Back to Journals » Clinical Ophthalmology » Volume 9
Incidence of bleb-associated endophthalmitis in the United States
Authors Vaziri K, Kishor K, Schwartz S , Maharaj AS, Moshfeghi D, Moshfeghi A, Flynn Jr. H
Received 2 October 2014
Accepted for publication 30 October 2014
Published 12 February 2015 Volume 2015:9 Pages 317—322
DOI https://doi.org/10.2147/OPTH.S75286
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Kamyar Vaziri,1 Krishna Kishor,1 Stephen G Schwartz,1 Arindel S Maharaj,1 Darius M Moshfeghi,2 Andrew A Moshfeghi,3 Harry W Flynn Jr1
1Department of Ophthalmology, Bascom Palmer Eye Institute, University of Miami, Miller School of Medicine, Miami, FL, USA; 2Department of Ophthalmology, Byers Eye Institute, Stanford University School of Medicine, Palo Alto, CA, USA; 3USC Eye Institute, Department of Ophthalmology, University of Southern California Keck School of Medicine, Los Angeles, CA, USA
Purpose: To evaluate the 5-year incidence rate of blebitis and bleb-associated endophthalmitis in the United States.
Methods: In this retrospective cross-sectional study, we utilized a large commercial health insurance claim-based database during 2007–2011 and identified all patients who had a record of trabeculectomy in 2007. These patients were followed until the end of 2011. During the follow-up period, all incidences of blebitis, confirmed bleb-associated endophthalmitis, and presumed bleb-associated endophthalmitis were recorded. Kaplan–Meier survival analysis was utilized to calculate 5-year cumulative incidence rates of blebitis and bleb-associated endophthalmitis following trabeculectomy procedures.
Results: Among the 1,461 trabeculectomies included in our analysis, eight cases of blebitis, five cases of confirmed bleb-associated endophthalmitis, and eight cases of presumed bleb-associated endophthalmitis were identified. We found that the 5-year cumulative incidence of blebitis was 0.55%±0.19%. The 5-year cumulative incidence of bleb-associated endophthalmitis was 0.45%±0.2% when only confirmed cases were included and 1.3%±0.34% when presumed cases were also added to the analysis. The mean time from procedure to diagnosis was 45 months for blebitis and 33 months for bleb-associated endophthalmitis.
Conclusion: Blebitis and bleb-related endophthalmitis are uncommon in the United States. The 5-year cumulative incidence was 0.55% for blebitis and 0.45%–1.3% for bleb-associated endophthalmitis.
Keywords: bleb, blebitis, bleb-associated endophthalmitis, trabeculectomy
Introduction
Bleb-related infections are potentially sight-threatening complications of trabeculectomy. These infections can be divided into two categories: blebitis and bleb-associated endophthalmitis. Blebitis refers to an infection limited to the bleb, with varying degrees of anterior chamber inflammation. When this infection moves beyond the anterior chamber and involves the vitreous, it is referred to as bleb-associated endophthalmitis.
Among bleb-related infections, endophthalmitis carries the highest risk of morbidity and is associated with poor visual outcomes. One study reported that 36%–62% of patients with bleb-associated endophthalmitis had a final visual acuity of worse than 5/200, even after treatment,1 and other studies have reported that the incidence of no light perception ranged from 23% to 35%.2,3 Several risk factors have been associated with bleb-associated endophthalmitis, including bleb leakage, use of antimetabolites, inferior trabeculectomy, thin avascular bleb, axial myopia, blepharitis, chronic antibiotic use, and younger age.4–9 While bleb-related endophthalmitis can occur acutely (<4 weeks), most cases are delayed onset (>4 weeks), with a reported average onset of 5 years after trabulectomy.10 One study reported endophthalmitis 42 years after glaucoma filtration surgery.11
Numerous series have reported the incidence of bleb-associated endophthalmitis at between 0.17% and 13.2%.8,12–26 However, many of these reports were single center, potentially creating a bias with regard to location-specific surgical techniques, geographic variability of microorganisms, and patient demographics. In addition, with the exception of a small minority of the studies,15,24–26 most used relatively smaller sample sizes (<600 trabeculectomies), possibly affecting the validity of the statistical analysis. In addition, the use of adjuvant antimetabolites (ie, mitomycin C and 5-fluorouracil) may have led to increased rates of endophthalmitis.14,24,25 At the same time, surgical techniques and surgeon confidence in using intraoperative antimetabolites may have improved in recent years, and this warrants a re-evaluation of the incidence rates using a large sample size and adequate follow-up time. In this study, we aimed to utilize a large nationally pooled insurance claim-based database to calculate the cumulative incidence of bleb-associated endophthalmitis following trabeculectomy procedures and to characterize these patients.
Methods
Data source
The current study is a retrospective cross-sectional case series utilizing the MarketScan Commercial Claims and Encounters database and the MarketScan Medicare Supplemental and Coordination of Benefits outpatient services and inpatient databases (Truven Health Analytics, Ann Arbor, MI, USA) from 2007 to 2011 (the most recent year the databases were available to us). The MarketScan family of databases comprises the largest convenience-based proprietary database in the US, annually encompassing approximately 40–50 million patients with employer-sponsored or supplemental insurance. These databases consist of de-identified, individual-level health records (inpatient and outpatient) obtained from large employers, hospitals, and Medicare programs. The MarketScan database contains de-identified and anonymized records and complies with the privacy requirements of the Health Information Portability and Accountability Act of 1996 (HIPAA), so Institutional Review Board (IRB) approval was not required.
The MarketScan outpatient services databases include demographic, provider type, and insurance information along with up to four diagnosis codes and one procedure code per recorded insurance claim (coded using the International Classification of Disease [ICD-9] and Current Procedural Terminology [CPT], respectively). Again, the databases are fully de-identified and thus HIPAA compliant and exempt from IRB approval. Detailed information regarding the structure, de-identification of patient records, and HIPAA compliance of MarketScan databases can be found elsewhere.27
Study sample and statistical analysis
The overall objective of this study was to identify patients who had a record of glaucoma filtering surgery in 2007 and follow their medical records until the end of 2011. We utilized CPT codes to select all the patients with such a history of trabeculectomy (CPT codes 66170 and 66172) in the year 2007. As the MarketScan databases are insurance claim based, they provide medical records for only the period of time during which the patients had active insurance coverage. As such, to be able to capture complete and uninterrupted medical records of patients during our study’s follow-up period, only patients with continuous medical insurance coverage from the date of their trabeculectomy to the end of 2011 were included.
All recorded medical diagnoses of these patients including blebitis (ICD-9 397.61 and 379.62) and bleb-associated endophthalmitis (ICD-9 code 379.63) were identified throughout the follow-up period. For the purposes of this study, we considered any patient with diagnosis code 379.63 to be a “confirmed” case of bleb-associated endophthalmitis. We also selected patients with ICD-9 diagnosis codes of 360.00 (“purulent endophthalmitis, unspecified”), 360.01 (“acute endophthalmitis”), and 360.02 (“panophthalmitis”) who did not have records of additional ophthalmic surgery, ophthalmic trauma, or history of intravitreal injection within 2 months prior to their endophthalmitis diagnosis. We hypothesized that these patients also represented cases of bleb-associated endophthalmitis that were incorrectly coded by their treating physicians, and for the purposes of this study, we considered these patients to be “presumed” cases of bleb-associated endophthalmitis.
Bleb revision procedures were identified by combined coding of CPT 66250 (“revision or repair of operative wound of anterior segment, any type, early or late, major or minor procedure”) along with any of the primary open-angle glaucoma ICD-9 diagnosis codes (365.10–365.15). Additional ICD-9 and CPT codes were queried to identify patients’ comorbidities and procedures of interest.
We used descriptive statistics and cross-tabulations to evaluate prevalence estimates of comorbidities and demographic information. Kaplan–Meier survival analysis was utilized to calculate cumulative incidence of bleb-associated endophthalmitis following trabeculectomy procedures. All statistical analyses were performed with SPSS (Version 22, SPSS Inc, Chicago, IL, USA).
Results
After excluding patients with noncontinuous insurance coverage during the follow-up period, utilizing CPT, 1,461 glaucoma filtering surgeries were included in this analysis. The age of included patients in this analysis ranged from infancy (<1 year old) to 95 years old with a mean of 68.9±12.8 years of age. There were 685 males (46.9%) and 776 females (53.1%).
Among the 1,461 glaucoma filtering surgeries analyzed, 67.8% had CPT code 66170 (“trabeculectomy ab externo in absence of previous surgery”) and the remaining 32.2% had CPT code 66172 (“trabeculectomy ab externo with scarring from previous ocular surgery or trauma – includes injection of antifibrotic agents”). The medical records of individuals were followed from the date of their glaucoma filtering surgeries in 2007 to the end of 2011, which yielded a mean follow-up time of 53.8±3.4 months (4.5 years).
In the database, five recorded cases of confirmed bleb-associated endophthalmitis (ICD-9 code 379.63), eleven cases of presumed bleb-associated endophthalmitis, and eight cases of blebitis were identified. Three of the endophthalmitis cases had CPT code 66170, and the remaining two had a recorded CPT code of 66172. Utilizing only the confirmed cases of endophthalmitis, Kaplan–Meier analysis showed that the cumulative incidence of developing bleb-associated endophthalmitis was 0.45%±0.2% at the maximum 5-year follow-up. The mean time to diagnosis of endophthalmitis following trabeculectomy was 44.6 months (or 3.7 years) and ranged from 23 months to 55 months.
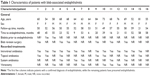
In a separate analysis, eleven cases of presumed bleb-associated endophthalmitis were identified that were potentially miscoded as other categories of endophthalmitis for a total of 16 endophthalmitis cases. In this scenario, the 5-year cumulative incidence of presumed bleb-associated endophthalmitis was 1.3%±0.34%, and the mean time to diagnosis of endophthalmitis following trabeculectomy was 32.8 months (2.7 years), ranging from 6 months to 55 months (Table 1). Among all 16 cases of confirmed and presumed bleb-associated endophthalmitis, two (12.5%) had a record of prior blebitis and six (37.5%) had a record of bleb revision surgery. In patients with bleb-associated endophthalmitis, vitreous tap and intravitreal injection of antibiotics were used in 14 (87.5%) cases and pars plana vitrectomy was utilized in five cases (31%). Two bleb-associated endophthalmitis cases had no treatment records in the database (Table 1).
Additionally, 5-year cumulative incidence of blebitis was 0.5%5±0.19% with mean time to diagnosis of 45 months, ranging from 2 months to 47 months.
Discussion
Bleb-associated endophthalmitis is a serious complication of trabeculectomy. Prompt recognition and treatment of bleb-related infections are important for best possible clinical outcomes. Signs and symptoms of bleb-associated endophthalmitis are similar to other forms of endophthalmitis and most commonly include eye pain and decreased vision.28 The presence of anterior chamber hypopyon and inflammatory cells in the vitreous are helpful in differentiating blebitis from endophthalmitis. Streptococcal species are the main causative agents for bleb-associated endophthalmitis in the US,2,10,11,28 while staphylococcal species are the predominant pathogens in East Asia,3,24 demonstrating a potential geographical variation.
To date, there have been no established and official guidelines for the treatment of bleb-related infections. The Endophthalmitis Vitrectomy Study29 did not recruit this cohort of patients, so its results do not directly apply to the management of these patients. Treatment regimens range from topical antibiotics for isolated blebitis to tap and inject or pars plana vitrectomy, depending on the severity of the infection. Furthermore, even with appropriate treatments, the final visual outcomes tend to be poor. A recent study found that close to half of the patients with bleb-associated endophthalmitis had final visual acuity of worse than 20/400, despite receiving the indicated medical or surgical therapies.1 As a result, it is important to re-evaluate the incidence of bleb-related endophthalmitis using a large sample size and adequate follow-up time.
Previous studies have reported a wide range of cumulative incidence rates for the development of bleb-associated endophthalmitis. This variability in reported incidence rates may be due to differences in surgical techniques, sample sizes used in analyses, and the duration of follow-up times. As many of these studies worked with relatively small sample sizes and limited average follow-up times, we aimed to investigate bleb-associated incidence rates utilizing a large proprietary database that allowed us to follow patients’ medical records for up to 5 years. To our knowledge, this was the first time that a large commercial database containing data from all 50 states was used to evaluate these incidence rates. We found that the cumulative incidence rate of bleb-associated endophthalmitis ranged between 0.45% and 1.3% at the maximum of a 5-year follow-up mark. These incidence rates fall within the spectrum of previously reported rates.
While our analysis included all cases of trabeculectomy with or without adjuvant chemotherapy, most of the prior studies that reported higher incidence rates focused solely on trabeculectomies that were accompanied by adjuvant mitomycin C or 5-fluorouracil injections.13,14,17,19,21–23,26 This may partly explain the higher incidence rates reported by those publications. While adjuvant antimetabolites such as mitomycin C and 5-fluorouracil have greatly increased the success rates of filtration surgeries, their use results in formation of thin and avascular blebs, potentially leading to easier migration of pathogens across the bleb and leading to higher rates of bleb-associated endophthalmitis.14,24,25 As the intraoperative use of these adjuvant antifibrotics is not coded separately and is included with the trabeculectomy procedural codes, we were unable to calculate the proportion of trabeculectomies in our sample size accompanied by adjuvant therapy.
Despite the higher rates of bleb-related infections in the first decade following the introduction of intraoperative antimetabolite use, these rates have declined significantly in more recent years,30 which may also partly explain why our cumulative incidence rate utilizing a more recent data sample was lower than those of older publications. The drop in the incidence rate of bleb-related infections has been attributed to many factors, including increased surgeon confidence in using intraoperative mitomycin C, a shift toward limbus-based from fornix-based procedures, and use of a larger area for mitomycin C application.30 Both fornix-based conjuctival flaps and a larger area for mitomycin C application may lead to less frequent formation of cystic blebs, an important risk factor for blebitis and bleb-associated endophthalmitis.31,32
The current study has several strengths and limitations. For our analysis, this study utilized a large database that includes patients from all 50 states of the United States, which reduced the dependence of our results on location-specific variables (ie, patient demographics or preferred surgical techniques). In addition, the database allowed us to detect all patients’ comorbities and any new diagnoses (regardless of the specialty) throughout the follow-up period.
The major limitation of this study is the fact that there is no way to confirm the diagnosis of these cases. The MarketScan databases are insurance claim-based, and the medical diagnoses and surgical procedures are recorded as ICD-9 and CPT codes, respectively, so the accuracy of the data necessarily depends upon proper coding by the treating physicians. We assumed that any case coded with diagnosis 379.63 was a definite case of bleb-associated endophthalmitis, so we considered these “confirmed” cases. In addition, we assumed that any case coded with diagnoses 360.00, 360.01, or 360.02 was likely a miscoded case of bleb-associated endophthalmitis, so we considered these “presumed” cases. Because the databases are fully de-identified, there is no way to confirm the accuracy of these assumptions, and our data should be evaluated with this in mind. Furthermore, the current study is unable to evaluate clinical findings or morbidities that do not have specific diagnosis codes associated with them, such as bleb leaks, or identify the causative pathogens in individuals with bleb-associated endophthalmitis.
Conclusion
In conclusion, the cumulative incidence of blebitis was 0.55%, and the cumulative incidence of bleb-associated endophthalmitis was between 0.45% and 1.3% after up to 5 years of follow-up. To our knowledge, this is the first time that a large commercial claims database was utilized to calculate these incidence rates. While it has been proposed than an increase in use of adjuvant antimetabolites would lead to an increase in overall incidence of bleb-associated endophthalmitis, the calculated rate was at the lower end of the spectrum of numbers reported by previous publications. This may have been partly due to improved surgical techniques over recent years.
Acknowledgments
Access to the MarketScan databases was made possible by a grant from the Celia Lipton and Victor W Farris Foundation, Inc, West Palm Beach, FL, USA. In addition, this project was partially supported by NIH Center Core Grant P30EY014801 and an unrestricted grant from Research to Prevent Blindness, New York, NY, USA.
Disclosure
The authors report no conflicts of interest in this work.
References
Leng T, Miller D, Flynn HW Jr, Jacobs DJ, Gedde SJ. Delayed-onset bleb-associated endophthalmitis (1996–2008): causative organisms and visual acuity outcomes. Retina. 2011;31(2):344–352. | ||
Busbee BG, Recchia FM, Kaiser R, et al. Bleb-associated endophthalmitis: clinical characteristics and visual outcomes. Ophthalmology. 2004;111(8):1495–1503. | ||
Ye H, Sun X, Gan D, et al. Bleb-associated endophthalmitis in a Chinese population (2003–2010): clinical characteristics and visual outcome. Eur J Ophthalmol. 2012;22(5):719–725. | ||
Hori N, Mochizuki K, Ishida K, Yamamoto T, Mikamo H. Clinical characteristics and risk factors of glaucoma filtering bleb infections. Nihon Ganka Gakkai Zasshi. 2009;113(10):951–963. | ||
Soltau JB, Rothman RF, Budenz DL, et al. Risk factors for glaucoma filtering bleb infections. Arch Ophthalmol. 2000;118(3):338–342. | ||
Jampel HD, Quigley HA, Kerrigan-Baumrind LA, Melia BM, Friedman D, Barron Y. Risk factors for late-onset infection following glaucoma filtration surgery. Arch Ophthalmol. 2001;119(7):1001–1008. | ||
Ashkenazi I, Melamed S, Avni I, Bartov E, Blumenthal M. Risk factors associated with late infection of filtering blebs and endophthalmitis. Ophthalmic Surg. 1991;22(10):570–574. | ||
Sharan S, Trope GE, Chipman M, Buys YM. Late-onset bleb infections: prevalence and risk factors. Can J Ophthalmol. 2009;44(3):279–283. | ||
Poulsen EJ, Allingham RR. Characteristics and risk factors of infections after glaucoma filtering surgery. J Glaucoma. 2000;9(6):438–443. | ||
Song A, Scott IU, Flynn HW Jr, Budenz DL. Delayed-onset bleb-associated endophthalmitis: Clinical features and visual acuity outcomes. Ophthalmology. 2002;109:985–991. | ||
Ciulla TA, Beck AD, Topping TM, Baker AS. Blebitis, early endophthalmitis, and late endophthalmitis after glaucoma-filtering surgery. Ophthalmology. 1997;104(6):986–995. | ||
Alwitry A, King AJ. Surveillance of late-onset bleb leak, blebitis and bleb-related endophthalmitis: a UK incidence study. Graefe’s Arch Clin Exp Ophthalmol. 2012;250(8):1231–1236. | ||
DeBry PW, Perkins TW, Heatley G, Kaufman P, Brumback LC. Incidence of late-onset bleb-related complications following trabeculectomy with mitomycin. Arch Ophthalmol. 2002;120(3):297–300. | ||
Greenfield DS, Suñer IJ, Miller MP, Kangas TA, Palmberg PF, Flynn HW Jr. Endophthalmitis after filtering surgery with mitomycin. Arch Ophthalmol. 1996;114(8):943–949. | ||
Katz LJ, Cantor LB, Spaeth GL. Complications of surgery in glaucoma. early and late bacterial endophthalmitis following glaucoma filtering surgery. Ophthalmology. 1985;92(7):959–963. | ||
Freedman J, Gupta M, Bunke A. Endophthalmitis after trabeculectomy. Arch Ophthalmol. 1978;96(6):1017–1018. | ||
Higginbotham EJ, Stevens RK, Musch DC, et al. Bleb-related endophthalmitis after trabeculectomy with mitomycin C. Ophthalmology. 1996;103(4):650–656. | ||
Wolner B, Liebmann JM, Sassani JW, Ritch R, Speaker M, Marmor M. Late bleb-related endophthalmitis after trabeculectomy with adjunctive 5-fluorouracil. Ophthalmology. 1991;98(7):1053–1060. | ||
Ticho U, Ophir A. Late complications after glaucoma filtering surgery with adjunctive 5-fluorouracil. Am J Ophthalmol. 1993;115(4):506–510. | ||
Solomon A, Ticho U, Frucht-Pery J. Late-onset, bleb-associated endophthalmitis following glaucoma filtering surgery with or without antifibrotic agents. J Ocul Pharmacol Ther. 1999;15(4):283–293. | ||
Mochizuki K, Jikihara S, Ando Y, Hori N, Yamamoto T, Kitazawa Y. Late infection after trabeculectomy with adjunctive mitomycin C and 5-fluorouracil. Investig Ophthalmol Vis Sci. 1996;81(10):877–883. | ||
Mégevand GS, Salmon JF, Scholtz RP, Murray AD. The effect of reducing the exposure time of mitomycin C in glaucoma filtering surgery. Ophthalmology. 1995;102(1):84–90. | ||
Muckley ED, Lehrer RA. Late-onset blebitis/endophthalmitis: incidence and outcomes with mitomycin C. Optom Vis Sci. 2004;81(7):499–504. | ||
Kuang TM, Lin YC, Jui-Ling Liu C, Hsu WM, Chou CK. Early and late endophthalmitis following trabeculectomy in a Chinese population. Eur J Ophthalmol. 2008;18(1):66–70. | ||
Wallin Ö, Al-Ahramy AM, Lundström M, Montan P. Endophthalmitis and severe blebitis following trabeculectomy. Epidemiology and risk factors; A single-centre retrospective study. Acta Ophthalmol. 2014;92(5):426–431. | ||
Yamamoto T, Sawada A, Mayama C, et al. The 5-year incidence of bleb-related infection and its risk factors after filtering surgeries with adjunctive mitomycin C: collaborative bleb-related infection incidence and treatment study 2. Ophthalmology. 2014;121(5):1001–1006. | ||
Danielson E. Health Research Data for the Real World: The MarketScan® Databases. 2014. Available from: http://truvenhealth.com/Portals/0/Users/031/31/31/PH_13434%200314_MarketScan_WP_web.pdf. Accessed December 11, 2014. | ||
Ba’arah BT, Smiddy WE. Bleb-related endophthalmitis: clinical presentation, isolates, treatment and visual outcome of culture-proven cases. Middle East Afr J Ophthalmol. 2009;16(1):20–24. | ||
Endophthalmitis Vitrectomy Study Group. Results of the Endophthalmitis Vitrectomy Study: a randomized trial of immediate vitrectomy and of intravenous antibiotics for the treatment of postoperative bacterial endophthalmitis. Arch Ophthalmol. 1995;113(12):1479–1496. | ||
Rai P, Kotecha A, Kaltsos K, et al. Changing trends in the incidence of bleb-related infection in trabeculectomy. Br J Ophthalmol. 2012;96(7):971–975. | ||
el Sayyad F, el-Rashood A, Helal M, Hisham M, el-Maghraby A. Fornix-based versus limbal-based conjunctival flaps in initial trabeculectomy with postoperative 5-fluorouracil: four-year follow-up findings. J Glaucoma. 1999;8(2):124–128. | ||
Wells AP, Cordeiro MF, Bunce C, Khaw PT. Cystic bleb formation and related complications in limbus-versus fornix-based conjunctival flaps in pediatric and young adult trabeculectomy with mitomycin C. Ophthalmology. 2003;110(11):2192–2197. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.