Back to Journals » Journal of Multidisciplinary Healthcare » Volume 8
Impact of an educational intervention on provider knowledge, attitudes, and comfort level regarding counseling women ages 40–49 about breast cancer screening
Authors Bryan T, Estrada C, Castiglioni A, Snyder E
Received 5 January 2015
Accepted for publication 12 February 2015
Published 4 May 2015 Volume 2015:8 Pages 209—216
DOI https://doi.org/10.2147/JMDH.S80337
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Teresa J Bryan,1,2 Carlos A Estrada,1,2 Analia Castiglioni,3 Erin D Snyder1,2
1University of Alabama at Birmingham, Birmingham, AL, USA; 2Birmingham Veterans Administration Medical Center, Birmingham, AL, USA; 3University of Central Florida College of Medicine, Orlando, FL, USA
Background: Mammography screening for women under the age of 50 is controversial. Groups such as the US Preventive Services Task Force recommend counseling women 40–49 years of age about mammography risks and benefits in order to incorporate the individual patient's values in decisions regarding screening. We assessed the impact of a brief educational intervention on the knowledge and attitudes of clinicians regarding breast cancer screening.
Methods: The educational intervention included a review of the risks and benefits of screening, individual risk assessment, and counseling methods. Sessions were led by a physician expert in breast cancer screening. Participants were physicians and nurses in 13 US Department of Veterans Affairs primary care clinics in Alabama. Outcomes were as follows: 1) knowledge assessment of mammogram screening recommendations; 2) counseling practices on the risks and benefits of screening; and 3) comfort level with counseling about screening. Outcomes were assessed by survey before and after the intervention.
Results: After the intervention, significant changes in attitudes about breast cancer screening were seen. There was a decrease in the percentage of participants who reported that they would screen all women ages 40–49 years (82% before the intervention, 9% afterward). There was an increase in the percentage of participants who reported that they would wait until the patient was 50 years old before beginning to screen (12% before the intervention, 38% afterward). More participants (5% before, 53% after; P<0.001) said that they would discuss the patient's preferences. Attitudes favoring discussion of screening benefits increased, though not significantly, from 94% to 99% (P=0.076). Attitudes favoring discussion of screening risks increased from 34% to 90% (P<0.001). The comfort level with discussing benefits increased from a mean of 3.8 to a mean of 4.5 (P<0.001); the comfort level with discussing screening risks increased from 2.7 to 4.3 (P<0.001); and the comfort level with discussing cancer risks and screening preferences with patients increased from 3.2 to 4.3 (P<0.001). (The comfort levels measurements were assessed by using a Likert scale, for which 1= not comfortable and 5= very comfortable.)
Conclusion: Most clinicians in the US Department of Veterans Affairs ambulatory practices in Alabama reported that they routinely discuss mammography benefits but not potential harms with patients. An educational intervention detailing recommendations and counseling methods affected the knowledge and attitudes about breast cancer screening. Participants expressed greater likelihood of discussing screening options in the future.
Keywords: breast cancer screening, education, primary care, mammography, counseling
Introduction
Breast cancer is the second leading cause of terminal cancer among women in the United States,1 and it is the most frequent cause of death by cancer for women in less developed regions.2 Mammography is routinely utilized to screen women in order to reduce their risk of death from breast cancer. However, mammography screening is also associated with inherent risks, specifically harms related to false positive screening and overdiagnosis.3
Mammography screening programs appear to confer a mortality benefit; however, this benefit is age dependent.3–5 Out of 2,000 women ages 40–49 screened biannually for 10 years, one death would be avoided at a cost of $105,000 per life year saved. For women ages 50–59, four out of 2,000 would benefit with a cost of $21,000 per life year saved. This increases to six lives saved for women in their 60s at the same cost.5,6
Potential harms from mammography include pain from the screening procedure itself, radiation exposure, false positive results (which may lead to unnecessary procedures and psychological stress), and overdiagnosis of breast cancer.4 Overdiagnosis (disease that would have never been evident in the patient’s lifetime) is the reason for an estimated 15%–25% of cancers identified by screening. At this rate, 6–10 women out of every 2,500 screened are at risk for overdiagnosis.7 The risk of false positives and overdiagnosis is higher when younger women are screened and when screening is done annually. In a recent meta-analysis, Welch and Passow report that 510–690 out of 1,000 women in their 40s screened annually over a 10-year time period may have a false positive mammogram. They estimate the risk of overdiagnosis to be up to eleven per 1,000 women receiving yearly screening in this age group.3
The American Cancer Society,8 The American College of Radiology,9 The National Comprehensive Cancer Network,10 and The American College of Obstetrics and Gynecologists11 recommend mammogram screening beginning at age 40. However, since evidence suggests that younger women may have a lower benefit–risk ratio, other groups in the United States, Canada, and Europe recommend that women at average risk wait until age 50 to be screened.12–15 A recent update from the World Health Organization recommends that screening of women ages 40–49 be a shared decision based on the patient’s values and preferences.16 Likewise, the US Preventive Services Task Force (USPSTF) recommends that mammography screening of women in this age group take into consideration the “patient’s values regarding specific benefits and harms”.12
Mammography screening rates remain unchanged in recent years, a finding which suggests that practice patterns have not incorporated options to postpone screening.17 Women indicate that they desire to be actively involved in decision-making regarding medical testing related to breast health.18 However, research has shown that providers do not typically include women in decision-making about screening. Lack of time, language barriers, and lack of knowledge are cited as reasons for not discussing these issues.19 Patients report that they typically receive information on the benefits of mammography screening but rarely receive information regarding the harms.20
Clinicians need to assist patients in weighing the benefits and the potential harms of screening. Therefore, it is important to clarify advantages and disadvantages of screening options in order to support patients in the determination of best actions according to their individual risks and preferences. Health care professionals are expected to provide patients with clear information about all of their health issues in order to engage them in shared decision-making about their medical care.21 As primary care moves toward a patient-centered, interdisciplinary team model, nonphysician team members are often tasked with discussing and ordering screening tests.22 Therefore, the education of the entire health care team on current breast cancer screening guidelines and counseling methods is an important step in achieving success in this area.
The objectives of our study were as follows: 1) to assess the US Department of Veterans Affairs (VA) primary care providers’ and staffs’ reported practices regarding counseling women on potential benefits and harms of breast cancer screening and 2) to assess the impact of a brief educational intervention on VA providers’ and staffs’ knowledge, attitude, and comfort level regarding counseling on the pros and cons of breast cancer screening.
Methods
We used a quasiexperimental design with participant surveys conducted before and after an educational intervention. All surveys were anonymous. The educational intervention consisted of a 30-minute academic detailing session for all physicians and nursing staff in 13 community-based primary care VA clinics in the state of Alabama from June 2012 to September 2012. Participants were instructed on USPSTF guidelines, which are the standards mandated by the Veterans Health Administration.23 In addition, the benefits and harms of mammography screening,3,4,7,12 risk assessment tools,24,25 and counseling methods26 were discussed. The same speaker facilitated all sessions, and the same material was presented to each group. The speaker was a general internist with proficiency in providing care to women; in addition, she has 20 years of experience in education of medical students, physicians, and nursing staff.
Teaching sessions focused on USPSTF recommendations because providers in the VA primary care clinics (our study group) are expected to adhere to these guidelines.23 A poster summarizing these recommendations was given to each clinic for future reference (Figure S1).
In addition, material from the lecture was also made available for future access in the Clinician Guide: Discussing Breast Cancer Screening Decisions with Average Risk Women in Their 40s.26 This guide was developed by the National Center for Health Promotion and Disease Prevention, Office of Patient Care Services, Veterans Health Administration.
Pre- and post-training surveys were used to assess these outcomes: 1) knowledge of breast cancer screening guidelines; 2) counseling practices of benefits and risks of screening; and 3) comfort level in providing counseling about risks and benefits of screening. Paper surveys were administered immediately before and after each teaching session. The participants were not matched in pre- and post-training surveys.
To assess knowledge of breast cancer screening guidelines, participants were asked how they would address screening mammography for average risk women ages 40–49. Participants were asked to choose from these options: 1) recommend mammogram screening; 2) recommend waiting until age 50 to start mammogram screening; and 3) recommend screening on the basis of patient preference.
To assess counseling practices of benefits and risks, participants were asked “Do you typically inform your patients of the benefits of mammography screening?” and “Do you typically inform your patients of the risks or harms of mammogram screening?”. Participants responded yes or no to both of these questions.
Finally, we asked participants how comfortable they were in providing counseling regarding screening benefits and risks/harms and in discussing cancer risks and preferences with women ages 40–49 for shared decision-making. (There were three questions asked; patients responded by using the five-point Likert scale, for which 1= not comfortable and 5= very comfortable.)
An exemption was obtained from the Institutional Review Board. The Institutional Review Board at our facility did not require informed consent to participate because the risk was no greater than those ordinarily encountered in daily life. The intervention was deemed an educational quality improvement project. Quality improvement consists of actions that intend to improve health care services and the health status of targeted patient groups.
Statistical analysis
We used standard descriptive statistics. To compare responses given before the intervention with those given after the intervention, we used the chi-square test for categorical data and the Mann–Whitney U test for ordinal data (comfort level), as data were not normally distributed. To illustrate differences in ordinal data (comfort level), we have presented the results in box plots. We used a P<0.05 to assess statistical significance. We used Stata 11.2 for analysis (StataCorp LP, College Station, TX, USA).
Results
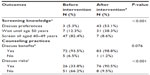
Thirteen outpatient VA clinics in Alabama received the educational intervention, which reached 87 out of a total of 121 staff members (physicians and nurses). There were 13 teaching sessions with an average of seven attendees at each session. A total of 165 surveys (78 before the intervention, 87 after the intervention) were received (nine participants did not complete the pretraining survey). The response rate was 90% for pretraining surveys and 100% for post-training surveys. Responders were registered nurses, licensed practical nurses, physicians, and nurse practitioners (Table 1).
Screening knowledge
Regarding the screening knowledge assessment, there were differences between the pre- and the post-intervention responses on breast cancer screening recommendations for 40–49 year old women. Before the intervention, 82.4% of participants reported that they would advise all women ages 40–49 to be screened; after the intervention, 8.6% of participants reported that they would give that advice. Before the intervention, 12.3% of participants reported that they would advise patients to wait until age 50 to be screened; that percentage increased to 38.3% after the intervention. The percentage of participants who said that they would discuss the patient’s preferences before making a screening decision increased from 5.3% before the intervention to 53.1% afterward. All differences were significant (P<0.001; Table 2).
Counseling practice
After the intervention, attitudes favoring discussion of risks of mammography increased from 33.8% to 90.5% (P<0.001). Attitudes favoring discussion of benefits of screening also trended upward from 93.5% to 98.8%; however, this was not statistically significant (P=0.076; Table 2).
Comfort level with counseling and with eliciting patient preferences
After the intervention, the comfort level with all aspects of counseling improved: benefits of screening (P<0.001); risks and harms of screening (P<0.001); and eliciting the screening preferences for women 40–49 (P<0.001). Figure 1 shows these relationships in the top, middle, and bottom panels, respectively.
Discussion
Our study shows that physicians and nursing staff (including registered nurses and licensed practical nurses) practicing in 13 community-based VA clinics in Alabama routinely provide counseling on the benefits of mammography screening but not on the potential harms of such screening. In order for women to make informed decisions regarding breast cancer screening, this information needs to be available to them. Although it has been several years since USPSTF recommended counseling women ages 40–49 about the risks and benefits of mammography screening, we found that few providers adhere to this recommendation in practice. This is consistent with prior data that change in behavior often lags behind more recent evidence and guidelines.27 Our study did not assess why providers do not discuss options with women. Previously reported reasons include disagreement with guidelines, lack of knowledge, and lack of time.28
After the educational intervention, those stating they would counsel women 40–49 increased from 5% to 53%. However, 38% indicated they would not offer screening, or even discuss screening options, until patients reach age 50. Likewise, 9% indicated they would continue to recommend screening for all 40-year old women. This may reflect the fact that there is controversy regarding screening recommendations with other groups continuing to recommend to start screening all women when they reach age 40.8–11
It has been demonstrated that VA medical facilities have greater compliance with breast cancer screening quality indicators than do non-VA hospitals.29 Our study took place in VA outpatient clinics that participate in a quality improvement system using computerized clinical reminders for preventive health. VA medical practitioners are likely to be influenced by prompts from these reminders. Some comments from our participants indicated that it was easier to order the mammogram and receive credit for the quality measure than to take additional steps to extend the reminder to age 50. This concern has also been voiced with regard to health policy in other countries. A publication from the UK calls for changing performance measures to assess informed choice rather than screening participation rates.30 VA performance measures have been updated to offer more options for women ages 40–49; these new criteria include documentation of a discussion of risks and benefits of screening.23 The Clinician Guide26, discussed previously, is also available to review during the completion of computerized quality reminders. Ongoing policy and clinical reminder development for nursing and allied health staff may be helpful in supporting primary care team members as they undertake an active role in counseling about preventive health.
Strengths of our study include our sample of primary care providers and staff from 13 VA community-based clinics. This provides a picture of nonacademic settings and allows for the assessment of the entire interdisciplinary team. Clinic staff, rather than the physician, often assist in completion of preventive health maintenance, and they may be the team members who actually provide the counseling and order the screening test.22 Hence, without involvement from the entire primary care team, efforts to accomplish counseling may be difficult. Therefore, clinic personnel need to be included in education around current guidelines, risk assessment, and counseling of patients.
There are limitations to our study. We did not compare the responses from particular staff members (physicians vs nonphysicians) or from different clinics. It is possible that some groups are more responsive to the intervention than are others, a variable which may allow for a change in approach in the future. In addition, our survey only assessed opinions and attitudes immediately after the intervention; we do not know if this will affect future clinical practice or if the change in attitudes and knowledge is sustainable. Future research will be needed to determine if actual practice patterns are influenced.
We found that most health care professionals’ opinions about counseling changed after receiving a brief educational intervention with information on guidelines and counseling methods. Our participants indicated that in the future they plan to counsel women in their 40s about their options for screening. This suggests that lack of awareness of screening guidelines and lack of knowledge regarding counseling techniques may be reasons why many providers do not offer this counseling. Therefore, academic sessions may be valuable for equipping clinicians with knowledge to enhance preventive services.
A combination of education, technology, and staff support is probably needed to increase the availability of counseling on screening options for women. A recent meta-analysis summarizes suggestions for evidence-based discussion points that are similar to our academic detailing for informed decision-making about mammography screening.31 Likewise, a recent editorial by Esserman and O’Kane suggests that screening should be further refined by improved risk assessment and adjustment of biopsy thresholds; therefore, the standard guidelines should move away from “one size fits all” screening.32 This more patient-centered approach will mean having more involved discussions with women about their options, but further research is needed to better understand whether these discussions affect outcomes.
Conclusion
Physicians and nursing staff in 13 outpatient VA primary care clinics in Alabama routinely discuss mammography benefits but not potential harms with women ages 40–49 prior to screening. An educational intervention detailing current breast cancer screening recommendations and counseling methods for this age group affected providers’ knowledge and attitudes toward screening. Hence, the delivery of patient-centered care may be enhanced by the education of the entire primary care team.
Acknowledgment
This project was funded by the Women’s Health Education Innovation Grant 2012, awarded by the Veterans Health Strategic Health Care Group.
Disclosure
The authors report no conflicts of interest in this work. The opinions expressed in this article are those of the authors alone and do not reflect the views of the US Department of Veterans Affairs, the University of Alabama in Birmingham, or the University of Central Florida College of Medicine.
References
SEER Cancer Statistics Review, 1975–2010 [webpage on Internet]. Bethesda: National Cancer Institute; 2012 [cited April 2013]. Available from: http://seer.cancer.gov/csr/1975_2010/. Accessed July 20, 2014. | |
Ferlay J, Soerjomataram I, Ervik M, et al. GLOBOCAN 2012 v1.0, Cancer Incidence and Mortality Worldwide: IARC CancerBase No. 11 [Internet]. Lyon, France: International Agency for Research on Cancer; 2013. Available from: http://globocan.iarc.fr/pages/fact_sheets_population.aspx. Accessed March 23, 2015. | |
Welch HG, Passow HJ. Quantifying the benefits and harms of screening mammography. JAMA Intern Med. 2014; 174(3):448–453. | |
Nelson HD, Tyne K, Nalik A, et al. Screening for breast cancer: an update for the US Preventive Services Task Force. Ann Intern Med. 2009;151(10):727–737. | |
Barratt A, Howard K, Irwig L, Salkeld G, Houssami N. Model of outcomes of screening mammography: Information to support informed choices. BMJ. 2005;330(7497):936. | |
Salzmann P, Kerlikowske K, Phillips K. Cost-effectiveness of extending screening mammography guidelines to include women 40 to 49 years of age. Ann Intern Med. 1997;127(11):955–965. | |
Kalager M, Adami HO, Bretthauer M, Tamimi RM. Overdiagnosis of invasive breast cancer due to mammogram screening: results from the Norwegian screening program. Ann Intern Med. 2012;156(7):491–499. | |
Smith RA, Manassaram-Baptiste D, Brooks D, et al. Cancer Screening in the United States, 2014: A review of current American Cancer Society Guidelines and current issues in cancer screening. CA Cancer J Clin. 2014;64(1):30–51. | |
Lee CH, Dershaw DD, Kopans D, et al. Breast cancer screening with imaging: Recommendations from the Society of Breast Imaging and the ACR on the use of mammography, breast MRI, breast ultrasound, and other technologies for the detection of clinically occult breast cancer. J Am Coll Radiol. 2010;7(1):18–27. | |
Bevers TB, Anderson BO, Bonaccio E, et al. NCCN clinical practice guidelines in oncology: breast cancer screening and diagnosis. J Natl Compr Canc Netw. 2009;7(10):1060–1096. | |
American College of Obstetricians-Gynecologists. Practice bulletin no 122: Breast cancer screening. Obstet Gynecol. 2011;118(2 Pt 1):372–382. | |
Nelson HD, Tyne K, Naik A, Bougatsos C, Chan BK, Humphrey L; US Preventive Services Task Force. Screening for breast cancer: an update for the US Preventive Services Task Force. Ann Intern Med. 2009;151(10):727–737, W237–W242. | |
Qaseem A, Snow V, Sherif K, Aronson M, Weis KB, Owens DK. Screening mammography for women 40 to 49 years of age: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2007;146(7):511–515. | |
Canadian Task Force on Preventive Health Care; Tonelli M, Connor Gorber S, Joffres M, et al. Recommendations of screening for breast cancer in average-risk women aged 40–74 years. CMAJ. 2011; 183(17):1991–2001. | |
Advisory Committee on Cancer Prevention. Recommendations on cancer screening in the European Union. Advisory Committee on Cancer Prevention. Eur J Cancer. 2000;36(12):1473–1478. | |
World Health Organization. WHO Position Paper on Mammography Screening. Geneva: World Health Organization; 2014. Available from: http://apps.who.int/iris/bitstream/10665/137339/1/9789241507936_eng.pdf?ua=1. Accessed February 7, 2015. | |
Pace LE, He Y, Keating NL. Trends in mammography screening rates after publication of the 2009 US Preventive Services Task Force recommendations. Cancer. 2013;119(14):2518–2523. | |
Davey HM, Barratt AL, Davey E, et al. Medical tests: women’s reported and preferred decision-making roles and preferences for information on benefits, side-effects and false results. Health Expect. 2002;5(4):330–340. | |
Dunn AS, Shridharani KV, Lou W, Bernstein J, Horowitz CR. Physician-patient discussions of controversial cancer screening tests. Am J Prev Med. 2001;20(2):130–134. | |
Zikmund-Fisher BJ, Couper MP, Singer E, et al. Deficits and variations in patients’ experience with making 9 common medical decisions: the DECISIONS survey. Med Decis Making. 2010;30(5 Suppl):85S–95S. | |
Coulter A, Parsons S, Askham J. Policy Brief: Where are the Patients in Decision-Making About Their Own Care? Copenhagen: World Health Organization Regional Office for Europe; 2008. Available from: http://apps.who.int/iris/bitstream/10665/107980/1/E93419.pdf?ua=1. Accessed February 7, 2015. | |
Department of Veterans Affairs, Veterans Health Administration. VHA Handbook 1101.10. Patient Aligned Care Team (PACT) Handbook. Washington, DC: Veterans Health Administration; 2014. Available from: http://www1.va.gov/vhapublications/ViewPublication.asp?pub_ID=2977. Accessed December 24, 2014. | |
Veteran’s Hospital Administration. VHA National Center for Health Promotion and Disease Prevention: Screening for Breast Cancer. Washington, DC: Veterans Health Administration; 2014. Available from the Veteran’s Administration Intranet. Accessed December 24, 2014. | |
van Ravesteyn NT, Miglioretti DL, Stout NK, et al. Tipping the balance of benefits and harms to favor screening mammography starting at age 40 years: a comparative modeling study of risk. Ann Intern Med. 2012;156(9):609–617. | |
Nelson HD, Zakher B, Cantor A, et al. Risk factors for breast cancer for women aged 40 to 49 years: a systematic review and meta-analysis. Ann Intern Med. 2012;156(9):635–648. | |
National Center for Health Promotion and Disease Prevention, Office of Patient Care Services, Veterans Health Administration. Clinician Guide: Discussing Breast Cancer Screening Decisions with Average Risk Women in Their 40’s. Washington, DC: Veterans Health Administration; 2011. Available from: http://www.prevention.va.gov/docs/VANCP_BreastCancerFact.pdf. Accessed December 24, 2014. | |
Berwick DM. Disseminating innovations in health care. JAMA. 2003;289(15):1969–1975. | |
Cabana MD, Rand CS, Powe NR, et al. Why don’t physicians follow clinical practice guidelines? A framework for improvement. JAMA. 1999;282(15):1458–1465. | |
Prevention – Breast Cancer Screening [webpage on Internet]. Washington, DC: US Department of Veterans Affairs; 2012. Available from: http://www.va.gov/QUALITYOFCARE/initiatives/compare/prevention-breast-cancer-screening.asp. Accessed December 24, 2014. | |
Strech D. Participation rate or informed choice? Rethinking the European key performance indicators for mammography screening. Health Policy. 2014;115(1):100–103. | |
Pace LE, Keating NL. A systematic assessment of benefits and risks to guide breast cancer screening decisions. JAMA. 2014;311(13):1327–1335. | |
Esserman L, O’Kane ME. Moving beyond the breast cancer screening debate. J Women’s Health (Larchmt). 2014;23(8):629–630. |
Supplementary material
References
van Ravesteyn NT, Miglioretti DL, Stout NK, et al. Tipping the balance of benefits and harms to favor screening mammography starting at age 40 years: a comparative modeling study of risk. Ann Intern Med. 2012;156(9):609–617. | |
Kalager M, Adami HO, Bretthauer M, Tamimi RM. Overdiagnosis of invasive breast cancer due to mammogram screening: results from the Norwegian screening program. Ann Intern Med. 2012;156(7):491–499. | |
Veteran’s Hospital Administration. VHA National Center for Health Promotion and Disease Prevention: Screening for Breast Cancer. Washington, DC: Veterans Health Administration; 2014. Available from the Veteran’s Administration Intranet. Accessed December 24, 2014. | |
Breast Cancer Risk Assessment Tool. National Cancer Institute at the National Institutes of Health. Last updated 5/16/2011. Available from: http://www.cancer.gov/bcrisktool/. Accessed March 23, 2015. | |
National Center for Health Promotion and Disease Prevention, Office of Patient Care Services, Veterans Health Administration. Clinician Guide: Discussing Breast Cancer Screening Decisions with Average Risk Women in Their 40’s. Washington, DC: Veterans Health Administration; 2011. Available from: http://www.prevention.va.gov/docs/VANCP_BreastCancerFact.pdf. Accessed December 24, 2014. | |
Breast Cancer Screening (PDQ®). National Cancer Institute at the National Institutes of Health. Last updated November 24, 2014. Available from: http://www.cancer.gov/cancertopics/pdq/screening/breast/patient. Accessed March 23, 2014. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.