Back to Journals » Patient Related Outcome Measures » Volume 6
How do disease perception, treatment features, and dermatologist–patient relationship impact on patients assuming topical treatment? An Italian survey
Authors Burroni AG, Fassino M, Torti A, Visentin E
Received 28 October 2014
Accepted for publication 18 December 2014
Published 16 February 2015 Volume 2015:6 Pages 9—17
DOI https://doi.org/10.2147/PROM.S76551
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Robert Howland
Anna Graziella Burroni,1 Mariella Fassino,2 Antonio Torti,3 Elena Visentin4
1IRCCS University Hospital San Martino, IST National Institute for Cancer Research, Genoa, Italy; 2Department of Psychology, Specialization School in Clinical Psychology, University of Turin, Turin, Italy; 3Dermatology practice, Milan, Italy; 4HTA and Scientific Support, CSD Medical Research Srl, Milan, Italy
Background: Psoriasis largely affects daily activities and social interactions and has a strong impact on patients’ quality of life. Psoriatic patients have different attitudes toward their condition. Topical medications are essential for the treatment of psoriasis, but the majority of patients do not adhere to these therapies.
Objective: The history of treatment success or failure seems to influence patient attitude toward topical therapy. Therefore, it is important to understand the psychological, experiential, and motivational aspects that could be critical for treatment adherence, and to describe the different attitudes toward topical treatment. Furthermore, the physician–patient relationship and the willingness to trust the dermatologist may have a substantial role in encouraging or discouraging patients’ attitudes toward topical therapy.
Methods: A survey was designed to collect aspects that could be relevant to understanding different patient attitudes toward psoriasis and its treatments. A total of 495 self-administered questionnaires compiled by psoriatic patients were analyzed from 20 Italian specialized hospital centers in order to provide a nationwide picture.
Results: Psoriatic patients have different perceptions and experiences in relation to their condition: half of them consider psoriasis as a disease, while the other half consider psoriasis as a disorder or a nuisance. Topical therapy is the most widely used treatment, even though it is not considered the most effective one and often perceived to be cosmetic. The main findings are: 1) inadequate patient education about this disease, 2) lack of information about topical treatment, and 3) lack of results within the expected time frame. Furthermore, physicians need to build a good relationship with psoriatic patients in order to motivate them, to trust in their care, and to adhere to treatment.
Conclusion: This survey adds new and important details about daily life and well-being and the needs of psoriatic patients, providing suggestions for dermatologists to improve patients management.
Keywords: psoriasis, topical therapy, survey, dermatologist
Background
Psoriasis has an estimated prevalence in Italy of 2.1% in children and of 2.9% in adults. Its incidence in Italian adults is 230/100,000 person-years.1 Visible dermatological conditions, such as psoriasis, even when not clinically severe or during periods of remission, may have a substantial psychosocial impact on patients’ lives2 as it largely affects daily activities and social interactions, ultimately reflecting on patients’ quality of life (QoL).3 Social stigmatization and rejection are commonly experienced by patients with psoriasis with a consequent profound effect on self-confidence, self-image, and sense of well-being.4 It is not only the number and spread of the body surface areas affected by psoriasis that reflect on the way in which patients perceive and react to their health status, but also the visibility of affected areas. Patients with psoriasis can live and cope with their disease quite differently; some report feelings of embarrassment and shame, while others show a state of anger when compared with healthy controls.5
Topical treatments are essential for psoriasis, but the majority of patients do not seem to recognize their usefulness and do not adhere to treatment. Indeed, only 35%–72% of the recommended dose is used during a treatment period ranging from 14 days to 8 weeks.6
There is a continuous need to understand which variables can explain and/or predict patients’ attitudes toward topical therapy, in order to deliver practical recommendations/interventions for improving the patient’s adherence and, therefore, ways to improve treatment efficacy.
When assessing patients’ perception toward topical treatment, specific aspects should be considered, such as the cosmetic and galenic properties of the formulation, and particularly of the vehicle (very greasy, desiccating, or sticky vehicles), the smell of the preparation, the time required for its application, in addition to the convenience, easiness, and pleasantness of its use. Other more general factors are associated with psoriasis treatment, ie, the history of its therapeutic success or failure. Patient dissatisfaction with efficacy leads to frustration, a feeling that is further influenced by the chronic nature of the disease.6–8 In addition, the physician–patient relationship and the willingness to trust the dermatologist may contribute to the level of adherence to therapy.9,10 Patients with psoriasis do not seem to interact enough with their physicians and discuss topical treatment. Moreover, insufficient information about the disease and its management, unclear or complex instructions, and loss or omission of instructions may contribute to nonadherence to topical treatment.
The purpose of this survey was to investigate the patient’s perception of the disease, his/her appraisal of the topical treatment, and his/her relationship with the dermatologist in order to understand how these aspects may affect daily life and well-being and the needs of psoriatic patients.
Methods
A self-administered questionnaire was designed on the basis of the Italian Society of Psychosomatic Dermatology (SIDEP Società Italiana di Dermatologia Psicosomatica) guidelines, on systematic literature review, and qualitative patient-focus interviews. Psychologists and experts in pharmaceutical market research conducted the qualitative interviews on two psoriatic patients to adjust the questionnaire and verify that all significant variables were taken into account. The resulting questionnaire was evaluated by a panel of experts from the SIDEP members during an “ad hoc” meeting.
The final questionnaire investigated the following main aspects:
- Socio-demographic information: sex, age, time since diagnosis, education level, and occupational status.
- General disease: patients were asked to define psoriasis, to assess the severity of the disease, and to specify the body areas involved.
- Related feelings: patients were asked to describe their feelings at the moment of the diagnosis of psoriasis, the discomfort (both experienced and anticipated) due to psoriasis in different body parts, the influence of psoriasis in everyday life.
- Treatments used: patients were asked to describe the types of treatment and therapy used in the past, to give their opinion about therapy features (by means of emoticons), to describe the therapeutic management, and to indicate the time period in which they expect the treatment benefit.
- Relationship with the physician: patients were asked to describe their assessment of their dermatologists and the number of dermatologists visited, and the factors influencing their decision to change their dermatologist.
- Information about psoriasis: source and type of information retrieved.
The questionnaire included the use of multiple choice answers, numerical and categorical scales, and open questions. Furthermore, emoticons were used to graphically represent feelings/features perceived by the patients with respect to the various formulations used in topical therapy (ie, comfortable, protective, greasy, etc).
Descriptive statistics were compiled. The mean and percentage range are reported along with the actual range (minimum and maximum scores).
Results
Questionnaire and survey
The survey was completed by 504 patients attending 20 Italian hospital centers specialized in psoriasis between June and December 2013. Nine out of 504 questionnaires were excluded from the analysis because they were only partially completed. It should be noted that since patients were recruited in specialized centers, their psoriasis is likely to be at least moderate in severity.
Socio-demographic results
Of the respondents, 57% were men; their mean age was 52.6 years (66% of patients were between 40 and 70 years of age). The panel included patients from a wide range of educational and working levels, and so represented a good cross-section of the psoriasis population. The mean time from diagnosis to interview was 19.6 years, which indicates inclusion of chronically ill patients.
Figure 1 reports the distribution of lapsed time from diagnosis to survey.
  | Figure 1 Patients’ distribution by time from diagnosis to survey. |
Perception of the disease
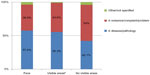
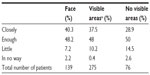
The majority of respondents (54%) perceived their illness as either a disease or a pathology as compared with 44% of respondents who considered psoriasis as a nonpathological condition (nuisance, complaint, inconvenience, or problem) (Figure 2). There is a clear correlation between the visibility of the areas affected and the perception of the illness: as shown in Figure 3, patients affected on the face and other visible areas (hands, nails, arms) perceived their illness mainly as a disease/pathology (57.6% and 55.3%, respectively) in comparison with patients not affected in visible areas (42.1%). Regarding disease severity, more than half of the patients (56%) assessed their disease as moderate and only 27% as severe.
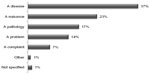  | Figure 2 Results to the question “How would you define psoriasis?” |
The perception of the disease’s severity is strictly related to the number of body surface areas affected: most patients being affected in eight or more areas perceive their psoriasis as severe. Again, results show a relationship between the visibility of the affected areas and the perception of the severity of psoriasis: when psoriasis involves the face, which occurs in approximately 28% of patients, the severity perceived is greater.
Figure 4 indicates the level of discomfort (on a rating scale from 1 to 10) perceived by patients, depending on the area involved by psoriasis; the highest scores are associated with highly exposed body parts (face, hands, scalp) or genitals, while less discomfort is attributed to other parts with lower visibility.
Treatments used
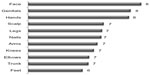
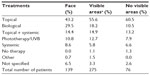
Topical therapy is the most widely used treatment, followed by biological therapy and phototherapy (Figure 5). Almost 6% of patients reported the use of systemic therapy only, whereas 15% reported the use of combined systemic and topical therapy. Biological therapy is used mostly by patients affected on the face or other visible areas (29.5% and 18.2%, respectively), whereas 60% of patients not affected on visible areas reported they use topical therapy only (Table 1).
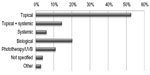  | Figure 5 Results of the question “What kind of treatment are you currently taking?” |
The majority of patients have used more than one therapy for psoriasis: 74% reported they had used other therapies with a mean number of 3.4 topical medications – in the past.
Topical therapy
Patients were asked to focus on a topical psoriasis product, and to indicate whether they considered it to be a medication or an emollient; 69% of patients chose the first possibility, while 29% chose the second. Data also revealed that patients who considered psoriasis to be a disease also considered topical products as medication, and even if topical products were not considered to be effective for most patients, 49% of them declared they always carry a topical product for use whenever needed. Also, this last result is strictly related to the visibility of the areas affected by psoriasis: 59.7% of patients affected on the face declared they always carry with them a topical product compared with 31.6% of those not affected on visible areas (Figure 6).
The preferred formulation appears to be cream, as it is assessed as comfortable, practical, and easy to apply (Figure 7).
The main reasons leading to interruption of topical therapy are: absence of improvement in the expected time frame, inconvenience of the daily applications, and discovery of a better product (Table 2). There is no correlation between the visibility of the affected areas and the reasons for nonadherence to topical therapy.
  | Table 2 Answers to the question “Thinking about various reasons that has led to discontinuing a topical treatment, indicating the weight of each reason listed” |
The majority of respondents declared they adhere closely to the instructions given with regard to the method of application of the topical therapy and reported benefit from free samples provided by their doctor. The dermatologist’s recommendations are followed closely mainly by patients affected on the face and other visible areas when compared with patients not affected on visible areas (40.3% and 37.5% versus 28.9%, respectively) (Table 3).
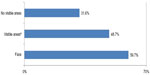
Of the respondents, 67% expected to notice treatment results within 2 weeks of usage, while 42% expected results within 1 week (Figure 8).
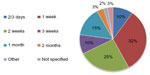  | Figure 8 Results to the question “How soon after initiation of therapy do you expect to see results?” |
Emollients’ features
The most appreciated features of topical therapy are: “Soothing” and “Reliable”, while the features that are less appreciated are: “Greased”, “Bedaubing”, and “Sticky”, as displayed in Figures 9 and 10 by emoticons.
  | Figure 9 Results to the question “Which feature of local products do you think are the most appreciated?” |
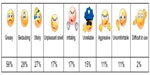  | Figure 10 Results to the question “Which effects of local products do you think are the most unpleasant?” |
When asked to rate the characteristics considered to be important for a topical treatment, the majority of responders attributed a high score to the items “It calms the itching” (9.1 points in a rating scale of 1–10, with 76% reporting a value of 9 or 10) and “Does not irritate the skin” (9.1 points, 75% reported a value of 9 or 10); also, the dermatologist’s recommendations are highly rated (9.1 points, 72% of patients reported a value of 9 or 10), which implies a good patient–doctor relationship and trust. The statement about the cost of the product: “It does not have an excessive cost” received an average rating of 8.4 points (62% of patients reported a value of 9 or 10).
Relationship with the physician
Patients reported that between the diagnosis and this survey, they have changed dermatologists by a mean of 4.2 times and have declared themselves satisfied with the help received from their clinicians in the management of psoriasis; the mean satisfaction is 7.9 points on a rating scale of 1 (no satisfaction) to 10 (extremely satisfied). The efficacy of the treatment prescribed (9) and the trust placed in the treatment by the dermatologist (8.7) and in his expertise (9) were considered to be the most important factors in establishing a positive relationship with the physician.
However, the most frequent reasons assigned for changing dermatologists were mainly the lack of efficacy of the prescribed treatment (43%) and lack of confidence in the physician (15%).
Discussion
Qualitative research has received increasing attention and importance in the medical field because it gives a deeper insight into the patient’s appraisal of aspects that cannot be measured, such as subjective illness perception.10 This survey adds new and important details about daily life and well-being and the needs of psoriatic patients.
An important outcome of this survey is the different patient perceptions related to psoriasis: only half of them consider psoriasis to be a disease, while the other half consider it to be a disorder or nuisance. The perceived severity of psoriasis, as the perception of the illness, appears to depend not only upon the number of affected areas but also, and especially, upon visibility. Discomfort is demonstrated to be greater if the areas affected are the face, hands, or genitals, ie, visible or “relational” areas. In this patient population, topical therapy is the most widely used, even though it is not considered the most effective one. However, half of the patients always carry a topical product to be used “in case of need” (eg, when traveling). Patients affected on the face or other visible areas (hands, arms, nails) are more aware of their condition, often declaring they always bring with them a topical product to use as needed and follow closely the recommendations of their dermatologist. This survey included patients’ assessment of expected characteristics of topical products, such as soothing. Results indicate that topical products are expected to provide skin well-being and reduction of itching, in addition to reliability, as skin diseases are perceived to be due to improper use of topical products. Indeed, results related to the evaluation of topical products indicate that more than three-quarters of patients attributed a rating score of 9 or 10 to the item “It calms the itching” and almost two-thirds of patients reported a rating score of 9 or 10 for the item “Does not irritate the skin,” reflecting the fear of possible side effects from inappropriate product usage, an issue particularly felt by psoriatic patients.11,12
The main cause of nonadherence to topical therapy is lack of results: however, 67% of patients expect an improvement within 2 weeks of treatment, even if this period is considered too short to be effective.
Generally, patients expressed satisfaction with their relationship with their dermatologist and reported that the main reason for changing dermatologists was the absence of the expected treatment effect. Nevertheless, the efficacy of the prescribed treatment, the expertise of the dermatologist, and the trust between patient and physician are the most important factors for a positive physician–patient relationship.
The principal findings highlighted by this survey are: 1) the inadequate patient education about this disease (44% of patients considered psoriasis a nonpathological disease), 2) the lack of topical treatment information (when asked to focus on a topical treatment, one out of three patients thought of a simple cosmetic product), and 3) the unrealistic expected time to treatment efficacy (67% of patients expect treatment results within a few weeks). For these reasons, dermatologists should keep in mind that informing patients on all these aspects could lead to a better awareness of the disease with greater patient benefits. Nonetheless, patients declare their adherence to the prescribed instructions of topical application and express the need for a fair product price. Pouplard et al13 showed that almost two-thirds of topical prescriptions are not adequately written and do not include the required information to improve adherence, while Brown et al12 found that 18% of the subjects surveyed reported “high treatment cost” as the reason for poor therapy adherence.
It is of utmost importance that physicians build a good relationship with psoriatic patients, focusing on communication and education, and that they gain confidence and make them feel more satisfied and trust in their care and, consequently, more optimistic and motivated to adhere to treatment.14–16
A good relationship should be based on frequent follow-up visits. Sedona et al9 demonstrated a positive correlation between adherence level and frequency of follow-up visits. Therefore, physicians who wish to optimize patients’ adherence to treatment could increase the frequency of visits, particularly in the early stages of treatment.
In a qualitative study performed by Kjellgren et al,17 authors confirmed the importance of enhanced communication skills among the providers, together with individualized dermatology patient education and continuous treatment support. All personnel involved in the management of psoriatic patients (ie, dermatologists, dermatology nurses, and pharmacists) should strictly cooperate in order to form an effective treatment support network.18
A possible limitation of this survey is the fact that it was restricted to patients attending the hospital centers specialized in psoriasis. Therefore, patients interviewed can have a more severe pathology and a greater consciousness of their disease compared with subjects with a mild or moderate psoriasis, who may have different perceptions of their disease, different attitudes concerning their relationship with their dermatologist, and who are possibly even less adherent to therapy. A possible evidence of this bias in population selection could be the preferred source of information; the majority of respondents stated that the dermatologist is their most important source of information: this result cannot be reasonably generalized to include psoriatic patients not attending a specialized center.
Conclusion
The results of this survey provide a reminder to physicians on the key points that they should seek to address during the management of their psoriatic patients. When prescribing topical treatments, physicians should educate patients about the nature of their disease and encourage them to use medications correctly and consistently with clear and simple instructions, in order to obtain an effective and stable disease control.8,9 It is also important to inform patients about the minimum treatment duration needed to obtain favorable results and to provide realistic expectations about effectiveness and safety. These efforts may lead to improved management of psoriatic patients, as well as promoting adherence to treatment, and a positive physician–patient relationship.
Acknowledgments
The authors would like to thank all clinicians who collaborated in the survey: E Maiani, IFO Rome; A Manzotta, San Camillo Hospital Rome; M Fantini, Manzoni Hospital Lecco; M Morri, Rimini Hospital; A Richetta, Policlinico Umberto I Rome; P Di Russo, Sant’Andrea Hospital Rome; MT Corradin, Pordenone Hospital; M Donini, Venezia Hospital; S Di Nuzzo, Clinic of Padova; MU Marconi, San Paolo Hospital Milan; F Musumeci, Salerno Hospital; F Cusano, Benevento Hospital; G Bagnoni, L Livorno Hospital; L Brandini, Flucecchio Hospital; F Laconsole, Clinical of Bari; A Altobella, Ospedali Riuniti Lecce; G Pistone, Clinical of Palermo; ML Musumeci, Clinical of Catania; G Roncarolo, Asti Hospital; A Zanca, Mantova Hospital.
Disclosure
This research was supported by an unrestricted grant from Pierre Fabre SpA. CSD Italy Srl was responsible for questionnaire writing, data entry, data analysis, and data interpretation. CSD Medical Research Srl was responsible for medical writing and editorial assistance. Anna Graziella Burroni is a consultant for Abbvie Srl. Antonio Torti is a consultant for Pierre Fabre SpA. Elena Visentin is an employee of CSD Medical Research Srl and follows projects for Novartis, Lundbeck, Bayer, Otsuka, and Pierre Fabre. The authors declare no other conflicts of interest.
References
Parisi R, Symmons DPM, Griffiths CEM, Ashcroft DM; On behalf of the Identification and Management of Psoriasis and Associated ComorbidiTy (IMPACT) project team. Global epidemiology of psoriasis: a systematic review of incidence and prevalence. J Invest Dermat. 2013;133:377–385. | |
Sampogna F, Tabolli S, Abeni D, et al. Living with psoriasis: prevalence of shame, anger, worry, and problems in daily activities and social life. Acta Derm Venereol. 2012;92:299–303. | |
Colombo D, Perego R. Quality of life in psoriasis. In: Hermenio L, editor. Psoriasis – Types, Causes and Medication. Croatia, Europe: InTech Publisher; 2013. | |
Kimball AB, Gieler U, Linder D, et al. Psoriasis: is the impairment to a patient’s life cumulative? J Eur Acad Dermatol Venereol. 2010;24: 989–1004. | |
Weiss SC, Kimball AB, Liewehr DJ, Blauvelt A, Turner ML, Emanuel EJ. Quantifying the harmful effect of psoriasis on health-related quality of life. J Am Acad Dermatol. 2002;47:512–518. | |
Devaux A, Castela E, Archier E. Adherence to topical treatment in psoriasis: a systematic literature review. J Eur Acad Dermatol Venereol. 2012;26(Suppl 3):61–67. | |
Zschocke I, Mrowietz U, Lotzin A. Assessing adherence factors in patients under topical treatment: development of the Topical Therapy Adherence Questionnaire (TTAQ). Arch Dermatol Res. 2014;306: 287–297. | |
Reich K, Bewley A. What is new in topical therapy for psoriasis? J Eur Acad Dermatol Venereol. 2011;25(Suppl 4):15–20. | |
Sedona P, De Pità O, Ricciuti E. Adherence in topical treatments for psoriasis Consensus paper. Dermatol Exp. 2013;15:143–151. | |
Weiss M, Weisshaar W. Qualitative interviews on chronic pruritus in haemodialysis patients. Acta Derm Venereol. 2014;94(6):713–714. | |
Fouere S, Adjadj L, Pawin H. How patients experience psoriasis: results from a European survey. J Eur Acad Dermatol Venereol. 2005;19(Suppl 3):2–6. | |
Brown KK, Rehmus WE, Kimball AB. Determining the relative importance of patient motivations for nonadherence to topical corticosteroid therapy in psoriasis. J Am Acad Dermatol. 2006;55:607–613. | |
Pouplard C, Gourraud P-A, Meyer N, et al. Are we giving patients enough information on how to use topical treatments? Analysis of 767 prescriptions in psoriasis. Br J Dermatol. 2011;165:1332–1336. | |
Serup J, Lindblad AK, Maroti M, et al. To follow or not to follow dermatological treatment – a review of the literature. Acta Derm Venereol. 2006;86:193–197. | |
Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;4:353. | |
Uhlenhake EE, Kurkowski D, Feldman SR. Conversations on psoriasis – what patients want and what physicians can provide: a qualitative look at patient and physician expectations. J Dermatolog Treat. 2010;21:6–12. | |
Kjellgren K, Ring L, Kettis Lindblad Å, Maroti M, Serup J. To follow dermatological treatment regimens – patients’ and providers’ views. Acta Derm Venereol. 2004;84:445–450. | |
Kettis Lindblad Å, Kjellgren KI, Ring L, Maroti M, Serup J. The role of dermatologists, nurses and pharmacists in chronic dermatological treatment: patient and provider views and experiences. Acta Derm Venereol. 2006;86:202–208. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.