kinase inhibitors: a meta-analysis
Authors Ma Q, Gu L, Ren Y, Zeng L, Gong T, Zhong D
Received 24 April 2015
Accepted for publication 25 May 2015
Published 28 August 2015 Volume 2015:8 Pages 2361—2374
DOI https://doi.org/10.2147/OTT.S87298
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 5
Editor who approved publication: Professor Daniele Santini
Qing Ma, Li-Yan Gu, Yao-Yao Ren, Li-Li Zeng, Ting Gong, Dian-Sheng Zhong
Department of Oncology, The General Hospital of Tianjin Medical University, Tianjin, People’s Republic of China
Background: Vascular endothelial growth factor receptor tyrosine kinase inhibitors (VEGFR-TKIs) have been widely used in a variety of solid malignancies. Concerns have arisen regarding the risk of severe infections (≥grade 3) with use of these drugs, but the contribution of VEGFR-TKIs to infections is still unknown.
Methods: The databases of PubMed and abstracts presented at oncology conferences’ proceedings were searched for relevant studies from January 2000 to December 2014. Summary incidences, Peto odds ratio (Peto OR), and 95% confidence intervals (CIs) were calculated by using either random-effects or fixed-effects models according to the heterogeneity of included studies.
Results: A total of 16,488 patients from 27 randomized controlled trials were included. The risk of developing severe (Peto OR 1.69, 95% CI: 1.45–1.96, P<0.001) and fatal infections (Peto OR 1.78, 95% CI: 1.13–2.81, P=0.013) was significantly increased in patients treated with VEGFR-TKIs when compared to controls. Exploratory subgroup analysis showed no effect of tumor types, phase of trials, or agent used on the Peto OR of severe infections. When stratified according to specific infectious events, the risks of high-grade febrile neutropenia, pneumonia, fever, and sepsis were increased compared with controls, with Peto ORs of 1.57 (95% CI: 1.30–1.88, P<0.001), 1.79 (95% CI: 1.29–2.49, P<0.001), 5.35 (95% CI: 1.47–19.51, P=0.011), and 3.68 (95% CI: 1.51–8.99, P=0.004), respectively. Additionally, VEGFR-TKIs significantly increased the risk of fatal sepsis (OR 3.66, 95% CI: 1.47–9.13, P=0.005) but not fatal pneumonia (OR 1.34, 95% CI: 0.80–2.25, P=0.26).
Conclusion: The use of VEGFR-TKIs significantly increases the risk of developing severe and fatal infectious events in cancer patients. A close monitoring for any signs of infections is recommended for patients treated with VEGFR-TKIs.
Keywords: VEGFR-TKIs, infections, cancer, randomized controlled trials, meta-analysis
Introduction
Tumor angiogenesis is a complex process that is crucial for tumor growth, invasion, and metastasis.1–3 During the past decades, many new agents targeting vascular endothelial growth factor (VEGF) and its receptors (VEGFRs) have proven to be a successful strategy in patients with cancer. Until now, the US Food and Drug Administration has approved a number of VEGFR tyrosine kinase inhibitors (TKIs) in multiple indications: sunitinib, sorafenib, pazopanib, and axitinib have been approved for patients with metastatic renal cell carcinoma (RCC).4–8 Moreover, sunitinib has been approved for pancreatic neuroendocrine tumors9 and refractory gastrointestinal stromal tumors (GISTs),10 and sorafenib has been approved for advanced hepatocellular carcinoma (HCC)11 and radioiodine-refractory differentiated thyroid carcinoma.12 Additionally, vandetanib has been approved for symptomatic or progressive medullary thyroid cancer,13 and regorafenib has been approved for refractory advanced colorectal cancer14 and GISTs.15
However, the toxicity profiles of VEGFR-TKIs are unique compared with the adverse effects typically associated with traditional cytotoxic anticancer therapies. They include mucocutaneous adverse events,16–19 liver dysfunction,20–23 gastrointestinal perforation,24,25 and cardiovascular toxicities.26–33 Additionally, severe infections (≥grade 3) associated with VEGFR-TKIs have been reported in randomized controlled trials (RCTs). However, the incidence has varied substantially among clinical trials, and there has been no systematic attempt to synthesize the data in order to define the overall incidence and risk of infections associated with these drugs. Therefore, we conducted a systematic review and meta-analysis of RCTs to determine the overall risk of developing severe infection in cancer patients treated with these drugs.
Methods
Data sources
Studies were identified by searching the Cochrane Central Register of Controlled Trials (CENTRAL), PubMed (up to December 2014), Web of Science, and EMBASE, including abstracts from the leading conference proceedings. The search was limited to prospective RCTs published in English. Keywords were sorafenib, nexavar, BAY43-9006, sunitinib, sutent, SU11248, pazopanib, votrient, GW786034, vandetanib, caprelsa, ZD6474, axitinib, AG-013736, cediranib, AZD2171, tivozanib, regorafenib, BAY 73-4506, cabozantinib, brivanib, ramucirumab, IMC-1121B, nintedanib, BIBF 1120, motesanib, randomized controlled trials, and cancer. The search strategy also used text terms such as angiogenesis inhibitors and vascular endothelial growth factor receptor-tyrosine kinase inhibitors to identify relevant information (Supplementary material). When more than one publication or presentation was identified from the same clinical trial, the most recent report with complete information about infectious events was included for analysis. The quality of reports of clinical trials was assessed and calculated using the five-item Jadad scale including randomization, double-blinding, and withdrawals.34
Study selection
The purpose of this study was to determine whether VEGFR-TKIs contribute to the development of severe and fatal infectious events in patients with cancer. Therefore, we only selected those randomized clinical trials that directly compared patients with cancer treated with and without VEGFR-TKIs for analysis. Clinical trials that met the following criteria were included: (1) prospective randomized controlled Phase II and III trials in cancer patients, (2) randomized assignment of patients to VEGFR-TKIs treatment or control in addition to current chemotherapy and/or biological agent, and (3) events or event rate and sample size available for high-grade (grade 3–4) and fatal (grade 5) infectious events. Phase I trials were excluded because of interstudy variability in drug dosing as well as the small number of patients in these trials. Study selection was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement.35
Data extraction and clinical endpoints
Two investigators independently performed data extraction. Agreement between the two data extractors was assessed with the Kappa statistic test. The following information was recorded for each study: first author’s name, year of publication, trial phase, number of patients enrolled, treatment arms, number of patients in treatment and controlled groups, underlying malignancy, median age, median progression-free survival and overall survival, adverse outcomes of interest (infectious events), and name and dosage of VEGFR-TKIs. The following adverse outcomes were considered as infectious events and were included in the analyses: infections (not specified), febrile neutropenia, sepsis, septic shock, fever, bacterial peritonitis, and pneumonia. Adverse events of severe infections (≥grade 3), as assessed and recorded according to the National Cancer Institute’s common terminology criteria (version 2 or 3; http://ctep.cancer.gov), were extracted for analysis, which has been widely used in cancer clinical trials.
Statistical analysis
The principal summary measures were incidence, Peto odds ratio (Peto OR), and corresponding 95% confidence intervals (CIs). For the calculation of incidence, the number of patients experiencing infections and total number of patients treated with VEGFR-TKIs were extracted from the safety profiles of all selected clinical trials; the proportion of patients with infections and 95% CIs were derived for each study.
We also calculated the Peto ORs and 95% CIs of infections in patients assigned to VEGFR-TKIs vs control treatment. For one study that reported zero events in the treatment or control arm, we applied the classic half-integer correction to calculate the relative risk (RR) and variance.36 We also conducted the following prespecified subgroup analyses to find the potential risk factor of infections: tumor types, VEGFR-TKIs, and phase of trials. For each meta-analysis, the Cochran Q statistic and I2 score were first calculated to determine heterogeneity among the proportions of the included trials.37 For P<0.10 values of the Cochran Q statistic, the assumption of homogeneity was deemed invalid, and a random-effects model was reported. Otherwise, results from the fixed-effects model were reported. Additionally, we also calculated the number needed to harm from the absolute difference of the pooled estimates between the two groups. Finally, potential publication biases were evaluated with funnel plots for severe infections, which assessed the relative symmetry of individual study estimates around the overall estimate, followed by Begg’s and Egger’s tests. A two-tailed P-value of <0.05 without adjustment for multiplicity was considered statistically significant. The leave-one-out procedure was also performed for primary endpoint analysis. A two-tailed P-value of <0.05 was considered statistically significant. The results of the meta-analysis were reported as classic forest plots. All statistical analyses were performed by using Version 2 of the Comprehensive MetaAnalysis program (Biostat, Englewood, NJ, USA) and Open Meta-Analyst software version 4.16.12 (Tufts University).
Trial sequential analysis
Trial sequential analyses (TSAs) were performed post hoc to assess the risk of random errors and false-positive results, and to help clarify the need for additional trials. RR was used as effect estimate in a DerSimonian and Laid random-effects model. Zero-event trials were handled by adding 0.5 events to the two arms. We used two-sided tests, type I error set at 5% and power set at 80%. In the TSA based on all trials, the boundaries were calculated with a relative risk reduction set at an arbitrary level of 60% and with model variance-based heterogeneity correction. The incidence of severe infections in the control group was set at 3.3% for cancer patients. TSA was performed in TSA V.0.9 β (http://www.ctu.dk/tsa/).
Results
Search results
Our search yielded 982 clinical studies relevant to VEGFR-TKIs (sunitinib, sorafenib, pazopanib, vandetanib, axitinib, cediranib, tivozanib, regorafenib, cabozantinib, nintedanib, brivanib, ramucirumab, and motesanib). After excluding review articles, Phase I studies, single-arm Phase II studies, case reports, meta-analyses, observation studies, duplicated RCTs, commentaries, letters, and RCTs without adequate infections data (Figure 1), we selected 27 RCTs, including 24 Phase III and three Phase II trials, for the purpose of analysis (Table 1). A total of 16,488 patients from 27 clinical trials were included for analysis. The characteristics of patients and studies are listed in Table 2. Underlying malignancies included non-small-cell lung cancer (NSCLC) (ten trials),38–47 colorectal cancer (three trials),14,48,49 thyroid cancer (three trials),50–52 HCC (two trials),53,54 advanced breast cancer (one trial),55 urothelial cancer (one trial),56 pancreatic cancer (one trial),57 gastric cancer (one trial),58 melanoma (one trial),59 RCC (one trial),60 acute myeloid leukemia (one trial),61 castration-resistant prostate cancer (one trial),62 and GIST (one trial).15 When examining by agent, sorafenib was investigated in seven trials (2,964 patients), vandetanib in seven trials (4,223 patients), sunitinib in five trials (3,167 patients), cediranib in two trials (1,164 patients), regorafenib in two trials (956 patients), motesanib in one trial (1,072 patients), ramucirumab in one trial (1,253 patients), nintedanib in one trial (655 patients), and brivanib in one trial (502 patients). The Cohen–Kappa statistic for agreement between the two reviewers was 0.866 (95% CI: 0.80–0.93).
  | Figure 1 Selection process for prospective randomized controlled trials included in the meta-analysis. |
Trial quality
Randomized treatment allocation sequences were generated in all trials. Twenty-one trials were placebo-controlled and double-blinded. Follow-up time was generally adequate for each trial and included a period of approximately 2–4 weeks after end of therapy on trial. All the trials were of moderately high to high quality (Jadad score 3–5).
RR of severe and fatal infections
Severe infections occurred in 484 out of 8,937 (3.8%) patients receiving VEGFR-TKIs. In the non-TKI group, severe infections occurred in 274 out of 7,767 (3.0%) patients. Subjects in the VEGFR-TKI group were at significantly higher risk of severe infections than subjects in the non-TKI group (OR 1.69, 95% CI: 1.45–1.96, P<0.001; Figure 2). There was no evidence of heterogeneity (Q=31.61, P=0.206, I2=17.76%). Fatal infections occurred in 52 out of 4,923 (1.0%) patients receiving VEGFR-TKIs. In the non-TKI group, fatal infections occurred in 26 out of 4,111 (0.8%) patients. There was significant difference in risk of fatal infections between subjects in the VEGFR-TKI group and those in the non-TKI group (OR 1.78, 95% CI: 1.13–2.81, P=0.013; Figure 3), and there was no evidence of significant heterogeneity (Q=15.0, P=0.31, I2=13.4%). We also did sensitivity analysis to examine the stability and reliability of pooled severe ORs by sequential omission of individual studies. The results indicated that the significance estimate of pooled severe RRs was not significantly influenced by omitting any single study (Figure 4).
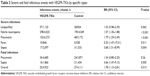
Subgroup analysis of RR of severe infections
To determine whether the observed increase in ORs of developing severe infections was the result of confounding bias, we performed subgroup analyses according to the underlying malignancy, VEGFR-TKIs, and phase of trials. When stratified by tumor types, a significantly increased risk of severe infections was observed in colorectal cancer (OR 1.99, 95% CI: 1.19–3.33, P=0.009) and NSCLC (OR 1.65, 95% CI: 1.39–1.96, P<0.001), while the risk of severe infections was decreased in HCC (OR 0.52, 95% CI: 0.10–2.65, P=0.44; Table 1). However, no significant differences in ORs of severe infections were found among these tumor types (P=0.85). Clinicians should be cautious when interpreting these results due to the limited RCTs of HCC and colorectal cancer included for the OR calculation.
The risk of severe infections might be related to different VEGFR-TKIs. Our results demonstrated that the use of sorafenib (OR 2.11, 95% CI: 1.48–3.00, P<0.011) and sunitinib (OR 2.18, 95% CI: 1.35–3.53, P=0.001) significantly increased the risk of severe infections, while a nonsignificantly increased risk of severe infections was observed in vandetanib, cediranib, and regorafenib (Table 1). Again, no significant differences in ORs of severe infections were found among these drugs (P=0.48). Then, we also carried out a subgroup risk analysis stratified according to phase of trials (Phase II vs Phase III). Patients from Phase III trials had an OR of 1.71 (95% CI: 1.47–1.99, P<0.001), while patients from Phase II studies had an OR of 1.21 (95% CI: 0.60–2.44, P=0.60; Table 1).
TSA assessed the effect of VEGFR-TKIs on severe infections in cancer patients and showed that the required information size was 3,259 which was less than that in our study (n=16,488), and the cumulative Z-curve crossed the trial sequential monitoring boundary for harm, indicating that further studies are unlikely to change the current conclusion (Figure 5).
  | Figure 5 Trial sequential analysis of 27 trials with lower risk of bias reporting severe infections. |
Risk of severe and fatal infections by specific types
Individual specified and nonspecified causes of severe and fatal infections are listed in Table 3. Of those severe infections that were specified, the most common events for severe infections were febrile neutropenia (61.6%). We then calculated the risk of severe infections stratifying trials according to specific type of severe infections. Our results showed that the use of VEGFR-TKIs significantly increased the risk of severe febrile neutropenia (OR 1.57, 95% CI: 1.30–1.88, P<0.001), pneumonia (OR 1.79, 95% CI: 1.29–2.49, P<0.001), fever (OR 5.35, 95% CI: 1.47–19.51, P=0.011), and sepsis (OR 3.68, 95% CI: 1.51–8.99, P=0.004). We also calculated the risk of fatal infections stratifying trials according to specific types of infections; the use of VEGFR-TKIs significantly increased the risk of fatal sepsis (OR 3.66, 95% CI: 1.47–9.13, P=0.005) but not fatal pneumonia (OR 1.34, 95% CI: 0.80–2.25, P=0.26; Table 1).
Publication bias
A funnel plot and both Begg’s and Egger’s tests were performed to assess the publication bias of the selected studies. The shapes of the funnel plots showed no evidence of obvious asymmetry (P=0.61 for OR of severe infections; Figure 6). The results from Egger’s test were not significant (P=0.58).
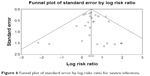  | Figure 6 Funnel plot of standard error by log-risks ratio for severe infections. |
Discussion
During the past decade, identification of the importance of VEGF signal pathway in tumor growth, invasion, and metastasis has led to the development of VEGFR-targeted treatments, which has significantly changed the prognosis of several solid tumors including RCC, HCC, colorectal cancer, and thyroid cancer. Although VEGFR-TKIs are generally well tolerated, infection is an emerging complication with the use of these drugs. Infections can delay treatment or reduce patient compliance with VEGFR-TKI therapies, and the management of infections also increases the cost of cancer treatment. Thus, it is particularly important for all health care practitioners and patients to understand and recognize the risk of infection associated with VEGFR-TKI therapies.
To the best of our knowledge, this is the first and largest meta-analysis evaluating the risk of infections associated with VEGFR-TKIs. In this comprehensive analysis of 16,488 patients, 27 randomized Phase II and III trials using VEGFR-TKIs (sunitinib, sorafenib, pazopanib, axitinib, vandetanib, cediranib, ramucirumab, regorafenib, nintedanib, and motesanib) were included. We did not include Phase I trials in our meta-analysis, since these studies are not randomized and include a wide range of different dosages of drugs. We observed a significant 1.69-fold increase in the risk of high grades of infections with VEGFR-TKIs compared to controls not receiving VEGFR-TKIs. Sensitivity analysis demonstrated that the significance estimate of pooled severe ORs was not significantly influenced by omitting any single study. We also investigated the outcome of VEGFR-TKIs-associated severe infections; our results showed that the use of VEGFR-TKIs significantly increased the risk of fatal infections when compared to non-VEGFR-TKI regimens (P=0.013). However, given that the absolute risk of fatal infections is low, the use of VEGFR-TKIs should be considered in the context of overall survival benefits. As VEGFR-TKIs are increasingly used in cancer patients, it is particularly important for clinicians to understand and recognize the risk of severe and fatal infection.
Given an increased OR of treatment-related infections, it is clear that proper monitoring, immediate intervention, and effective management are crucial to achieve the maximal therapeutic benefit of VEGFR-TKIs. However, there are no specific guidelines for the treatment of VEGFR-TKIs-induced infections because there is a lack of controlled studies addressing the subject. Based on our findings, the following approaches may be considered to reduce the association of VEGFR-TKIs with risk of infections. Before the initiation of VEGFR-TKIs, clinicians must fully treat patients with any active infection and must monitor patients during the course of VEGFR-TKIs treatment. Clinicians should be cautious when adding VEGFR-TKIs, especially sorafenib and sunitinib, to the first-line or second-line therapies for the treatment of NSCLC and colorectal cancers.
Despite the size of this meta-analysis, our study has some limitations. First, this was a trial-level meta-analysis, and confounding variables at the patient level, such as comorbidities, younger age, prior cardiac history, and previous chemotherapeutic exposure, could not be incorporated into the analysis. However, all of the included trials exhibited moderate- or good-quality Jadad scores, and a report suggests that trial-level and patient-level meta-analyses yield similar results. Second, although most of these trials carried out the randomization process adequately, the infectious events are retrospectively collected. Therefore, these data should be interpreted cautiously because the extracted data used for this analysis could not be considered randomized, which somehow compromised the evidence level. Finally, our literature search is limited to articles published in English creating some selection bias. However, our research detects no publication bias using Begg and Egger tests for ORs of severe and fatal infections.
Conclusion
The use of small-molecule VEGFR-TKIs is associated with an increase in the risk of developing severe and fatal infectious events in cancer patients. Close monitoring for any sign of infections is recommended, especially in NSCLC and colorectal cancer patients. Nevertheless, for the average patient, these approved drugs do improve clinical outcomes in their respective indications, and the benefits generally outweigh the risks.
Authors’ contributions
QM and D-SZ designed research. L-YG, YYR, and L-LZ conducted research. TG, D-SZ, and YYR analyzed data. QM wrote the draft. All authors read, reviewed, and approved the final manuscript. D-SZ had primary responsibility for final content. All authors contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work.
Disclosure
All authors declare that they have no potential conflicts of interests.
References
Folkman J. Anti-angiogenesis: new concept for therapy of solid tumors. Ann Surg. 1972;175(3):409–416. | ||
Carmeliet P, Jain RK. Angiogenesis in cancer and other diseases. Nature. 2000;407(6801):249–257. | ||
Folkman J. Role of angiogenesis in tumor growth and metastasis. Semin Oncol. 2002;29(6 suppl 16):15–18. | ||
Motzer RJ, Hutson TE, Cella D, et al. Pazopanib versus sunitinib in metastatic renal-cell carcinoma. N Engl J Med. 2013;369(8):722–731. | ||
Motzer RJ, Escudier B, Tomczak P, et al. Axitinib versus sorafenib as second-line treatment for advanced renal cell carcinoma: overall survival analysis and updated results from a randomised phase 3 trial. Lancet Oncol. 2013;14(6):552–562. | ||
Sternberg CN, Davis ID, Mardiak J, et al. Pazopanib in locally advanced or metastatic renal cell carcinoma: results of a randomized phase III trial. J Clin Oncol. 2010;28(6):1061–1068. | ||
Escudier B, Eisen T, Stadler WM, et al. Sorafenib in advanced clear-cell renal-cell carcinoma. N Engl J Med. 2007;356(2):125–134. | ||
Motzer RJ, Hutson TE, Tomczak P, et al; TARGET Study Group. Sunitinib versus interferon alfa in metastatic renal-cell carcinoma. N Engl J Med. 2007;356(2):115–124. | ||
Raymond E, Dahan L, Raoul JL, et al. Sunitinib malate for the treatment of pancreatic neuroendocrine tumors. N Engl J Med. 2011;364(6):501–513. | ||
Demetri GD, van Oosterom AT, Garrett CR, et al. Efficacy and safety of sunitinib in patients with advanced gastrointestinal stromal tumour after failure of imatinib: a randomised controlled trial. Lancet. 2006;368(9544):1329–1338. | ||
Llovet JM, Ricci S, Mazzaferro V, et al. Sorafenib in advanced hepatocellular carcinoma. N Engl J Med. 2008;359(4):378–390. | ||
Lam ET, Ringel MD, Kloos RT, et al. Phase II clinical trial of sorafenib in metastatic medullary thyroid cancer. J Clin Oncol. 2010;28(14): 2323–2330. | ||
Wells SA, Gosnell JE, Gagel RF, et al. Vandetanib for the treatment of patients with locally advanced or metastatic hereditary medullary thyroid cancer. J Clin Oncol. 2010;28(5):767–772. | ||
Grothey A, Van Cutsem E, Sobrero A, et al; CORRECT Study Group. Regorafenib monotherapy for previously treated metastatic colorectal cancer (CORRECT): an international, multicentre, randomised, placebo-controlled, phase 3 trial. Lancet. 2013;381(9863):303–312. | ||
Demetri GD, Reichardt P, Kang YK, et al; GRID Study Investigators. Efficacy and safety of regorafenib for advanced gastrointestinal stromal tumours after failure of imatinib and sunitinib (GRID): an international, multicentre, randomised, placebo-controlled, phase 3 trial. Lancet. 2013;381(9863):295–302. | ||
Abdel-Rahman O, Fouad M. Risk of mucocutaneous toxicities in patients with solid tumors treated with sunitinib: a critical review and meta analysis. Expert Rev Anticancer Ther. 2015;15(1):129–141. | ||
Fischer A, Wu S, Ho AL, Lacouture ME. The risk of hand-foot skin reaction to axitinib, a novel VEGF inhibitor: a systematic review of literature and meta-analysis. Invest New Drugs. 2013;31(3):787–797. | ||
Elting LS, Chang YC, Parelkar P, et al; Mucositis Study Group of the Multinational Association of Supportive Care in Cancer/International Society of Oral Oncology (MASCC/ISOO). Risk of oral and gastrointestinal mucosal injury among patients receiving selected targeted agents: a meta-analysis. Support Care Cancer. 2013;21(11):3243–3254. | ||
Balagula Y, Wu S, Su X, Feldman DR, Lacouture ME. The risk of hand foot skin reaction to pazopanib, a novel multikinase inhibitor: a systematic review of literature and meta-analysis. Invest New Drugs. 2012;30(4):1773–1781. | ||
Iacovelli R, Palazzo A, Procopio G, et al. Incidence and relative risk of hepatic toxicity in patients treated with antiangiogenic tyrosine kinase inhibitors for malignancy. Br J Clin Pharmacol. 2013;77(6):929–938. | ||
Ghatalia P, Je Y, Mouallem NE, et al. Hepatotoxicity with vascular endothelial growth factor receptor tyrosine kinase inhibitors: a meta-analysis of randomized clinical trials. Crit Rev Oncol Hematol. 2014;93(3):257–276. | ||
Teo YL, Ho HK, Chan A. Risk of tyrosine kinase inhibitors-induced hepatotoxicity in cancer patients: a meta-analysis. Cancer Treat Rev. 2013;39(2):199–206. | ||
Kapadia S, Hapani S, Choueiri TK, Wu S. Risk of liver toxicity with the angiogenesis inhibitor pazopanib in cancer patients. Acta Oncol. 2013;52(6):1202–1212. | ||
Qi WX, Sun YJ, Tang LN, Shen Z, Yao Y. Risk of gastrointestinal perforation in cancer patients treated with vascular endothelial growth factor receptor tyrosine kinase inhibitors: a systematic review and meta-analysis. Crit Rev Oncol Hematol. 2014;89(3):394–403. | ||
Qi WX, Shen F, Qing Z, Xiao-Mao G. Risk of gastrointestinal perforation in cancer patients treated with aflibercept: a systematic review and meta-analysis. Tumour Biol. 2014;35(11):10715–10722. | ||
Ghatalia P, Morgan CJ, Je Y, et al. Congestive heart failure with vascular endothelial growth factor receptor tyrosine kinase inhibitors. Crit Rev Oncol Hematol. 2014;94(2):228–237. | ||
Ghatalia P, Je Y, Kaymakcalan MD, Sonpavde G, Choueiri TK. QTc interval prolongation with vascular endothelial growth factor receptor tyrosine kinase inhibitors. Br J Cancer. 2014;112(2):296–305. | ||
Abdel-Rahman O, Fouad M. Risk of cardiovascular toxicities in patients with solid tumors treated with sorafenib: an updated systematic review and meta-analysis. Future Oncol. 2014;10(12):1981–1992. | ||
Abdel-Rahman O, Fouad M. Risk of cardiovascular toxicities in patients with solid tumors treated with sunitinib, axitinib, cediranib or regorafenib: an updated systematic review and comparative meta-analysis. Crit Rev Oncol Hematol. 2014;92(3):194–207. | ||
Qi WX, Shen Z, Tang LN, Yao Y. Risk of arterial thromboembolic events with vascular endothelial growth factor receptor tyrosine kinase inhibitors: an up-to-date meta-analysis. Crit Rev Oncol Hematol. 2014;92(2): 71–82. | ||
Qi WX, Shen Z, Tang LN, Yao Y. Congestive heart failure risk in cancer patients treated with vascular endothelial growth factor tyrosine kinase inhibitors: a systematic review and meta-analysis of 36 clinical trials. Br J Clin Pharmacol. 2014;78(4):748–762. | ||
Qi WX, Shen Z, Lin F, et al. Incidence and risk of hypertension with vandetanib in cancer patients: a systematic review and meta-analysis of clinical trials. Br J Clin Pharmacol. 2013;75(4):919–930. | ||
Qi WX, Min DL, Shen Z, et al. Risk of venous thromboembolic events associated with VEGFR-TKIs: a systematic review and meta-analysis. Int J Cancer. 2013;132(12):2967–2974. | ||
Jadad AR, Moore RA, Carroll D, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17(1):1–12. | ||
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol. 2009;62(10):1006–1012. | ||
Choueiri TK, Schutz FA, Je Y, Rosenberg JE, Bellmunt J. Risk of arterial thromboembolic events with sunitinib and sorafenib: a systematic review and meta-analysis of clinical trials. J Clin Oncol. 2010;28(13):2280–2285. | ||
Zintzaras E, Ioannidis JP. Heterogeneity testing in meta-analysis of genome searches. Genet Epidemiol. 2005;28(2):123–137. | ||
Reck M, Kaiser R, Mellemgaard A, et al; LUME-Lung 1 Study Group. Docetaxel plus nintedanib versus docetaxel plus placebo in patients with previously treated non-small-cell lung cancer (LUME-Lung 1): a phase 3, double-blind, randomised controlled trial. Lancet Oncol. 2014;15(2):143–155. | ||
Laurie SA, Solomon BJ, Seymour L, et al. Randomised, double-blind trial of carboplatin and paclitaxel with daily oral cediranib or placebo in patients with advanced non-small cell lung cancer: NCIC Clinical Trials Group study BR29. Eur J Cancer. 2014;50(4):706–712. | ||
Garon EB, Ciuleanu TE, Arrieta O, et al. Ramucirumab plus docetaxel versus placebo plus docetaxel for second-line treatment of stage IV non-small-cell lung cancer after disease progression on platinum-based therapy (REVEL): a multicentre, double-blind, randomised phase 3 trial. Lancet. 2014;384(9944):665–673. | ||
Scagliotti GV, Vynnychenko I, Park K, et al. International, randomized, placebo-controlled, double-blind phase III study of motesanib plus carboplatin/paclitaxel in patients with advanced nonsquamous non-small-cell lung cancer: MONET1. J Clin Oncol. 2012;30(23):2829–2836. | ||
Scagliotti GV, Krzakowski M, Szczesna A, et al. Sunitinib plus erlotinib versus placebo plus erlotinib in patients with previously treated advanced non-small-cell lung cancer: a phase III trial. J Clin Oncol. 2012;30(17):2070–2078. | ||
Lee JS, Hirsh V, Park K, et al. Vandetanib versus placebo in patients with advanced non-small-cell lung cancer after prior therapy with an epidermal growth factor receptor tyrosine kinase inhibitor: a randomized, double-blind phase III trial (ZEPHYR). J Clin Oncol. 2012;30(10):1114–1121. | ||
Natale RB, Thongprasert S, Greco FA, et al. Phase III trial of vandetanib compared with erlotinib in patients with previously treated advanced non-small-cell lung cancer. J Clin Oncol. 2011;29(8):1059–1066. | ||
Scagliotti G, Novello S, von Pawel J, et al. Phase III study of carboplatin and paclitaxel alone or with sorafenib in advanced non-small-cell lung cancer. J Clin Oncol. 2010;28(11):1835–1842. | ||
Herbst RS, Sun Y, Eberhardt WE, et al. Vandetanib plus docetaxel versus docetaxel as second-line treatment for patients with advanced non-small-cell lung cancer (ZODIAC): a double-blind, randomised, phase 3 trial. Lancet Oncol. 2010;11(7):619–626. | ||
Natale RB, Bodkin D, Govindan R, et al. Vandetanib versus gefitinib in patients with advanced non-small-cell lung cancer: results from a two-part, double-blind, randomized phase ii study. J Clin Oncol. 2009;27(15):2523–2529. | ||
Carrato A, Swieboda-Sadlej A, Staszewska-Skurczynska M, et al. Fluorouracil, leucovorin, and irinotecan plus either sunitinib or placebo in metastatic colorectal cancer: a randomized, phase III trial. J Clin Oncol. 2013;31(10):1341–1347. | ||
Hoff PM, Hochhaus A, Pestalozzi BC, et al. Cediranib plus FOLFOX/CAPOX versus placebo plus FOLFOX/CAPOX in patients with previously untreated metastatic colorectal cancer: a randomized, double-blind, phase III study (HORIZON II). J Clin Oncol. 2012;30(29):3596–3603. | ||
Brose MS, Nutting CM, Jarzab B, et al. Sorafenib in radioactive iodine-refractory, locally advanced or metastatic differentiated thyroid cancer: a randomised, double-blind, phase 3 trial. Lancet. 2014;384(9940):319–328. | ||
Wells SA Jr, Robinson BG, Gagel RF, et al. Vandetanib in patients with locally advanced or metastatic medullary thyroid cancer: a randomized, double-blind phase III trial. J Clin Oncol. 2012;30(2):134–141. | ||
Leboulleux S, Bastholt L, Krause T, et al. Vandetanib in locally advanced or metastatic differentiated thyroid cancer: a randomised, double-blind, phase 2 trial. Lancet Oncol. 2012;13(9):897–905. | ||
Kudo M, Han G, Finn RS, et al. Brivanib as adjuvant therapy to transarterial chemoembolization in patients with hepatocellular carcinoma: a randomized phase 3 trial. Hepatology. 2014;60(5):1697–1707. | ||
Abou-Alfa GK, Johnson P, Knox JJ, et al. Doxorubicin plus sorafenib vs doxorubicin alone in patients with advanced hepatocellular carcinoma: a randomized trial. JAMA. 2010;304(19):2154–2160. | ||
Barrios CH, Liu MC, Lee SC, et al. Phase III randomized trial of sunitinib versus capecitabine in patients with previously treated HER2-negative advanced breast cancer. Breast Cancer Res Treat. 2010;121(1):121–131. | ||
Choueiri TK, Ross RW, Jacobus S, et al. Double-blind, randomized trial of docetaxel plus vandetanib versus docetaxel plus placebo in platinum-pretreated metastatic urothelial cancer. J Clin Oncol. 2012;30(5):507–512. | ||
Goncalves A, Gilabert M, Francois E, et al. BAYPAN study: a double-blind phase III randomized trial comparing gemcitabine plus sorafenib and gemcitabine plus placebo in patients with advanced pancreatic cancer. Ann Oncol. 2012;23(11):2799–2805. | ||
Yi JH, Lee J, Park SH, et al. Randomised phase II trial of docetaxel and sunitinib in patients with metastatic gastric cancer who were previously treated with fluoropyrimidine and platinum. Br J Cancer. 2012;106(9):1469–1474. | ||
Flaherty KT, Lee SJ, Zhao F, et al. Phase III trial of carboplatin and paclitaxel with or without sorafenib in metastatic melanoma. J Clin Oncol. 2013;31(3):373–379. | ||
Hutson TE, Escudier B, Esteban E, et al. Randomized phase III trial of temsirolimus versus sorafenib as second-line therapy after sunitinib in patients with metastatic renal cell carcinoma. J Clin Oncol. 2014;32(8):760–767. | ||
Serve H, Krug U, Wagner R, et al. Sorafenib in combination with intensive chemotherapy in elderly patients with acute myeloid leukemia: results from a randomized, placebo-controlled trial. J Clin Oncol. 2013;31(25):3110–3118. | ||
Michaelson MD, Oudard S, Ou YC, et al. Randomized, placebo-controlled, phase III trial of sunitinib plus prednisone versus prednisone alone in progressive, metastatic, castration-resistant prostate cancer. J Clin Oncol. 2014;32(2):76–82. |
Supplementary materials
Search strategy for meta-analysis of association between use of vascular endothelial growth factor receptor tyrosine kinase inhibitors (VEGFR-TKIs) and the risk of severe infections in cancer patients
PubMed
- VEGFR-TKIs [ALL]
- “VEGFR-tyrosine kinase inhibitors” [ALL]
- “VEGFR-tyrosine kinase inhibitor” [ALL]
- “vascular endothelial growth factor receptor tyrosine kinase inhibitor” [ALL]
- “vascular endothelial growth factor receptor tyrosine kinase inhibitors” [ALL]
- 1 or 2 or 3 or 4 or 5
- “nexavar” [NM] OR “BAY43-9006” [NM] OR “sorafenib” [ALL]
- “sutent” [NM] OR “SU11248” [NM] OR “sunitinib” [ALL]
- “votrient” [NM] OR“GW786034” [NM] OR “vandetanib” [ALL]
- “caprelsa” [NM] OR “ZD6474” [NM] OR “axitinib” [ALL]
- “AG-013736” [MH] OR “cediranib” [ALL]
- “AZD2171” [NM] OR “tivozanib” [ALL]
- “BAY73-4506” [MH] OR “regorafenib” [ALL]
- “cabozantinib” [ALL]
- “brivanib” [ALL]
- “ramucirumab” [ALL]
- “IMC-1121B” [NM] OR “nintedanib” [ALL]
- “BIBF1120” [MH] OR “motesanib” [ALL]
- 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18
- “neoplasms” [MH] OR “neoplasms” [ALL] OR “cancer” [ALL]
- “neoplasm” [ALL]
- “neoplasia” [ALL]
- “malignancy” [ALL]
- Malignant [ALL]
- “carcinoma” [MH] OR “carcinoma” [ALL]
- “glioma” [MH] OR “glioma” [ALL]
- “leukaemia” [ALL] OR “leukemia” [MH] OR “leukemia” [ALL]
- “lymphoma” [MH] OR “lymphoma” [ALL]
- “melanoma” [MH] OR “melanoma” [ALL]
- “meningioma” [MH] OR “meningioma” [ALL]
- “sarcoma” [MH] OR “sarcoma” [ALL]
- 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 or 31
- 19 and 32
- “humans” [MH]
- 33 and 34
ALL = all fields, MH = MeSH Terms, NM = substance name
Limitation: humans
Date of Search: December 2014 (1974–December 2014)
EMBASE
- VEGFR-TKIs
- “VEGFR- tyrosine kinase inhibitors”
- “VEGFR- tyrosine kinase inhibitor”/de
- “vascular endothelial growth factor receptor tyrosine kinase inhibitor”/de
- “vascular endothelial growth factor receptor tyrosine kinase inhibitors”/de
- 1 or 2 or 3 or 4 or 5
- “sunitinib”/de
- “sorafenib”/de
- “pazopanib”/de
- “vandetanib”/de
- “axitinib”/de
- “cediranib”/de
- “tivozanib”/de
- “regorafenib”/de
- “cabozantinib”/de
- “nintedanib”/de
- “brivanib”/de
- “ramucirumab”/de
- “motesanib”/de
- 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19
- “cancer”/de
- “neoplasm”/de
- “neoplasia”/de
- malignancy
- malignant
- “carcinoma”/de
- “glioma”/de
- “leukemia”/de
- “lymphoma”/de
- “melanoma”/de
- “meningioma”/de
- “sarcoma”/de
- 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 or 31 or 32
- [humans]/lim
- [embase]/lim OR [embase classic]/lim
- 20 and 34 and 35
/de = Mapped terms, /lim = Limitation
Limitation: humans
Date of Search: December 2014 (1979–December 2014)
CENTRAL database (The Cochrane Library)
- VEGFR-TKIs [ALL]
- “VEGFR-tyrosine kinase inhibitors” [ALL]
- “VEGFR-tyrosine kinase inhibitor” [ALL]
- 4 “vascular endothelial growth factor receptor tyrosine kinase inhibitor” [ALL]
- “vascular endothelial growth factor receptor tyrosine kinase inhibitors” [ALL]
- 1 or 2 or 3 or 4 or 5
- “sunitinib”/de
- “sorafenib”/de
- “pazopanib”/de
- “vandetanib”/de
- “axitinib”/de
- “cediranib”/de
- “tivozanib”/de
- “regorafenib”/de
- “cabozantinib”/de
- “nintedanib”/de
- “brivanib”/de
- “ramucirumab”/de
- “motesanib”/de
- 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19
- “cancer”/de
- “neoplasm”/de
- “neoplasia”/de
- malignancy
- malignant
- “carcinoma”/de
- “glioma”/de
- “leukemia”/de
- “lymphoma”/de
- “melanoma”/de
- “meningioma”/de
- “sarcoma”/de
- 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 or 31 or 32
- 20 and 33
[ALL] = in All Text
Limitation: none
Date of Search: December 2014 (1979–December 2014)
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.